Prostate cancer research and clinical practice in the UK are undergoing significant change, driven by major national trials, new diagnostic approaches, and emerging treatments for advanced disease. Over the past year, several programmes have gathered pace, each aiming to address long-standing challenges around early detection, rapid diagnosis, disease inequality, and targeted therapies. Together, these efforts mark one of the most important pushes in UK prostate cancer care for decades.
The TRANSFORM Trial: Towards a National Screening Programme
The largest and most ambitious initiative is the £42 million TRANSFORM trial, which has officially launched across the UK. This study is designed to assess whether the country should adopt a national screening programme for prostate cancer, something experts and patient groups have been calling for due to the high number of men diagnosed each year.
Prostate cancer remains the most common cancer in men in the UK, yet there is still no routine screening scheme. The long-standing hesitation stems from concerns around the traditional prostate-specific antigen (PSA) blood test, which can struggle with accuracy. High PSA levels do not always mean cancer is present, and normal levels do not always rule it out. This inconsistency has made policymakers reluctant to approve widespread testing without more substantial evidence.
The TRANSFORM trial aims to change this. Rather than relying solely on PSA, the study is comparing new test combinations that may offer greater accuracy, fewer unnecessary biopsies, and earlier detection of disease that genuinely needs treatment.
In its first stage, around 16,000 men aged 50 to 74 will be invited through GP practices to take part. Men from higher-risk groups, including Black men and those with a family history of prostate cancer, will be invited from the age of 45. This focus on risk-based participation is a central feature of the trial, reflecting growing evidence that some groups face higher chances of developing aggressive disease.
One of the most advanced elements of the trial is the inclusion of a genetic saliva test. Researchers hope that by examining inherited markers linked to prostate cancer, clinicians will be able to identify those who benefit most from early imaging or further monitoring. Participants may also be offered a fast MRI scan, a shorter and simpler version of the prostate MRI that has become part of the modern diagnostic pathway.
The trial’s first phase will determine which combination of PSA, saliva testing, and MRI is most effective. Later stages will expand the study to as many as 300,000 men, generating evidence on a scale the UK has never seen for prostate cancer screening.
Reducing inequalities is also at the heart of TRANSFORM. Black men in the UK are twice as likely to develop prostate cancer and more likely to be diagnosed at a later stage. The trial organisers have committed to ensuring strong representation from this group, aiming for at least 10 per cent of participants to be Black men. Researchers hope this will finally provide clear evidence tailored to those who need it most.
Suppose TRANSFORM confirms that a multi-test screening approach is both accurate and cost-effective. In that case, the results will be presented to the UK National Screening Committee, which will then consider whether to recommend a national screening programme. Such a decision would be one of the most significant policy changes in men’s health in a generation.
A One-Day Diagnostic Pathway: NHS Pilots New AI-Supported System
While screening focuses on catching prostate cancer early, many men still face long waiting times once symptoms emerge or a PSA test raises concerns. MRI scans, biopsies, and follow-up appointments can stretch across several weeks, creating anxiety and delaying treatment.
A new NHS trial aims to fix this. Fifteen hospitals across England are preparing to introduce a “one-day diagnosis” pathway for suspected prostate cancer, supported by advanced artificial intelligence (AI). The first pilot site will be Leeds Teaching Hospitals NHS Trust, which will run the system early next year.
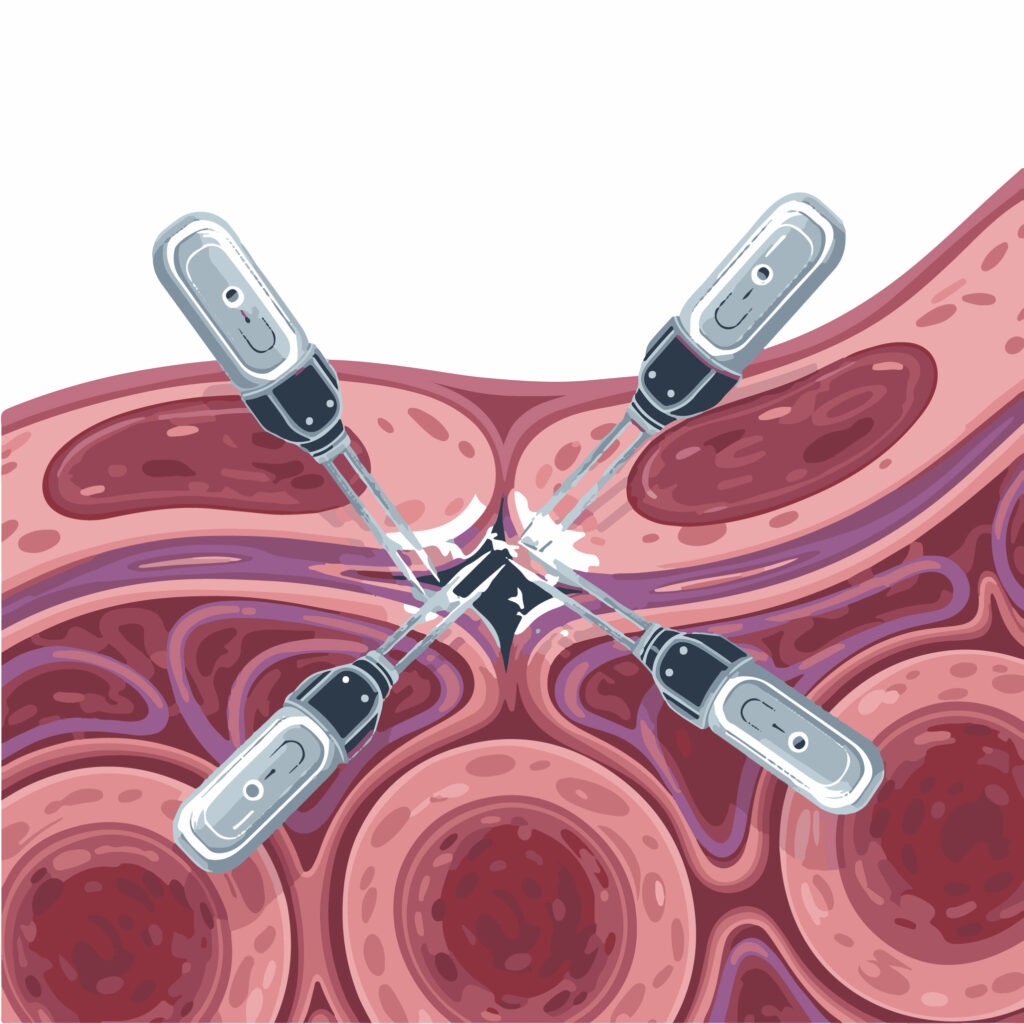
Under the new model, a man referred with suspected prostate cancer will have his MRI scanned, analysed, reviewed, and—if required—be booked for a biopsy on the same day. In some cases, the biopsy may be performed during the same visit.
