Summary: This article explores the core principles of radiotheranostics and radiotherapeutics in cancer, highlighting their unique methods, applications, and advantages in modern healthcare. It examines the historical context, discusses technological progress, and emphasises their impact on personalised medicine. Practical examples illustrate the differences and potential benefits for patients, clinicians, and researchers.
Keywords: Radiopharmaceuticals; Personalised Medicine; Imaging-Guided Therapy; Diagnostic Imaging; Targeted Radioisotopes; Oncology.
Introduction to Radioisotopes
The application of radioisotopes in medical care has evolved considerably over the past century. Early developments in radiation therapy heralded a shift in how clinicians approach cancer treatment, enabling them to direct ionising radiation at tumours in an effort to halt cancer cell proliferation. Over time, advances in nuclear medicine led to more uses of radioisotopes for both diagnostic imaging and targeted therapy. Out of these advancements emerged two related but distinct fields: radiotheranostics and radiotherapeutics.
Although both involve the use of radioactive substances, each field possesses unique features that have implications for disease diagnosis, patient management, and healthcare resource allocation. Radiotheranostics marries the twin modalities of diagnosis and treatment by using the same or closely related radiopharmaceuticals for imaging and therapy. Radiotherapeutics, on the other hand, is concerned primarily with the therapeutic application of radioisotopes to eradicate cancer cells. Understanding the difference between these fields is fundamental for any healthcare professional looking to stay informed about the rapidly changing sphere of nuclear medicine.
Historical Context
The history of radiation use in medicine begins at the turn of the 20th century, soon after the discovery of X-rays by Wilhelm Conrad Röntgen in 1895 and radioactivity by Henri Becquerel the following year. Marie and Pierre Curie’s work on radium and polonium provided the foundation for understanding how radioactive elements could influence biological tissues. Early clinical experiments revealed that high doses of ionising radiation could destroy tumour cells. However, research also highlighted the damage inflicted on healthy tissues if the radiation beam was not carefully targeted or the dose was not properly calibrated.
Subsequent decades witnessed the development of external beam radiotherapy (EBRT), in which linear accelerators deliver high-energy radiation to cancerous tissue from outside the body. This approach was a considerable step forward, but scientists soon realised that certain radiopharmaceuticals could localise in specific tissues. For instance, radioactive iodine-131 (I-131) readily accumulates in thyroid tissue, making it an excellent diagnostic and therapeutic tool for thyroid-related conditions. This led to the first glimpses of what we now refer to as radiotheranostics: using the same isotope for both imaging (to detect tumours) and therapy (to eliminate malignant cells).
