Summary: Radiation has revolutionised modern medicine, enabling earlier diagnoses, more precise treatments, and improved outcomes across a range of diseases. However, with these benefits comes a serious responsibility: ensuring the safety of healthcare professionals and patients exposed to ionising radiation. This article examines the crucial importance of radiation safety in medical practice, tracing its regulatory foundations, technological advancements, common challenges, and emerging concerns. With increasing reliance on medical imaging and radiotherapy, robust safety protocols and a culture of awareness are essential to minimise risks and safeguard public health.
Keywords: radiation safety, medical imaging, radiotherapy, healthcare workers, ionising radiation, patient protection.
Introduction
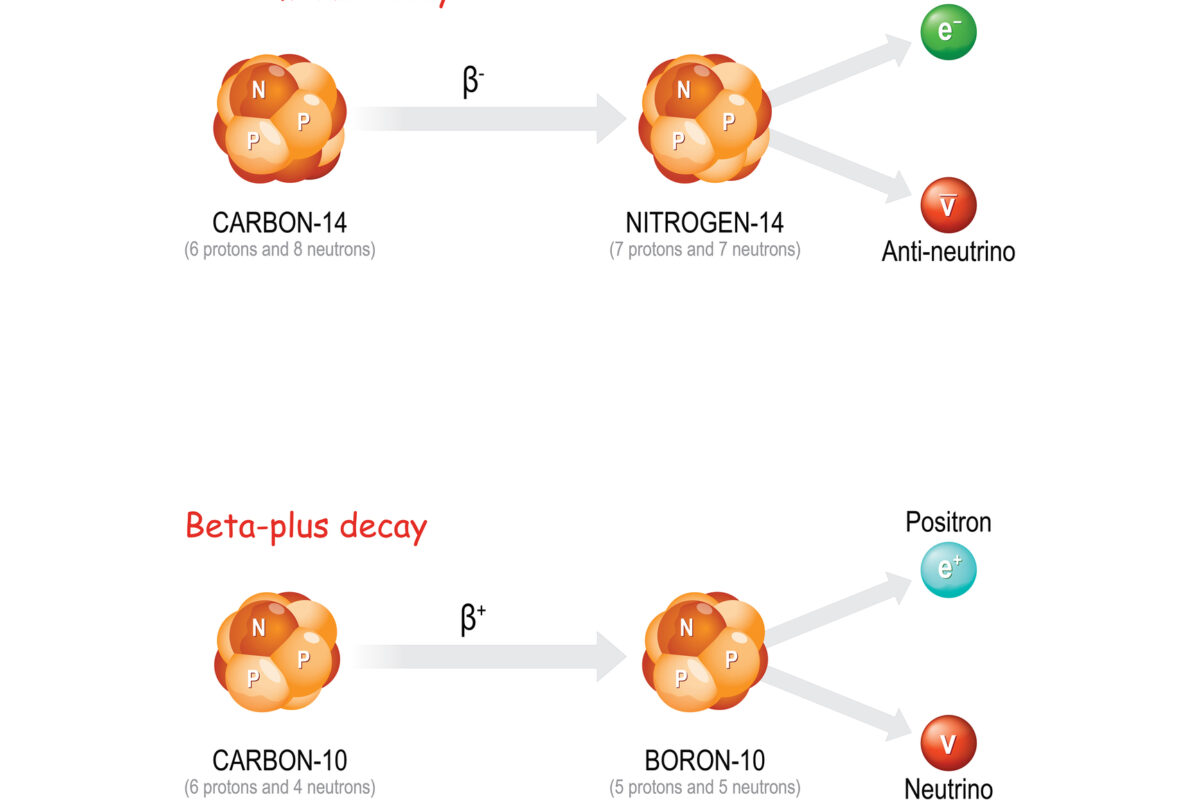
Medical applications of radiation have become indispensable tools in the diagnosis and treatment of disease. From X-rays to computed tomography (CT), nuclear medicine, and radiotherapy, radiation has extended the boundaries of what is medically possible. Yet, ionising radiation is not without consequence. Exposure carries potential risks, including deterministic effects such as skin burns and radiation sickness, and stochastic effects like cancer induction, particularly with prolonged or high doses.
