Radiopharmacy, a crucial branch of medical science, combines the expertise of pharmacy with the specialised knowledge of radiochemistry to create radiopharmaceuticals. These compounds are indispensable in nuclear medicine, facilitating both the diagnosis and treatment of various diseases. This article explores the fundamental principles behind radiopharmacy, including the nature and preparation of radiopharmaceuticals, radiolabelling, the physics of radioactive decay, quality control, and safety protocols. It also looks into the applications of radiopharmaceuticals in diagnostic imaging and therapy, highlighting the critical role radiopharmacists play in ensuring these compounds’ efficacy and safety.
Introduction to Radiopharmacy
Radiopharmacy, also known as nuclear pharmacy, is a specialised field within pharmacy and medicine that focuses on preparing, handling, and dispensing radioactive substances, known as radiopharmaceuticals, used for diagnosis and therapy. These compounds are integral to nuclear medicine, where they provide vital information about the functioning of organs, tissues, and cells and are also used to treat certain diseases, particularly cancers.
Radiopharmaceuticals are unique in that they require the knowledge of pharmacology and a deep understanding of nuclear chemistry, physics, and radiobiology. Developing and applying these compounds necessitates stringent quality control measures and adherence to safety protocols to protect the patient and healthcare professionals.
Nature and Types of Radiopharmaceuticals
Radiopharmaceuticals are composed of a radioactive isotope, known as a radionuclide, and a biologically active molecule. The radionuclide emits radiation detectable by imaging devices or interacts with tissues for therapeutic effects. The biologically active molecule targets specific organs, tissues, or cellular receptors, ensuring the radionuclide’s delivery to the intended site within the body.
There are two main types of radiopharmaceuticals:
- Diagnostic Radiopharmaceuticals: These are used primarily for imaging and include compounds such as Technetium-99m, Fluorine-18, and Iodine-123. These radiopharmaceuticals emit gamma rays or positrons, which are captured by imaging devices like gamma cameras or PET scanners. They are designed to provide detailed images of organs and tissues, aiding in the diagnosis of conditions such as cancer, cardiovascular disease, and neurological disorders.
- Therapeutic Radiopharmaceuticals: These are used to treat diseases by delivering targeted radiation to specific tissues. Examples include Iodine-131, used to treat thyroid cancer, and Lutetium-177, used in the treatment of neuroendocrine tumours. The radiation emitted by these compounds causes damage to the targeted cells, leading to their destruction while minimising harm to surrounding healthy tissues.
Radiolabelling and Its Importance
Radiolabelling is the process of attaching a radionuclide to a biologically active molecule. This is a critical step in the production of radiopharmaceuticals, as it determines the compound’s specificity and stability. The choice of radionuclide and the method of labelling depend on the intended application, the desired half-life of the radiopharmaceutical, and the chemical properties of the molecule to be labelled.
There are several methods of radiolabelling, including:
- Direct Labelling: Where the radionuclide is directly attached to the molecule.
- Indirect Labelling: Where a chelator or linking agent is used to bind the radionuclide to the molecule.
- Isotopic Exchange: Where a stable isotope in the molecule is replaced with a radioactive isotope.
The radiolabelling process must be carefully controlled to ensure the radiopharmaceutical’s purity, stability, and bioavailability, as these factors significantly impact its efficacy and safety.
The Physics of Radioactive Decay
Understanding the physics of radioactive decay is fundamental to radiopharmacy. Radionuclides undergo decay, releasing radiation in the form of alpha particles, beta particles, or gamma rays. The type of radiation emitted and the energy it carries are key considerations when selecting radionuclides for radiopharmaceuticals.
- Alpha Decay: Involves the emission of alpha particles (helium nuclei) and is characterised by its high energy but low penetration. Alpha-emitting radiopharmaceuticals are used therapeutically to destroy diseased tissues, particularly in cancers.
- Beta Decay: Involves the emission of beta particles (electrons or positrons). Beta-minus emitters are used therapeutically to damage cellular DNA, while beta-plus emitters (positrons) are used in PET imaging.
- Gamma Decay: Involves the emission of gamma rays, which have high penetration power and are ideal for imaging. Gamma-emitting radionuclides are commonly used in diagnostic radiopharmaceuticals.
Another critical parameter is the half-life of a radionuclide. It refers to the time required for half of the radioactive atoms to decay. The half-life must be appropriate for the radiopharmaceutical’s intended use; diagnostic agents typically have short half-lives to minimise radiation exposure, while therapeutic agents may have longer half-lives to ensure sustained delivery of radiation to diseased tissues.