Fast-forward to the modern era, the progression of nuclear medicine has taken on a more personalised dimension. Researchers developed various radiopharmaceuticals designed to localise in different tissues, each coupled with isotopes suitable for imaging (gamma or positron emitters) or therapy (beta or alpha emitters). These advancements led to two interrelated but distinct strategies for treating cancer: radiotheranostics and radiotherapeutics.
Defining Radiotheranostics
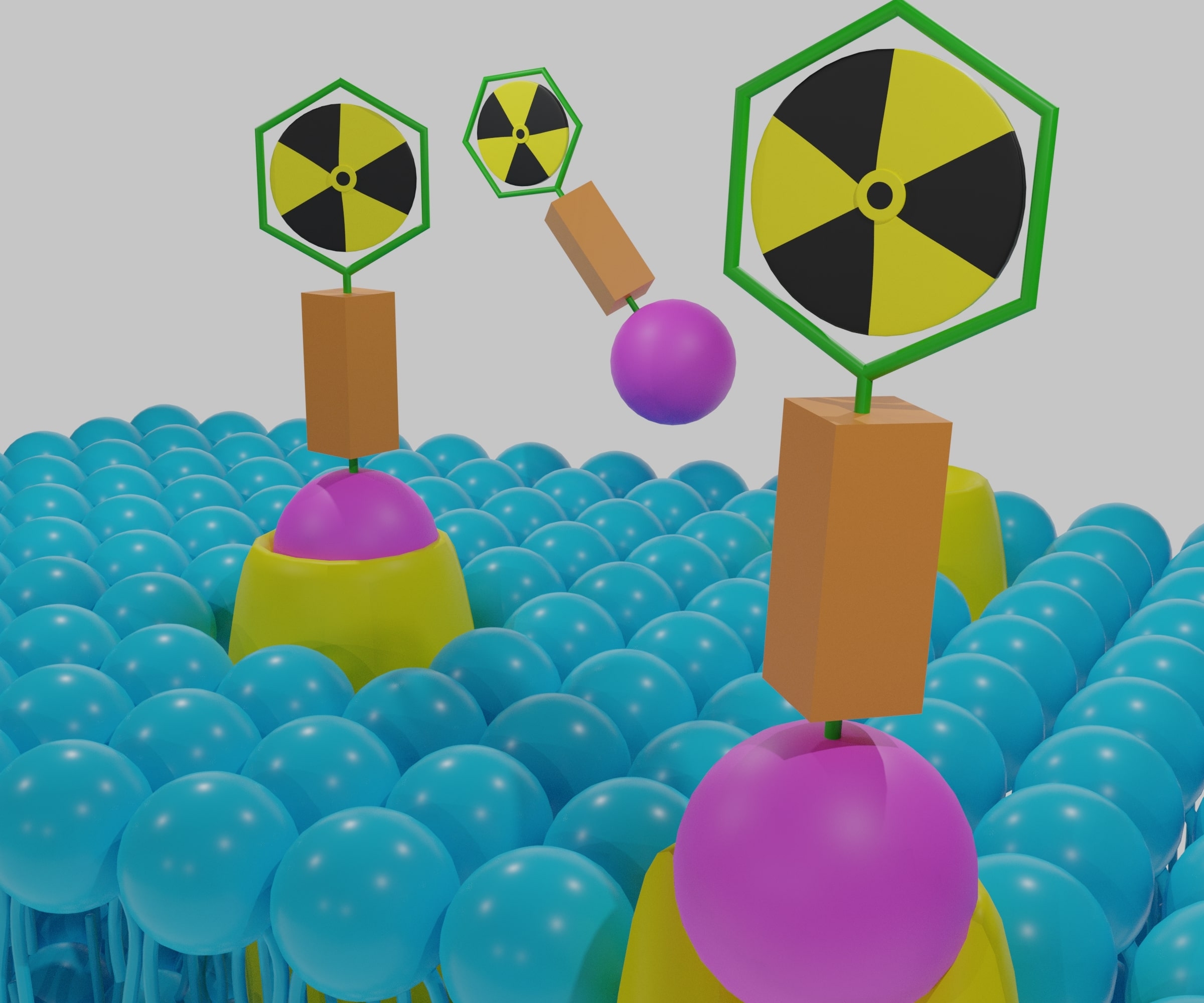
Radiotheranostics represents a combined strategy for diagnosing and treating diseases, mostly cancers, using specialised radiopharmaceuticals. Often, a molecule targeting a particular receptor on tumour cells is labelled with a diagnostic isotope, such as gallium-68 (Ga-68) or technetium-99m (Tc-99m), allowing clinicians to map where tumours have spread. Subsequently, the same molecule can be labelled with a therapeutic isotope, for example, lutetium-177 (Lu-177), to deliver radiation directly to malignant cells.
The defining aspect of radiotheranostics is this matching of diagnostic and therapeutic components. By using identical or closely related carrier molecules, one can often ensure that the tissue distribution for imaging will mirror the distribution for treatment. As a result, patients can undergo a screening scan to confirm that the radiopharmaceutical accumulates in the tumour, which increases the likelihood of successful therapy. If the diagnostic scan reveals minimal uptake in the tumour, then the therapy might be reconsidered, thus sparing patients from ineffective treatment and its associated side effects.
Advantages of Radiotheranostics
- Personalised Approach: Each patient’s tumour might have a specific molecular signature or receptor profile. Radiotheranostics enables clinicians to tailor treatment to individual tumour biology.
- Reduced Side Effects: Because the radioactive material predominantly targets cancer cells, healthy tissues experience less exposure to radiation.
- Improved Accuracy: Imaging scans confirm that the chosen radiopharmaceutical concentrates in the tumour before therapy is delivered. This minimises the risk of a patient receiving a less effective treatment plan.
- Streamlined Treatment Process: The same or a closely related compound can be used for both imaging and therapy, potentially simplifying production, regulation, and logistics.
Current Applications
Radiotheranostics has become most prominent in the management of neuroendocrine tumours (NETs) and prostate cancer. Agents such as gallium-68 DOTATATE for imaging and lutetium-177 DOTATATE for therapy have successfully pinpointed and treated neuroendocrine tumours. In the context of prostate cancer, radiolabelled PSMA (Prostate-Specific Membrane Antigen) ligands are used for PET imaging with gallium-68 or fluorine-18, followed by treatment with lutetium-177 PSMA ligands. Clinical trials and real-world evidence have shown encouraging outcomes, leading to increased adoption of these approaches in major cancer centres.
