Radiology stands on the brink of a transformative era, with Artificial Intelligence (AI) at its core. The integration of AI in radiology heralds a future where diagnostic accuracy, efficiency, and personalised patient care reach unprecedented levels. This article outlines the advancements, potential impacts, ethical considerations, and the road ahead for AI in radiology, providing an outlook on its evolving landscape.
Introduction to Artificial Intelligence in Medical Diagnostics
Radiology, traditionally seen as the art and science of utilising various forms of radiant energy to diagnose and sometimes treat diseases, has long been a cornerstone of medical diagnostics. Its significance extends from early detection and diagnosis to guiding treatment decisions, making it indispensable across healthcare. The evolution of radiology over the years has been marked by significant technological advancements, from the discovery of X-rays to the development of computed tomography (CT), magnetic resonance imaging (MRI), and ultrasound. These innovations have continually enhanced the ability of radiologists to diagnose and understand a myriad of conditions with ever-increasing accuracy and detail.
The latest frontier in this evolution is the integration of Artificial Intelligence (AI) into radiology. AI, particularly machine learning (ML) and deep learning (DL) algorithms, have the potential to transform the field by augmenting the capabilities of radiologists. The promise of AI lies not just in automating routine tasks but in its ability to analyse and interpret medical images with a level of precision and efficiency that was previously unattainable. This shift is poised to revolutionise the way radiologists work, enhancing their role from diagnosticians to comprehensive clinical decision-makers.
The impact of AI on radiology is multifaceted. It offers the potential to significantly improve diagnostic accuracy by identifying subtle patterns and anomalies in images that the human eye may overlook. For instance, AI algorithms can detect minute signs of diseases such as early-stage cancers, brain aneurysms, or cardiac abnormalities, facilitating earlier and more accurate diagnoses. This early detection capability is crucial, as it can dramatically affect patient outcomes, offering a greater chance of successful treatment and, in many cases, survival.
Beyond diagnostic accuracy, AI stands to greatly enhance efficiency within radiology departments. The volume of diagnostic imaging studies has been increasing steadily, placing a considerable burden on radiologists who must interpret a vast number of images daily. AI can streamline this workflow by quickly sifting through images, prioritising those that require urgent attention, and automating the detection of common conditions. This helps manage workload more effectively and reduces the time to diagnosis, a critical factor in many acute and life-threatening conditions.
Furthermore, AI’s role in radiology extends into patient care, offering avenues for personalised treatment planning and predictive analytics. By analysing a patient’s imaging data over time, AI algorithms can predict disease progression and recommend the most effective treatment plans. This level of personalisation is at the heart of modern medicine with a shift towards more patient-centred care, where treatments are tailored to the individual’s specific condition and physiological makeup.
However, the integration of AI into radiology also presents challenges. Ethical considerations, data privacy, and the potential for algorithmic bias are significant concerns that must be addressed to fully realise the potential of AI in this field. Additionally, there is the question of how AI will change the role of radiologists. Rather than replacing human expertise, AI is more likely to augment and enhance the role of the radiologist by necessitating a shift in training and education to prepare the next generation of radiologists for a future where AI is an integral part of their toolkit.
The future of radiology lies in a harmonious integration of AI, where human expertise and artificial intelligence collaborate to improve diagnostic accuracy, enhance efficiency, and provide personalised patient care. As we stand on the brink of this transformative era, the trajectory of AI in radiology is not just about technological advancement but about reshaping the very foundations of how medical care is delivered. This promises a future where the full potential of radiology is realised in improving patient outcomes and advancing healthcare.
