Antibody-drug conjugates (ADCs) represent a groundbreaking therapeutic strategy in cancer treatment, combining the specificity of monoclonal antibodies with the potent cytotoxicity of chemotherapeutic drugs. This article explores the development, mechanism of action, clinical applications, benefits, challenges, and future potential of ADCs in oncology. ADCs have revolutionised targeted therapy by delivering cytotoxic agents directly to tumour cells, minimising systemic toxicity and maximising therapeutic efficacy. This precision medicine approach has shown significant promise, particularly in patients with refractory or relapsed cancers, and continues to evolve with new research and technological advancements.
Introduction to Antibody-Drug Conjugates
The treatment of cancer has advanced significantly over the past few decades, transitioning from conventional chemotherapy and radiotherapy to more targeted approaches such as immunotherapy. Among the novel therapeutic strategies, Antibody-Drug Conjugates (ADCs) have emerged as a key player in the field of targeted cancer therapy. ADCs combine the specificity of monoclonal antibodies (mAbs) with the cell-killing ability of cytotoxic drugs, offering a potent weapon in the fight against cancer.
This article will look into the concept of ADCs, their mechanism of action, their applications in cancer therapy, and the current challenges and future directions in the field.
What Are Antibody-Drug Conjugates?
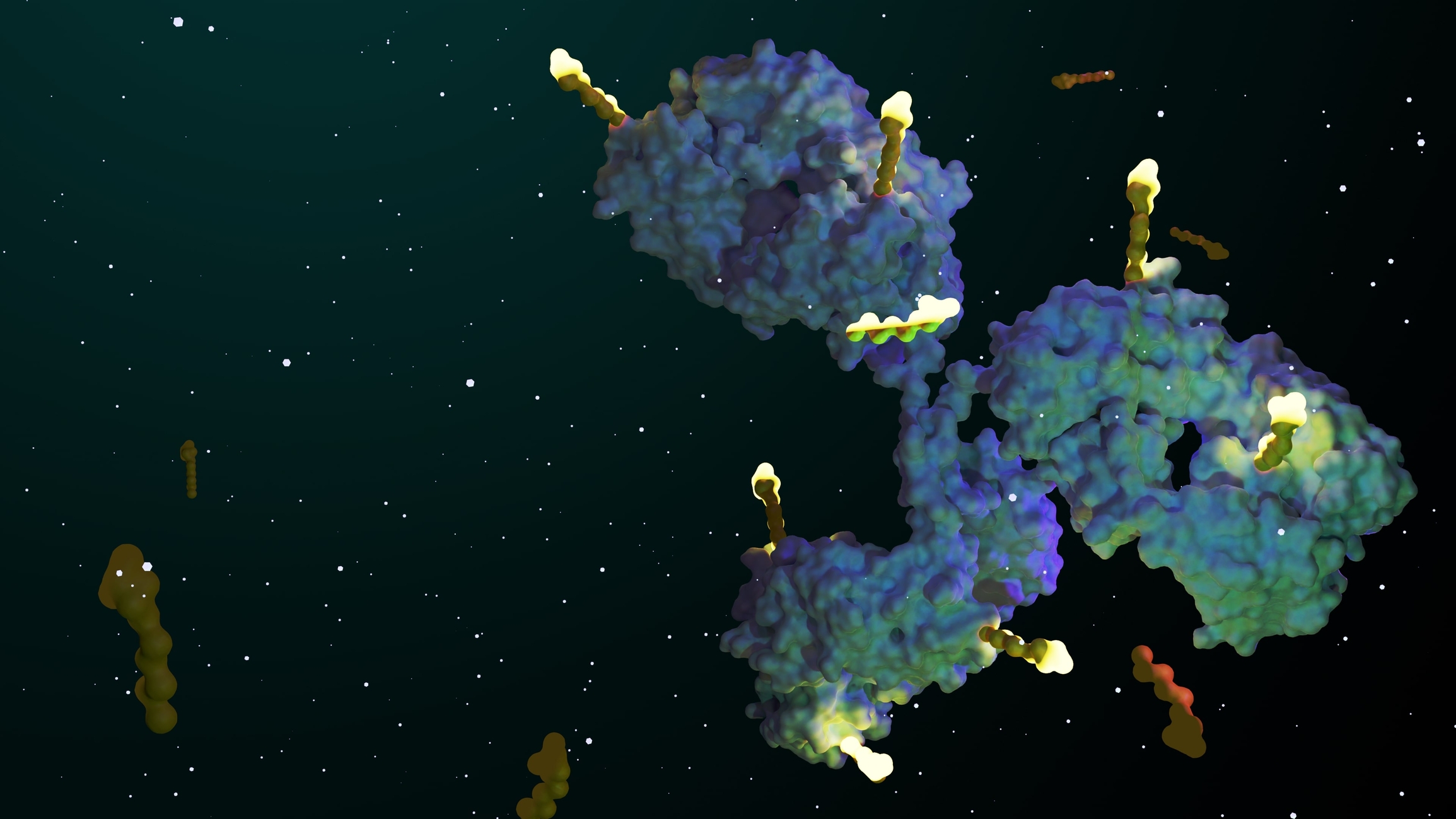
Antibody-drug conjugates are complex molecules consisting of three main components:
- Monoclonal Antibody (mAb): The antibody component is designed to specifically bind to an antigen that is overexpressed on cancer cells but has limited expression on normal cells.