Radiation safety in medicine encompasses a range of practices, procedures, regulations, and technologies designed to protect patients, healthcare workers, and the public from the adverse effects of radiation while ensuring the delivery of effective clinical care. This field intersects with medical physics, radiology, oncology, occupational health, and healthcare management, requiring a collaborative and proactive approach.
Historical Perspective and the Evolution of Safety Culture
The use of radiation in medicine dates back to the discovery of X-rays by Wilhelm Röntgen in 1895 and the pioneering work of Marie and Pierre Curie in the field of radioactivity. In those early days, the dangers of radiation were not well understood. Healthcare professionals routinely operated equipment without shielding, dosimetry, or protective barriers. The consequences were tragic, with many pioneers suffering radiation-induced injuries or early deaths.
It wasn’t until the mid-20th century, following both medical observations and the catastrophic events of Hiroshima, Nagasaki, and nuclear accidents, that the seriousness of radiation exposure was fully recognised. These events prompted the formation of international bodies, such as the International Commission on Radiological Protection (ICRP), and national regulatory agencies, all of which are tasked with setting dose limits and best practice guidelines.
The concept of ALARA — “As Low As Reasonably Achievable” — emerged as a cornerstone principle of radiation protection. It underscores the need to limit exposure by balancing benefit and risk, encouraging minimisation of dose without compromising diagnostic or therapeutic value.
Occupational Exposure: Risks and Regulation
Healthcare professionals working in radiology, interventional cardiology, nuclear medicine, and radiotherapy are at the frontline of occupational exposure. Unlike patients, who generally receive radiation during a limited number of procedures, staff may be exposed daily, sometimes for years or decades.
The UK’s Ionising Radiations Regulations (IRR17) require employers to assess and manage radiation risks, designate controlled areas, train staff, and monitor doses. Personal dosimeters and area monitoring are critical components of this framework. Workers classified as ‘radiation workers’ must undergo regular health surveillance and dose recording. The annual effective dose limit for occupational exposure in the UK is 20 millisieverts (mSv), though most workers receive well below this amount.
Lead aprons, thyroid shields, lead glasses, and fixed or mobile protective barriers are standard in interventional procedures. However, compliance with wearing protective equipment can be inconsistent, especially under high workloads or in emergency settings. Long-term exposure, even within regulatory limits, is a growing concern, particularly with procedures involving fluoroscopy, which can emit high levels of scattered radiation.
Patient Protection and the Justification of Medical Exposures
Patient safety is equally critical. The challenge lies in balancing diagnostic quality and therapeutic effectiveness against the potential risks of unnecessary radiation. Every medical exposure must be justified: it should provide a net clinical benefit and should not be conducted solely for non-medical reasons, such as administrative convenience.
Diagnostic reference levels (DRLs) are used to help identify unusually high or low radiation doses in standard imaging procedures. While DRLs are not strict limits, they serve as a benchmark to optimise practice and flag potential issues.
In radiotherapy, patients often receive very high doses of radiation aimed at tumour control. Here, precision is vital. Advances such as image-guided radiotherapy (IGRT), intensity-modulated radiotherapy (IMRT), and proton therapy allow tighter dose conformity and reduce exposure to surrounding healthy tissues. Nevertheless, planning errors, equipment malfunctions, and human errors can still lead to overexposure, underscoring the need for robust quality assurance and incident reporting systems.
Technological Innovations and Their Impact
Technology has played a vital role in reducing radiation risk. Digital imaging has replaced traditional film, allowing for better image quality at lower doses. Dose-tracking software and automatic exposure controls help optimise parameters in real-time, and new imaging techniques, such as low-dose CT scanning, continue to emerge.
In interventional radiology, real-time dosimetry and feedback systems enable operators to adjust their techniques in real-time. In nuclear medicine, advancements in radiopharmaceutical design and hybrid imaging systems, such as PET/CT and SPECT/CT, enable shorter scan times and lower administered activities.
Automation and artificial intelligence (AI) offer further promise. AI algorithms can assist in protocol optimisation, anomaly detection, and patient positioning, reducing the need for repeat scans and human error.