AI in Radiology: Current Landscape
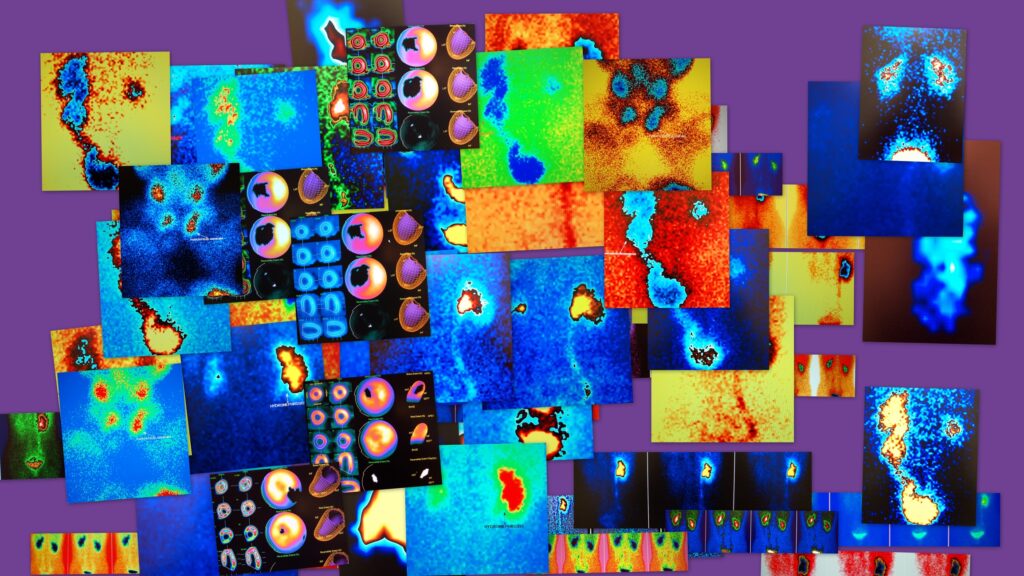
The integration of AI into radiology has been transformative, heralding a new era of diagnostic precision and efficiency. In the current landscape, the role of AI is rapidly expanding, leveraging its capabilities to enhance the interpretation of imaging data and support radiologists in making more informed decisions. Machine learning (ML) and deep learning (DL) algorithms are at the core of this transformation, and they have demonstrated remarkable success in identifying complex patterns within imaging data that may elude human detection.
These advanced AI models are being deployed across a spectrum of radiological applications, from detecting subtle signs of cancer in its early stages to identifying markers of neurological disorders and cardiovascular diseases. Their ability to rapidly process and analyse large volumes of imaging scans makes them invaluable tools in today’s healthcare settings, where the timely and accurate diagnosis of conditions can significantly influence treatment outcomes.
Moreover, AI algorithms are streamlining the diagnostic process by providing quicker results and enhancing the accuracy of these diagnoses. By learning from vast datasets of imaging scans, these algorithms are continuously improving, becoming more adept at recognising disease patterns and anomalies. This iterative learning process ensures that AI models remain at the cutting edge of diagnostic technology, offering up-to-date insights based on the latest radiological research and findings.
The current landscape of AI in radiology also highlights the potential for these technologies to revolutionise patient care. AI models are paving the way for more personalised treatment plans and improved patient outcomes by assisting in the early detection of diseases and providing precise, data-driven insights. As these technologies become more integrated into clinical workflows, they promise to augment the capabilities of the radiologist and redefine the standards of care in radiology departments worldwide.
Technological Advancements
The landscape of radiology is undergoing a significant transformation, courtesy of rapid technological advancements in AI. These advancements have propelled AI algorithms to a level of performance where, in certain cases, they equal or even surpass the diagnostic acumen of human radiologists. This milestone in AI development is not just theoretical but is being evidenced in clinical settings, where AI-driven tools demonstrate exceptional proficiency in identifying early signs of various diseases.
A striking example of the capabilities of AI is its precision in detecting early manifestations of conditions like pneumonia, breast cancer, and bone fractures in X-rays and MRIs. The algorithms, trained on vast datasets of radiological images, have learned to discern subtle abnormalities that may be indicative of these diseases. Their ability to do so with remarkable accuracy and speed is a testament to the potential of AI in enhancing diagnostic processes and patient outcomes.
Moreover, the synergy between AI and advanced imaging technologies is opening new frontiers in radiological assessment. The integration of AI with 3D imaging technology, for instance, has significantly improved the clarity and detail of images. This advancement allows for more nuanced interpretations of complex anatomical structures, offering radiologists a deeper understanding of patient conditions. Similarly, combining AI with molecular imaging facilitates more detailed analyses of biological processes at the cellular and molecular levels, contributing to earlier and more accurate diagnoses.