Defining Radiotherapeutics
Radiotherapeutics is the broader category of therapy involving radioactive substances. The principal aim is to destroy malignant cells by delivering ionising radiation internally, either systemically or locally. Unlike radiotheranostics, which hinges on the dual use of radiopharmaceuticals for diagnosis and treatment, radiotherapeutics focuses primarily on treatment. It may or may not incorporate a diagnostic step using the same radiopharmaceutical.
In many instances, radiotherapeutics might still rely on diagnostic imaging techniques (such as PET, CT, or MRI) for initial tumour localisation. Still, these imaging scans often employ different agents or rely on structural scanning rather than the same radiopharmaceutical. Furthermore, radiotherapeutics do not necessarily mandate that the therapeutic compound be used specifically for targeted imaging. Instead, the emphasis is placed on delivering a therapeutic isotope to kill or palliate cancerous lesions.
Main Categories of Radiotherapeutics
- Systemic Radiotherapy involves administering a radioactive compound that circulates throughout the body to address metastatic or widespread disease. Examples include I-131 for thyroid cancer and radium-223 for metastatic prostate cancer in bones.
- Locally Delivered Radioisotopes: Small radioactive sources (such as brachytherapy seeds) are placed within or near the tumour. While not always referred to under the same banner as ‘radiotherapeutics,’ brachytherapy is indeed a form of therapeutic radiation that uses sealed radioactive sources to eradicate tumour cells.
- Tumour-Targeted Radiopharmaceuticals: Similar to what is used in radiotheranostics, molecules such as peptides or antibodies are labelled with therapeutic isotopes. The difference here is that the same molecule might not be used for a preceding diagnostic scan.
Advantages of Radiotherapeutics
- Focused Treatment: When tumour-seeking carriers or local placement methods are used, radiation can be delivered where it is needed most, reducing harm to healthy tissues.
- Established Record: Many forms of radiotherapeutics, such as brachytherapy and iodine-131 for thyroid disorders, are well-studied and have been in clinical use for decades.
- Compatibility with Other Treatments: Radiotherapeutics can be administered alongside other therapies, such as chemotherapy or targeted agents, sometimes boosting overall therapeutic effectiveness.
Key Distinctions Between Radiotheranostics and Radiotherapeutics in Cancer
Integration of Diagnosis and Therapy:
- Radiotheranostics deliberately combines diagnostic and therapeutic processes, often employing the same or a similar radiopharmaceutical for imaging and treatment.
- Radiotherapeutics is primarily concerned with treatment. While clinicians might perform diagnostic imaging beforehand, it is not necessarily with the same or a closely related radiopharmaceutical.
Personalised Medicine Emphasis:
- Radiotheranostics aligns strongly with personalised medicine. Clinicians can tailor therapy by confirming the tumour’s affinity for the radiopharmaceutical through a diagnostic scan.
- Radiotherapeutics aims to destroy cancerous tissue using radioisotopes but does not always use a matching diagnostic compound beforehand.
Patient Selection:
- Radiotheranostics often involves a selection process where patients undergo a diagnostic scan to verify that the radiopharmaceutical localises in the tumour. Only those with positive scans typically proceed to therapy.
- Radiotherapeutics can be applied more broadly, depending on the known biology of cancer (for example, if it is known that thyroid tissue uptakes iodine).
Complexity of Protocols:
- Radiotheranostics may require a two-step or multi-step approach—imaging first, then therapy. This can lengthen the overall treatment timeframe and allow for careful patient-specific planning.
- Radiotherapeutics can be more straightforward in some clinical contexts. If a patient is diagnosed through standard imaging and is known to be a candidate for a particular radioactive therapy, the next step might be direct treatment.
Clinical Workflow and Expertise:
- Radiotheranostics demands close coordination among radiologists, nuclear medicine physicians, medical physicists, and oncologists. Research centres with well-developed nuclear medicine departments often lead to radiotheranostic protocols.
- Radiotherapeutics can sometimes be administered in a more conventional cancer care setting, although specialist input is always required.
Regulatory and Financial Considerations:
- Radiotheranostics may encounter additional approval processes due to the unique diagnostic and therapeutic components combination. Costs can be higher if reimbursement systems are not structured to recognise the unified approach.