Quality Control in Radiopharmacy
Quality control (QC) is essential to radiopharmacy, ensuring that radiopharmaceuticals meet stringent standards before being administered to patients. QC measures include testing for radiochemical purity, sterility, apyrogenicity (absence of fever-causing contaminants), and the correct radiolabelling of the compound.
Radiochemical purity is particularly important, as impurities can affect the distribution and effectiveness of the radiopharmaceutical. Techniques such as thin-layer chromatography (TLC), high-performance liquid chromatography (HPLC), and gamma spectroscopy are commonly used to assess radiochemical purity.
Sterility and apyrogenicity are crucial to prevent infections or adverse reactions in patients. Radiopharmaceuticals are often produced under aseptic conditions, and sterility testing is conducted to ensure they are free from microbial contamination. Pyrogen testing, often done using the Limulus Amebocyte Lysate (LAL) assay, is used to detect endotoxins that could cause fever in patients.
Safety Protocols in Radiopharmacy
Safety is a paramount concern in radiopharmacy due to the potential hazards associated with handling radioactive materials. Radiopharmacists and technicians follow strict safety protocols to protect themselves, their colleagues, and patients from unnecessary radiation exposure.
Key safety measures include:
- Radiation Shielding: Using lead shields, barriers, and containers to minimise exposure to radiation.
- Personal Protective Equipment (PPE): Wearing gloves, lab coats, and eye protection to prevent contamination and exposure.
- Radiation Monitoring: Regularly monitoring radiation levels in the work environment and on personnel using dosimeters and other detection devices.
- Waste Management: Proper disposal of radioactive waste according to regulatory guidelines to prevent environmental contamination.
- Training and Education: Ensuring all personnel involved in radiopharmacy are adequately trained in radiation safety and emergency procedures.
Applications of Radiopharmaceuticals
Radiopharmaceuticals have a wide range of applications in both diagnostic imaging and therapy.
Diagnostic Imaging
One of the most significant applications of radiopharmaceuticals is in diagnostic imaging, which includes techniques such as:
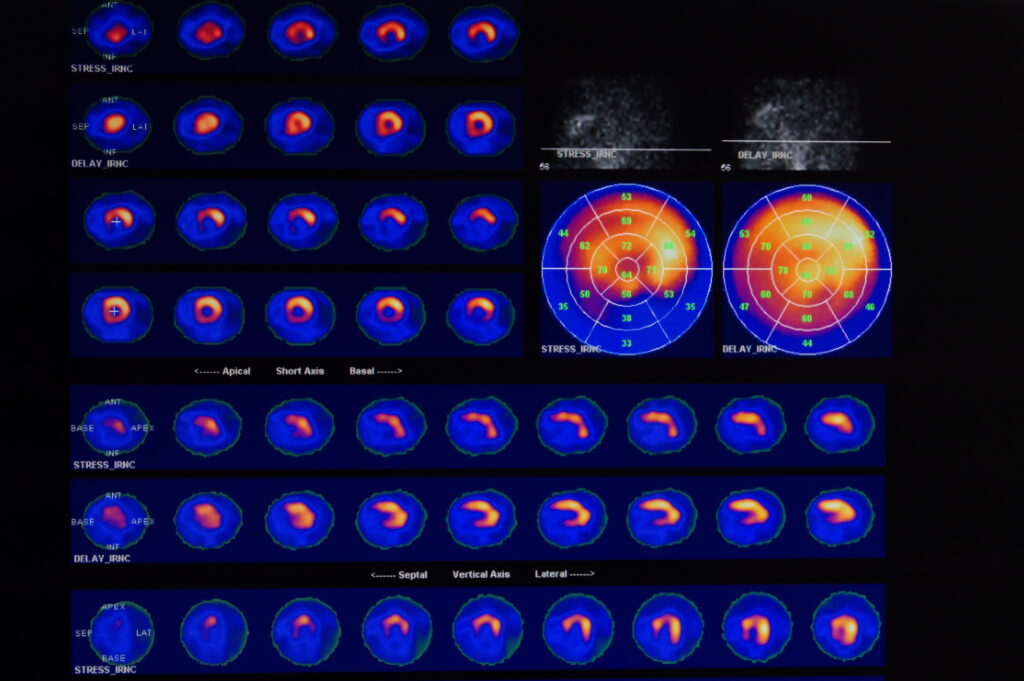
- Single Photon Emission Computed Tomography (SPECT): Utilises gamma-emitting radiopharmaceuticals like Technetium-99m to create 3D images of organs and tissues.
- Positron Emission Tomography (PET): Uses positron-emitting radiopharmaceuticals such as Fluorine-18 to produce detailed images of metabolic processes in the body.
These imaging techniques are invaluable in diagnosing various conditions, including cancer, heart disease, and neurological disorders. They provide detailed information about the function of organs and tissues, enabling early detection and accurate assessment of diseases.