These technological advancements underscore the transformative potential of AI in radiology. By augmenting traditional imaging technologies’ capabilities, AI enables more comprehensive and precise assessments, which are crucial for early disease detection, accurate diagnosis, and effective treatment planning. As AI continues to evolve, its integration with radiological practices promises to further enhance patient care quality, marking a new era in medical diagnostics.
Impact on Diagnostic Accuracy and Efficiency
The integration of AI into radiology has ushered in a new era of diagnostic precision and operational efficiency, setting a benchmark for the future of medical imaging. At the heart of this transformation is the unparalleled capability of AI algorithms to rapidly process and analyse extensive volumes of imaging data. This proficiency accelerates the diagnostic process and enhances the accuracy of diagnoses, addressing two critical challenges in radiology: the increasing demand for imaging services and the imperative for high diagnostic accuracy.
One of the most profound impacts of AI on radiology is its ability to detect abnormalities in imaging scans with a level of detail and speed that surpasses human capability. These AI algorithms, powered by machine learning and deep learning technologies, are trained on thousands, if not millions, of images. This extensive training enables them to precisely identify patterns and anomalies, thus significantly reducing the margin for human error. By swiftly flagging potential issues for further review, AI helps radiologists prioritise cases and focus their expertise where it is most needed, enhancing the overall quality of patient care.
Furthermore, AI’s iterative learning process, where algorithms continuously improve through exposure to new data, ensures that the diagnostic capabilities of these systems are always evolving. This aspect of AI technology not only boosts diagnostic accuracy over time but also contributes to the development of more reliable and robust diagnostic tools. As AI algorithms become more refined, they offer the potential to uncover insights from imaging scans that might previously have been overlooked, further contributing to early disease detection and treatment.
The impact of AI on diagnostic accuracy and efficiency in radiology is profound and far-reaching. By augmenting the capabilities of radiologists, AI-driven tools promise to enhance the quality of diagnostic imaging, improve patient outcomes through early and accurate disease detection, and streamline radiology workflows, ultimately leading to a more efficient and effective healthcare system.
Personalised Patient Care
The integration of AI in radiology is revolutionising diagnostic practices and significantly enhancing the personalisation of patient care. At the heart of this transformation is AI’s prowess in predictive analytics, which is reshaping the approach to treatment planning and patient management. By leveraging AI to analyse a combination of imaging data and comprehensive medical histories, clinicians can gain profound insights into a patient’s health status, disease progression, and potential response to various treatment modalities.
This capability of AI to predict disease trajectories and treatment outcomes is pivotal for the advancement of personalised medicine. It allows healthcare providers to move beyond the one-size-fits-all approach, enabling them to devise treatment plans highly tailored to each patient’s individual characteristics. For instance, in oncology, AI can analyse tumour characteristics from imaging scans alongside genetic information to predict how a tumour is likely to respond to different chemotherapy drugs or radiation therapy. This can lead to a customised treatment regimen that targets the tumour more effectively while minimising exposure to potentially unnecessary or harmful treatments.
Moreover, AI’s predictive models can forecast the likelihood of disease recurrence or the development of secondary conditions, allowing for proactive management strategies that could delay or prevent adverse outcomes. Such predictions, grounded in a deep analysis of imaging data and historical health information, provide a foundation for ongoing monitoring and intervention strategies tailored to the patient’s unique health trajectory.
The transition towards more personalised patient care facilitated by AI optimises treatment efficacy and enhances patient engagement and satisfaction. By involving patients in decisions that are informed by AI-driven insights, healthcare becomes more collaborative, empowering patients to take an active role in managing their health. This marks a significant step towards a future where medical treatment is as individual as the patients themselves, with AI playing a central role in achieving this vision of personalised medicine.
Ethical Considerations and Challenges
While heralding a new era of medical diagnostics and treatment, the integration of AI into radiology brings with it a suite of ethical considerations and challenges that must be navigated with care. These ethical dilemmas are not just theoretical; they have practical implications that could affect the quality of patient care and trust in the healthcare system.