- Radiotherapeutics has a longer track record, and some treatments (like I-131 for thyroid disease) are well established in healthcare systems worldwide. Hence, they might face fewer regulatory hurdles.
Current Trends and Future Directions
Improvements in Targeting Molecules: Ongoing research seeks to identify new peptides, antibodies, or small molecules that can bind exclusively or preferentially to receptors found on cancer cells. Peptide receptor radionuclide therapy (PRRT) has succeeded with neuroendocrine tumours, and investigations are expanding into other tumour types, such as breast, lung, and colon cancers. Antibodies, specifically monoclonal antibodies, are also being developed as vehicles for targeted radiation, offering the potential for more selective therapy.
Innovation in Radioisotopes: While beta-emitting isotopes such as I-131, Lu-177, and Yttrium-90 (Y-90) are the most commonly used in radiotherapeutics, alpha-emitting isotopes (e.g., Actinium-225, Radium-223) have garnered interest for their high-energy, short-range cytotoxic effects, meaning they can kill cancer cells effectively while sparing adjacent normal tissues. Alpha therapy is also being integrated into radiotheranostic protocols, broadening personalised radiomedicine’s scope.
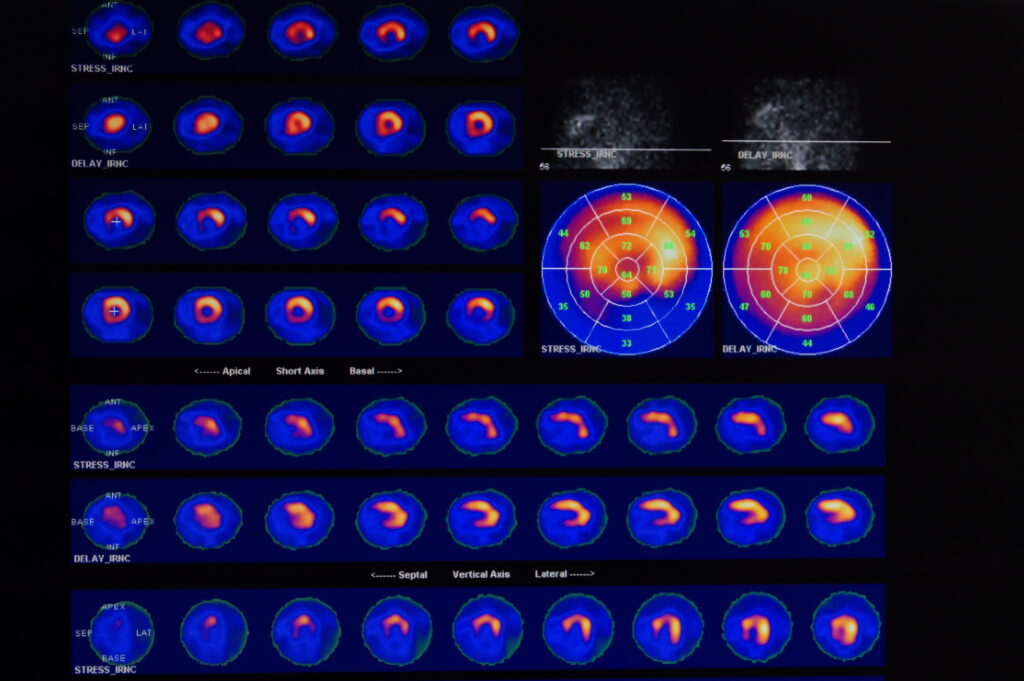
Theranostic Imaging Modalities: As diagnostic imaging technologies become more sensitive and specific, clinicians gain better insights into the tumour environment and disease burden. PET/CT and PET/MRI scanners provide high-resolution anatomical and metabolic data, improving the detection of cancer hotspots. These improvements feed directly into radiotheranostics, where the capacity to fuse PET images with therapy planning ensures that every joule of radiation is directed to the tumour.
Combination Therapies: Radiotheranostics and radiotherapeutics in cancer can be paired with other therapies, including immunotherapy, chemotherapy, and targeted agents like kinase inhibitors. By integrating different treatments, clinicians might achieve synergistic effects. Research is ongoing to determine the optimal ways to sequence or combine these therapies without incurring excessive toxicities. For example, some protocols involve using radiopharmaceuticals that sensitise tumours to chemotherapy or immunotherapy, potentially improving outcomes for patients with resistant or advanced-stage disease.
