Positron emission tomography (PET) is finding a new home in one of the most exciting corners of preclinical science: organ-on-a-chip platforms. Instead of imaging only animals or patients, researchers are now bringing PET right up to, and in some cases directly onto, microfluidic chips that mimic human organs and multi-organ systems.
This shift is more than a technical curiosity. It promises a tighter bridge between in vitro models and in vivo PET, better prediction of human drug behaviour, and smarter development of radiotracers and radiotherapeutics. In this article, we will examine how PET is being integrated into organ-on-a-chip systems, the latest hardware and application developments, and where the field appears to be heading.
Why PET and organ-on-a-chip belong together
Organ-on-a-chip (OoC) technology combines microfluidics, engineered scaffolds and living cells to recreate aspects of organ function in a small device. These chips can reproduce features such as shear stress, 3D architecture and multi-cellular interactions that are difficult to achieve in conventional culture plates. The long-term aim is to generate human-relevant data on pharmacokinetics (PK), efficacy, and toxicity while reducing reliance on animal models.
PET adds an attractive layer on top of this. Radiotracers and radiolabelled drugs can be quantified in real time with extremely high sensitivity, often down to the picomole level. Because many PET tracers are already used in animal and human studies, the same molecule can be applied across the in vitro–in vivo–clinical continuum.
For organ-on-a-chip systems specifically, PET offers several advantages:
- It gives non-destructive readouts, allowing repeated measurements over many hours without disrupting the chip.
- It yields dynamic information, so uptake, wash-in, washout and metabolism can all be tracked.
- It supports direct comparison with animal and human PET when the same tracer and kinetic models are used.
The last point is especially important for regulators and industry, who are looking for ways to connect innovative in vitro platforms to familiar in vivo endpoints.
From whole-body scanners to chip-scale PET
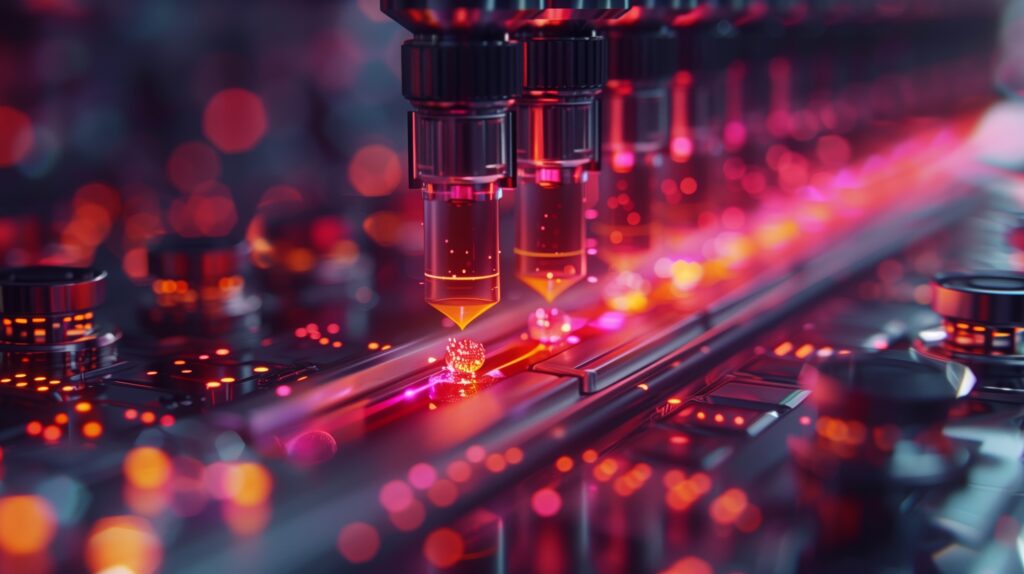
Conventional small-animal PET scanners are optimised for mice and rats, not for devices only a few centimetres across. This has led to the development of PET systems tailored to organ-on-a-chip and related microfluidic devices.
Recent work has described the design of dedicated “on-chip PET” systems with small fields of view and detector geometries arranged around microfluidic chips. These systems trade whole-body coverage for very high spatial resolution and sensitivity in a limited region, allowing sub-millimetre imaging of tiny tissue constructs under realistic culture conditions.
One concept study detailed a compact scanner built around an incubator-compatible chamber, so chips can be kept at physiological temperature and CO₂ levels while being imaged. Detector modules are placed as close as possible to the chip to maximise sensitivity. The group also explored how to handle low activity levels typical of microfluidic devices, testing reconstruction algorithms tuned for sparse data.