One of the foremost concerns is data privacy and security. AI systems in radiology rely on accessing vast amounts of sensitive patient data, including medical records and detailed imaging scans. The imperative to protect this data from breaches is paramount, as any compromise could have far-reaching consequences for patient privacy and the integrity of medical institutions. Ensuring the security of AI systems against cyber threats while maintaining patient confidentiality requires stringent data protection measures and ethical oversight.
Another significant ethical challenge is the potential for bias in AI algorithms. These biases can manifest when the data used to train AI models are not representative of the diverse patient populations they serve. For instance, if an AI system is predominantly trained on imaging data from a specific demographic, its diagnostic accuracy could be lower for patients outside of that demographic, leading to disparities in care. This raises questions about the fairness and impartiality of AI-assisted diagnoses and highlights the need for diverse and inclusive training datasets that reflect the heterogeneity of patient populations.
Addressing these ethical challenges necessitates the development of robust ethical frameworks that guide the deployment and operation of AI in radiology. Transparent algorithmic processes, where the decision-making mechanisms of AI systems are open to scrutiny, are essential to build trust among patients and practitioners. Moreover, ongoing monitoring and evaluation of AI systems are crucial to identify and correct biases, ensuring that AI-assisted diagnostics and treatments are fair, accurate, and beneficial to all patients.
In summary, while AI presents an opportunity to significantly enhance radiology practices, the ethical landscape it navigates is complex. The successful integration of AI into radiology will depend not only on technological advancements but also on our ability to address these ethical considerations thoughtfully and proactively, ensuring that AI serves the interests of all patients equitably.
The Road Ahead
The trajectory of AI in radiology is on a path of accelerated growth and innovation. The burgeoning capabilities of AI are not only reshaping diagnostic methodologies but are also set to redefine the entire spectrum of radiological services. The road ahead is marked by the continued evolution of AI’s interpretative abilities, with research and development efforts aimed at refining these technologies to be more intuitive and efficient. This progression includes the expansion of AI’s applications across a broader range of imaging techniques and medical conditions, enhancing its utility and impact on patient care.
A key aspect of this future is the deeper integration of AI into clinical workflows. The goal is to create a seamless interface between AI tools and radiological practices, ensuring that AI acts as an augmentative tool that complements radiologists’ expertise. Achieving this level of integration will require significant advancements in user-friendly interfaces, real-time processing capabilities, and systems that can provide actionable insights to radiologists without disrupting their workflows.
As AI becomes an integral part of the radiology landscape, there will be a consequential shift in radiology education and training. The emphasis will increasingly be on equipping new generations of radiologists with the skills to collaborate with AI effectively. Understanding the intricacies of AI algorithms, their strengths, limitations, and best use cases will become essential components of radiological education, ensuring that professionals can leverage these tools to enhance diagnostic accuracy and patient care.
Conclusion
AI represents a revolutionary force in the field of radiology, promising to enhance diagnostic precision, improve patient outcomes, and usher in an era of personalised medicine. While the journey ahead comes with its set of ethical and security challenges, the potential rewards are substantial. As we move forward, the continued refinement of AI technologies, combined with a thoughtful approach to addressing ethical considerations, will be crucial. This dual focus will ensure that AI not only advances the technical capabilities of radiology but also upholds the highest standards of patient care and equity. The future of radiology, powered by AI, promises to transform patient diagnoses and treatments, making it an exciting time for practitioners and patients alike.
Disclaimer
The information presented in this article is intended for general informational and educational purposes only. It does not constitute medical, clinical, legal, or professional advice, nor should it be interpreted as a substitute for consultation with qualified healthcare professionals. While efforts have been made to ensure the accuracy and currency of the content at the time of publication, Open Medscience makes no representations or warranties, express or implied, regarding the completeness, reliability, or suitability of the information provided.
Any reference to Artificial Intelligence (AI) technologies, products, or diagnostic capabilities reflects current trends and developments in the field of radiology as of the publication date. The inclusion of specific technologies or tools does not imply endorsement by Open Medscience, and outcomes may vary depending on clinical context and individual patient circumstances.
Readers are encouraged to consult appropriate medical professionals and regulatory guidelines before relying on AI-based diagnostics in practice. Open Medscience assumes no liability for any loss, damage, or adverse outcomes arising directly or indirectly from the use or application of information contained in this article.
home » blog » artificial intelligence »