The AI system, developed by British company Lucida Medical, rapidly analyses MRI images and highlights areas that may indicate cancer. This assists radiologists by prioritising urgent scans and reducing the chance of delays caused by high workloads or backlogs. If the AI flags a suspicious region, a radiologist can immediately review the scan and discuss the next steps with the patient.
NHS England believes this approach could shorten diagnosis times by up to a month. For many men, the difference between waiting weeks for answers and receiving them in a single day may have a major effect on their wellbeing. Faster diagnosis also helps ensure that aggressive cancers are identified without delay, giving clinicians more opportunities for treatment.
The trial reflects increasing confidence in the use of AI within NHS pathways, particularly in imaging. Unlike some AI systems used solely as triage tools, this one forms part of an integrated clinical pathway where human oversight remains central. Its role is to speed up the process, not replace clinical judgement.
If the pilot proves successful, the system could be rolled out nationally, forming a new standard for prostate cancer diagnosis across the NHS.
New Strategies for Advanced and Metastatic Disease
Alongside developments in screening and diagnosis, research teams across the UK are working to improve survival in advanced prostate cancer, where treatment challenges remain significant. When the disease spreads beyond the prostate, it becomes far harder to control, and new forms of therapy are urgently needed.
One major initiative is the INTENSIFY trial, which is supported by around £1.9 million in funding from Prostate Cancer UK. This study focuses on men with high-risk metastatic prostate cancer, examining whether starting more intensive treatment earlier can improve outcomes compared with current NHS standards.
Traditional treatment for metastatic disease typically involves hormone therapy, sometimes alongside chemotherapy or radiotherapy. However, researchers increasingly believe that earlier use of combination therapies might give patients a better chance, particularly when cancer is detected soon after it spreads. The INTENSIFY trial aims to provide clear evidence on whether such an approach offers longer survival or improved quality of life.
In parallel, laboratory researchers at The Institute of Cancer Research (ICR) in London have reported further progress in targeted treatment for advanced disease. A recent study found that as many as 40 per cent of advanced prostate cancers may respond well to a specific combination of drugs that block the AKT and CDK9 pathways.
Many aggressive prostate cancers lose the PTEN gene, which usually helps control cell growth. Without PTEN, cancer cells activate pathways that allow them to grow and resist treatment. By simultaneously inhibiting two pathways—AKT and CDK9—the drug combination triggers cell death in cancer cells rather than simply slowing growth.
While these findings are early, they open the door to a new kind of personalised therapy based on a patient’s tumour’s genetic profile. Clinical trials are expected to follow.
What These Developments Mean for Men in the UK
Taken together, the recent progress in UK prostate cancer research signals a significant shift in the national approach to the disease.
For screening, the TRANSFORM trial offers real hope that the UK will finally have a reliable method to identify cancer earlier. Early detection has long been seen as the missing piece of the puzzle, particularly given that prostate cancer often develops without symptoms in its early stages. A well-designed, accurate screening programme could help prevent thousands of advanced cancers each year.
The NHS AI-supported one-day diagnostic pathway may also change the care experience. Long waiting times have been a persistent problem, and anything that shortens the path will ease anxiety for men and allow treatment to begin faster.
Meanwhile, in the area of advanced disease, the combination of new clinical trials and targeted drug research highlights a strong commitment to improving survival and offering better treatment options for men whose cancer has already spread.
The Road Ahead
Although these developments are encouraging, challenges remain. Screening must balance early detection with the risk of over-diagnosis, ensuring that men are not treated unnecessarily for cancers that would never cause harm. The use of AI must be implemented carefully, with robust checks for accuracy and fairness. And for advanced disease, further trials will be essential before new drug combinations become widely available.
Even so, the momentum behind these initiatives suggests a real turning point in the UK’s approach to prostate cancer. With investment, collaboration between major research centres, and growing public awareness, the country is moving towards a future in which prostate cancer can be detected earlier, diagnosed faster, and treated more effectively than ever before.
Disclaimer
This article is provided for general information only and does not constitute medical advice. It should not be used as a substitute for consultation with qualified health professionals. Readers should seek personalised guidance from their GP or specialist regarding prostate cancer risk, screening options, diagnosis, or treatment. While every effort has been made to ensure accuracy at the time of publication, research findings, clinical practices, and NHS pathways may change. Open MedScience accepts no responsibility for actions taken based on the content of this article.