Yet, technology is not a panacea. Overreliance on automated systems can dull clinical vigilance. Newer equipment may have complex interfaces and require additional training, without which safety benefits may not be realised. Furthermore, high-end technology is not evenly distributed, especially in low- and middle-income countries, where older machines may still be in widespread use without the latest safety features.
Radiation Incidents and Learning from Mistakes
Radiation safety is not merely a technical or regulatory issue — it is deeply embedded in healthcare culture. Mistakes, though rare, do occur and can be devastating. Overdoses in radiotherapy, missed pregnancies in imaging, or equipment malfunctions leading to repeated scans are just a few examples of reportable incidents.
In the UK, such events are covered under the Ionising Radiation (Medical Exposure) Regulations (IR(ME)R). Healthcare providers are required to report significant accidental or unintended exposures to the appropriate authority, typically the Care Quality Commission (CQC). Root cause analyses, learning from errors, and implementing corrective actions are all part of the response mechanism.
Open reporting without fear of punishment is essential to building a culture of safety. Staff must feel empowered to raise concerns and report near-misses. Leadership plays a key role in modelling this behaviour and ensuring transparency.
Training, Awareness, and the Human Factor
Ultimately, the most advanced equipment and comprehensive regulations cannot replace the importance of well-informed, well-trained professionals. Radiation protection training is mandatory for all healthcare staff working with ionising radiation, but the quality and frequency of this training can vary.
Clinical staff must understand not only the physical principles of radiation but also how their behaviour influences exposure. For instance, standing at a greater distance from the source, properly positioning shielding, and communicating effectively with colleagues all contribute to reducing the dose.
Continuing professional development is key, particularly as techniques evolve and new risks emerge. Awareness campaigns, audits, and simulation-based training can help maintain high standards and promote a shared responsibility for safety.
Radiation safety is also influenced by systemic pressures, including understaffing, time constraints, and increased patient throughput, which can all lead to shortcuts or lapses in care. Investing in staffing, workflow design, and supportive environments is essential to enable safe practice.
Emerging Challenges and the Way Forward
As medical imaging and radiotherapy continue to expand, so too do the associated challenges. The increasing use of CT scans, particularly in emergency departments and for screening, raises questions about cumulative dose and long-term cancer risk. Patients with chronic illnesses may undergo repeated scans over many years, which could result in significant cumulative exposure.
New modalities, such as theranostics (combining therapy and diagnostics in nuclear medicine), bring both opportunities and risks. Handling novel radionuclides requires updated protocols and specialised training.
Cybersecurity is also becoming a concern. Imaging equipment and treatment planning systems are now digital and often interconnected via a network. A cyberattack or software failure could interrupt services or, in worst-case scenarios, affect dose calculations.
Globally, there is a need to harmonise safety standards and support countries with limited infrastructure. The International Atomic Energy Agency (IAEA) has launched initiatives to enhance radiation protection worldwide; however, further investment and political commitment are necessary to close the existing gap.
Conclusion
Radiation has transformed healthcare and continues to save lives every day. Yet, its use must be approached with respect, diligence, and a relentless commitment to safety. The protection of both patients and staff is not a static goal, but an ongoing challenge that requires vigilance, education, and adaptation.
The future of radiation safety in medicine lies in a balanced integration of regulation, innovation, and culture. With greater collaboration between technologists, clinicians, physicists, managers, and regulators, the goal is clear: to harness the power of radiation while ensuring that the benefits always outweigh the risks. In doing so, we protect not only the individual but also the integrity of the medical profession itself.
Disclaimer
This article is intended for informational and educational purposes only. While every effort has been made to ensure the accuracy and relevance of the content, Open Medscience does not guarantee that the information is complete, up to date, or applicable to all clinical or regulatory situations. The views expressed are those of the author(s) and do not necessarily reflect the opinions of regulatory bodies, healthcare institutions, or other professional organisations.
This publication does not constitute medical, legal, or professional advice. Healthcare professionals and institutions should always refer to national and international regulations, local policies, and current clinical guidelines when making decisions regarding radiation safety practices.
Open Medscience accepts no liability for any actions taken or omissions made based on the information provided in this article. Readers are encouraged to consult qualified experts for specific guidance related to radiation protection in their respective settings.
home » blog » medical physics »