- Linker: A chemical linker connects the antibody to the cytotoxic drug. The linker is crucial for the stability of the ADC in circulation and the release of the drug inside the target cells.
- Cytotoxic Payload: This is a highly potent drug, far more cytotoxic than standard chemotherapeutic agents. It is often too toxic to be administered alone, which is why it needs to be delivered specifically to cancer cells.
The basic principle of ADCs is to use the monoclonal antibody to guide the cytotoxic drug to the cancer cells, sparing normal tissues from damage and reducing the systemic side effects associated with traditional chemotherapy.
Mechanism of Action of ADCs
The mechanism of action of ADCs can be broken down into several steps:
- Target Recognition and Binding:
The monoclonal antibody component of the ADC binds to a specific antigen present on the surface of cancer cells. These antigens are usually proteins that are overexpressed in tumours compared to healthy tissues. - Internalisation:
After binding to the antigen, the ADC is internalised into the cancer cell through receptor-mediated endocytosis. This ensures that the drug is delivered specifically to the cancerous cell, rather than affecting healthy cells. - Payload Release:
Once inside the cancer cell, the ADC is transported to lysosomes, where the linker is broken down, releasing the cytotoxic payload. The release of the drug is often triggered by the acidic or enzymatic environment inside the cell. - Cell Death:
The cytotoxic drug then exerts its effect, typically by interfering with cellular processes such as DNA replication, ultimately leading to cell death.
This targeted approach helps minimise damage to normal tissues while maximising the impact on cancer cells.
Current ADCs in Cancer Therapy
As of today, several ADCs have been approved for the treatment of different types of cancers, and many more are in clinical development. The most notable approved ADCs include:
- Brentuximab Vedotin (Adcetris):
This ADC targets CD30, a marker found on certain types of lymphoma cells. It is used to treat Hodgkin lymphoma and systemic anaplastic large cell lymphoma. - Trastuzumab Emtansine (Kadcyla):
Trastuzumab emtansine targets HER2, a protein overexpressed in some breast cancer cells. It is used for HER2-positive metastatic breast cancer in patients who have previously been treated with trastuzumab and chemotherapy. - Enfortumab Vedotin (Padcev):
This ADC targets Nectin-4, which is expressed in bladder cancer cells. It is used in the treatment of locally advanced or metastatic urothelial cancer. - Sacituzumab Govitecan (Trodelvy):
Sacituzumab govitecan targets Trop-2, a protein overexpressed in several types of cancers, including triple-negative breast cancer. It is approved for patients with metastatic triple-negative breast cancer.
These ADCs have demonstrated significant efficacy in patients with refractory or relapsed cancers, where traditional treatments may no longer be effective.
Advantages of ADCs
The development of ADCs has provided several advantages in the treatment of cancer:
- Increased Specificity:
By targeting specific antigens on cancer cells, ADCs reduce off-target effects and minimise damage to healthy cells. - Improved Therapeutic Index:
ADCs enable the use of highly potent cytotoxic drugs that would be too toxic to administer systemically. This allows for a higher therapeutic index, meaning the drug can be more effective at lower doses, reducing adverse effects. - Overcoming Drug Resistance:
ADCs can be effective in cases where cancer cells have developed resistance to conventional therapies. Since they deliver the cytotoxic agent directly to the cancer cells, they can bypass some of the mechanisms of resistance, such as drug efflux pumps. - Personalised Medicine:
ADCs are part of the broader trend towards personalised medicine, where treatments are tailored to the molecular characteristics of a patient’s tumour. This allows for more effective and targeted therapy.