Another line of work has focused on mini-panel PET systems mounted underneath or alongside microfluidic platforms. These panels can image multiple samples in parallel, which is particularly useful for screening radiotracers or drugs across different cell lines or chip architectures within a single experiment.
These hardware developments reflect a general trend in PET towards dedicated scanners for specific organs or applications – breast, brain, prostate and now microfluidic chips – rather than relying solely on large, general-purpose systems.
Tumour-on-a-chip and radionuclide imaging
Cancer research is one of the earliest beneficiaries of this convergence. Tumour-on-a-chip models can recreate complex features, such as gradients in oxygen and nutrients, stromal interactions, and dynamic drug exposure, that are difficult to reproduce in 2D culture. Adding PET or high-resolution radionuclide imaging provides a means to examine how tracers and radiotherapeutics behave in more realistic tumour microenvironments.
Recent studies have used lung tumour-on-a-chip platforms with embedded radionuclide imaging capabilities to examine how radiolabelled compounds distribute through tumour tissue and associated vasculature over time. This includes assessing the binding of diagnostic tracers to their molecular targets and following the retention and efflux of therapeutic radionuclides.
Such models are particularly useful for theranostics – paired diagnostic and therapeutic radiopharmaceuticals that target the same molecule. On-chip PET or gamma imaging can help optimise dosing schedules, study combination treatments (for example, with immunotherapy) and explore resistance mechanisms long before a therapy reaches animal models or patients.
Body-on-a-chip with PET: towards systemic pharmacokinetics in vitro
Single-organ chips are powerful, but many safety and efficacy questions depend on how a drug moves through the whole body. A growing number of projects aim to construct multi-organ or “body-on-a-chip” systems, where multiple organ compartments – such as liver, kidney, gut and tumour – are linked by microfluidic channels that mimic blood flow.
In the UK, researchers have used 3D-printed body-on-a-chip devices populated with different cell types and perfused with radiolabelled drugs. PET imaging of these systems allows the team to monitor how the compound partitions between organ compartments over time, effectively creating an in vitro pharmacokinetic curve for each organ surrogate.
A related project combines such body-on-a-chip platforms with biomimetic chromatography and then cross-validates the results against PET/CT data from in vivo studies. The goal is to generate a rich, multi-scale dataset that can be used to train in silico models for predicting human drug distribution and target engagement, forming part of an integrated new approach methodologies (NAMs) toolbox for regulatory science.
In this setting, PET is not just another imaging modality; it is the anchor for linking chip data to animal and human data on an equivalent quantitative footing.
Micro- and nano-scale radionuclide imaging for organoids and chips
The line between organ-on-a-chip, organoids and micro-tissues is becoming increasingly blurred. Many technical advances in radionuclide imaging at small scales can be applied across all three.
One striking development is optical positron emission microscopy (oPEM). This technique combines scintillators and optical microscopy to visualise positron-emitting tracers at near-cellular resolution in small samples, including patient-derived tumour organoids. oPEM can measure uptake of clinical PET tracers in organoids under different treatment conditions and has been proposed as a platform for drug screening that directly connects to clinical PET data from the same tracers.
Microfluidic PET and gamma imaging setups are also being extended to organoid-on-a-chip systems, which benefit from controlled perfusion and better integration with detector modules. These converging approaches allow researchers to investigate heterogeneity in tracer uptake within small 3D structures, revealing patterns that might be invisible in bulk assays but are very relevant for predicting treatment response.
Emerging application themes
As these technologies mature, several key application areas are crystallising.
Radiotracer and radiopharmaceutical development
Early-stage screening of new tracers traditionally involves repeated animal studies, which are time-consuming and costly. On-chip PET and related radionuclide techniques enable the evaluation of binding, internalisation, washout, and metabolism in well-controlled human-derived models first. Candidates with poor characteristics can be discarded or optimised before moving to animal work, potentially cutting the number of in vivo experiments and improving the quality of those that remain.
ADME and toxicity
Multi-organ chips with PET readout are used to study absorption, distribution, metabolism, and excretion (ADME) in a manner closer to clinical pharmacology than classical cell assays. For example, a radiolabelled drug can be tracked as it moves from a gut compartment to a liver compartment, then to a kidney-like structure, with time–activity curves providing quantitative inputs for pharmacokinetic and pharmacodynamic (PK/PD) models. PET signals can also reveal off-target accumulation that might predict organ-specific toxicity.