Therapeutic Applications
Radiopharmaceuticals are also used therapeutically to treat various diseases, particularly cancers. Examples include:
- Radioiodine Therapy: Iodine-131 is used to treat thyroid cancer and hyperthyroidism. It is taken up by the thyroid gland, where it emits beta radiation to destroy diseased tissue.
- Peptide Receptor Radionuclide Therapy (PRRT): Uses radiolabelled peptides, such as Lutetium-177, to target and destroy neuroendocrine tumours.
- Radium-223 Therapy: Used to treat bone metastases in prostate cancer by delivering alpha radiation directly to the bone, killing cancer cells while sparing healthy tissue.
The Role of Radiopharmacists
Radiopharmacists are specialised professionals responsible for the preparation, quality control, and dispensing of radiopharmaceuticals. They play a critical role in ensuring these compounds’ safety, efficacy, and regulatory compliance.
Radiopharmacists must possess a deep understanding of both pharmacy and nuclear medicine, and they work closely with physicians, radiologists, and technologists to provide optimal patient care. Their responsibilities include:
- Preparation and Dispensing: Compounding radiopharmaceuticals under strict aseptic conditions, ensuring correct dosages, and verifying the identity and purity of the compounds.
- Quality Control: Conducting QC tests to ensure radiopharmaceuticals meet regulatory standards and are safe for patient use.
- Radiation Safety: Implementing and monitoring radiation safety protocols to protect staff and patients.
- Regulatory Compliance: Ensuring all activities related to radiopharmaceuticals comply with local, national, and international regulations.
Advances and Future Directions in Radiopharmacy
Radiopharmacy is a rapidly evolving field. Research is ongoing to develop new radiopharmaceuticals and improve existing ones. Advances in molecular biology, nanotechnology, and imaging techniques are driving innovation in this area.
- Targeted Radiopharmaceuticals: Research is focused on developing more targeted radiopharmaceuticals that can precisely deliver radiation to diseased cells while sparing healthy tissues. This includes the use of antibodies, peptides, and small molecules to target specific cellular receptors.
- Personalised Medicine: The development of radiopharmaceuticals tailored to individual patients’ genetic profiles and disease characteristics is an exciting area of research. This personalised approach promises to improve treatment efficacy and reduce side effects.
- Improved Imaging Techniques: Advances in imaging technology, such as hybrid PET/MRI scanners, are enhancing the diagnostic capabilities of radiopharmaceuticals, providing more detailed and accurate images.
Regulatory Aspects of Radiopharmacy
Due to their radioactive nature, the production, distribution, and use of radiopharmaceuticals are highly regulated. Regulatory bodies such as the Medicines and Healthcare Products Regulatory Agency (MHRA) in the UK, the Food and Drug Administration (FDA) in the United States, and the European Medicines Agency (EMA) oversee the approval and monitoring of these compounds.
Regulations cover various aspects, including:
- Manufacturing Practices: Radiopharmaceuticals must be produced in facilities that adhere to Good Manufacturing Practice (GMP) standards, ensuring the quality and safety of the products.
- Clinical Trials: New radiopharmaceuticals undergo rigorous clinical testing to establish their safety, efficacy, and appropriate dosage before being approved.
- Licensing and Distribution: Only licensed professionals and facilities are authorised to handle and dispense radiopharmaceuticals, and their use is restricted to specific medical indications.
Conclusion
Radiopharmacy is a vital and dynamic field that bridges the gap between pharmacy, chemistry, and nuclear medicine. The principles behind radiopharmacy encompass the careful selection, preparation, and handling of radiopharmaceuticals to ensure they are safe and effective for both diagnostic and therapeutic purposes. Radiopharmacists play a crucial role in this process, combining their expertise in pharmacy with a deep understanding of radiation science to advance patient care.
As the field continues to evolve, with new advances in targeted therapies and personalised medicine, radiopharmacy will remain at the forefront of medical innovation, contributing to the diagnosis and treatment of diseases in increasingly precise and effective ways.
Disclaimer
The content provided in this article is intended for informational and educational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. While every effort has been made to ensure the accuracy and currency of the information presented, Open Medscience does not guarantee its completeness or reliability and accepts no liability for any errors or omissions. Readers are advised to consult qualified healthcare professionals or regulatory authorities for advice tailored to their specific circumstances before acting upon any information contained herein. Any reference to commercial products, processes, or services does not constitute or imply endorsement by Open Medscience.
Radiopharmaceuticals involve the use of radioactive materials, which are subject to strict regulations and should only be handled by trained and licensed professionals in accordance with applicable laws and safety guidelines.
home » blog » radiopharmaceuticals »