Challenges and Limitations
While ADCs represent a promising advance in cancer therapy, they are not without their challenges and limitations:
- Target Antigen Selection:
Identifying appropriate target antigens that are highly expressed on cancer cells but have limited expression on normal tissues is crucial for the success of ADCs. If the antigen is also present on normal cells, the ADC may cause off-target toxicity. - Development of Resistance:
Just like other cancer treatments, resistance can develop to ADCs. Tumour cells may alter the expression of the target antigen or develop mechanisms to expel the ADC or its cytotoxic payload before it can exert its effects. - Drug Conjugation and Stability:
The stability of the linker between the antibody and the drug is critical. If the linker is too unstable, the cytotoxic drug may be released before it reaches the tumour, causing systemic toxicity. Conversely, if the linker is too stable, the drug may not be released effectively within the tumour cell. - Toxicity:
Although ADCs are designed to reduce toxicity compared to conventional chemotherapy, they are not entirely without side effects. Some patients may experience adverse reactions due to the release of the cytotoxic payload in healthy tissues or the immune response to the antibody. - Cost and Accessibility:
ADCs are complex and expensive to manufacture, making them costly for healthcare systems and patients. This can limit accessibility, particularly in low- and middle-income countries.
Future Directions in ADC Development
The field of ADCs is evolving rapidly, with ongoing research focused on overcoming the current challenges and improving the efficacy and safety of these therapies. Some of the key areas of future development include:
- Next-Generation Payloads:
Researchers are developing new cytotoxic drugs with different mechanisms of action, such as immune-stimulating agents or drugs that target novel cellular pathways, to be used as payloads in ADCs. - Improved Linker Technologies:
Advances in linker chemistry are being explored to ensure that the cytotoxic drug is released more precisely within cancer cells, reducing the risk of off-target toxicity. - Targeting New Antigens:
New tumour-specific antigens are continually being identified, expanding the range of cancers that can potentially be treated with ADCs. Researchers are also investigating ways to target intracellular antigens by using ADCs that can penetrate the tumour cell membrane. - Combination Therapies:
ADCs are increasingly being tested in combination with other therapies, such as immune checkpoint inhibitors, to enhance their efficacy. The combination of ADCs with other treatment modalities may help to overcome resistance and improve outcomes in patients with advanced cancers. - Bispecific ADCs:
A new frontier in ADC development is the creation of bispecific ADCs that can target two different antigens on cancer cells, potentially increasing the specificity and efficacy of the treatment.
Conclusion
Antibody-drug conjugates represent a significant advancement in the field of cancer therapy, offering a more targeted approach to treatment that reduces the systemic side effects associated with traditional chemotherapy. While there are still challenges to be addressed, the clinical success of several ADCs has demonstrated the potential of this approach. As research continues and technology improves, ADCs are likely to play an increasingly important role in the treatment of cancer, particularly in the era of personalised medicine.
Their ability to deliver highly potent cytotoxic agents directly to tumour cells, coupled with ongoing innovations, makes ADCs a promising avenue for improving patient outcomes and expanding therapeutic options in oncology. With further advancements, ADCs have the potential to revolutionise cancer treatment and provide new hope to patients facing difficult-to-treat cancers.
Disclaimer
The information provided in this article is for general educational and informational purposes only and is not intended as medical advice, diagnosis, or treatment. Open Medscience does not provide clinical or therapeutic recommendations and the content should not be used as a substitute for professional medical judgement or consultation with qualified healthcare providers. While every effort has been made to ensure the accuracy and reliability of the information presented, no guarantees are made regarding its completeness or timeliness.
Any references to specific drugs, therapies, or medical approaches are intended for illustrative purposes and do not imply endorsement. Readers are encouraged to consult healthcare professionals before making any decisions related to medical care or treatment options.
Open Medscience assumes no responsibility or liability for any consequence resulting directly or indirectly from any action or inaction based on the content of this article.
home » blog » medicine »