Oncology and theranostic optimisation
Tumour-on-a-chip systems are being used to test radionuclide therapies, including alpha- and beta-emitters, under conditions that model key aspects of the tumour microenvironment. PET or gamma imaging provides information on how long a therapeutic agent remains bound, how evenly it distributes through the tissue, and how combination treatments alter these properties. These data feed into dosimetry calculations and treatment planning strategies that can later be refined in animal models and clinical trials.
Alignment with total-body PET
The rise of total-body PET scanners, which can capture dynamic tracer behaviour across the whole human body simultaneously, has created fresh demand for mechanistic models of distribution and kinetics. Organ-on-a-chip systems using the same tracers and similar kinetic models can help interpret complex total-body PET datasets and may play a role in personalising therapy by providing patient-specific ex vivo data from biopsies or induced pluripotent stem cell (iPSC)-derived tissues.
Technical hurdles on the way
The field is moving quickly, but several technical challenges remain and are themselves active research topics.
First, spatial resolution and sensitivity must be balanced carefully. Organ-on-a-chip devices involve tiny volumes and often relatively low activity levels. This raises partial-volume issues and makes it more challenging to obtain high-quality kinetic data. Detector design, crystal size, timing resolution and reconstruction algorithms are all being tuned specifically for chip-scale imaging to get the most out of every detected event.
Second, environmental compatibility is non-trivial. Chips typically require humidified, temperature-controlled environments with access for optical microscopy and microfluidic tubing. PET detectors must operate close to this environment without overheating, introducing vibration, or blocking other instruments. Some groups are integrating PET modules into incubators or onto optical microscopes to enable multimodal imaging with minimal disruption of culture conditions.
Third, radiochemistry at the microlitre scale is challenging. Standard radiolabelling protocols assume millilitre volumes and higher activities. Microfluidic radiochemistry platforms are therefore being developed to produce tracers and radiolabelled drugs in quantities suited to chip experiments, with an emphasis on efficiency, low dead volumes and rapid synthesis to match half-lives.
Finally, there is the question of validation and standardisation. Regulatory agencies and industry partners will expect evidence that chip-based PET readouts correspond to relevant in vivo endpoints. This calls for systematic cross-comparison of chip, animal and human PET data, shared protocols, and possibly reference materials and benchmark devices. International initiatives are beginning to address these points as part of broader efforts to introduce new approaches and methodologies into safety and efficacy assessment.
Looking ahead
Putting all of this together, PET imaging for organ-on-a-chip appears to be moving through the classic trajectory from proof-of-concept towards early adoption in specialised labs.
We can expect to see more dedicated chip-scale PET systems emerge, including add-on modules for existing incubators and microscopes. Tumour- and body-on-a-chip platforms with PET readout will increasingly be used in radiotracer optimisation, radionuclide therapy research and mechanistic PK studies. Links between patient-derived organoids, organ-on-a-chip models, on-chip PET, and total-body PET will continue to tighten, providing a more coherent translational pipeline from bench to bedside.
For clinicians, this may translate into better-designed tracers, safer and more effective theranostic regimens, and more reliable predictions of how a new drug will behave across different patient populations. For researchers and regulators, combining PET with organ-on-a-chip offers a promising approach to generate human-relevant, quantitative data while reducing reliance on animal models.
For now, the field is still young, but the direction of travel is clear: PET is no longer confined to scanning whole bodies. It is becoming a powerful analytical tool for the miniature, engineered organs that are reshaping preclinical science.
Disclaimer
The information presented in PET Imaging Moves On-Chip: The New Phase of Organ-on-a-Chip Research is intended for educational and general informational purposes only. It does not constitute medical, scientific, regulatory, or professional advice, nor should it be used as a substitute for consultation with qualified specialists in imaging science, radiopharmacy, biomedical engineering, clinical research, or related fields.
Open MedScience does not make any guarantees regarding the accuracy, completeness, or timeliness of the material provided. Research areas such as organ-on-a-chip technology, PET imaging, and radiopharmaceutical development evolve rapidly, and findings may change as new evidence emerges. Readers are encouraged to verify key details through primary literature and to seek expert guidance before applying any concepts, methods, or interpretations described in this article.
Any views or interpretations expressed are those of the authors and do not necessarily reflect those of institutions, collaborators, or regulatory bodies. References to specific technologies, platforms, or studies are for illustrative purposes only and should not be taken as endorsements. Open MedScience accepts no liability for actions taken or not taken based on the content of this publication.
You are here: home » diagnostic medical imaging blog »