Accessibility and Cost: One major challenge in radiopharmaceutical therapy is ensuring access to patients worldwide. Radioisotopes require special handling and specialised facilities, which are often located in large medical centres. Production of short-lived isotopes also demands cyclotrons, nuclear reactors, or radionuclide generators, making distribution complex. Governments, academic institutions, and private companies are working together to expand production capacity and streamline regulatory hurdles, aiming to make these treatments available on a broader scale.
Patient-Centred Models of Care: With an increasing emphasis on patient satisfaction and quality-of-life metrics, radiopharmaceutical therapies have gained recognition for their potential to offer more targeted, less toxic cancer treatments. Patients typically experience fewer adverse effects compared to traditional chemotherapies, allowing them to maintain a higher quality of life during and after therapy. As a result, many hospitals are incorporating nuclear medicine clinics into their patient care pathways, ensuring that individuals have convenient access to advanced diagnostic and therapeutic options.
Comparison of Radiotheranostics and Radiotherapeutics
Below is a concise table comparing Radiotheranostics and Radiotherapeutics. It highlights their central focus, diagnostic steps, and clinical applications. This overview clarifies each method’s benefits and limitations, providing a clearer understanding of these two key approaches in modern nuclear medicine.
Conclusion
Radiotheranostics and radiotherapeutics are indispensable to modern cancer therapy. While radiotherapeutics has a solid foundation in oncology, radiotheranostics is forging new paths in personalised medicine by combining diagnosis and treatment into one integrated plan. By leveraging targeted radiopharmaceuticals, clinicians can identify tumours, gauge their suitability for treatment, and deliver therapy in a manner that reduces harm to healthy tissues.
For patients, the ongoing progress in both fields promises more effective and better-targeted treatments, which may translate into extended survival and improved quality of life. For clinicians, these innovations open up new diagnostic and therapeutic frontiers that demand a cross-disciplinary approach, bringing nuclear medicine experts, oncologists, and researchers together.
Healthcare systems, industry partners, and regulatory bodies must support the research, production, and distribution of new and existing radioisotopes. Collaborative efforts could help lower costs and streamline licensing processes, improving patient availability worldwide. Through innovation, collaboration, and responsible stewardship of radioactive resources, radiotheranostics and radiotherapeutics can reshape how cancer care is delivered.
With ongoing dedication to research, education, and patient-centred strategies, radiotheranostics and radiotherapeutics in cancer will remain at the forefront of targeted cancer therapy. These technologies demonstrate the versatility of nuclear medicine and underscore the fundamental shift toward treatments shaped by each patient’s unique molecular profile. As knowledge in the field grows, we can anticipate further refinements in both diagnosis and therapy, bringing us closer to cancer treatments that are increasingly precise, effective, and aligned with the goals of personalised medicine.
Q & A on Radiotheranostics and Radiotherapeutics
Q1: What are Radiotheranostics and Radiotherapeutics?
A1: Both involve using radioactive substances in medical treatment, primarily for cancer. Radiotheranostics combines diagnostic imaging and therapy in a single approach, using the same or very similar radiopharmaceuticals for both. Radiotherapeutics focuses on treatment only and may not always involve the same radioactive agent for diagnosis.
Q2: How do Radiotheranostics work in practice?
A2: First, a radiopharmaceutical labelled with a diagnostic radioisotope is administered to the patient. It attaches to targets on tumour cells, allowing imaging scans (such as PET) to confirm the tumour’s presence and uptake. If the scan shows that the radiopharmaceutical localises well, the diagnostic isotope is switched to a therapeutic one, delivering radiation directly to the tumour cells while sparing most healthy tissue.
Q3: In what types of cancer are Radiotheranostics commonly used?
A3: They are gaining popularity for neuroendocrine tumours and prostate cancer. For instance, gallium-68 DOTATATE scans can help locate neuroendocrine tumours, followed by lutetium-177 DOTATATE therapy. Similarly, gallium-68 or fluorine-18 labelled PSMA are used for prostate cancer imaging before lutetium-177 PSMA therapy.
Q4: How do Radiotherapeutics differ from Radiotheranostics?
A4: Radiotherapeutics focus on the therapeutic aspect, delivering radioactive material to target cancer cells. Although standard imaging may be used to detect tumours before treatment, radiotherapeutics do not necessarily rely on the same molecule for diagnosis and therapy. A good example is radioactive iodine-131 for thyroid cancer, which is well-established for treatment but can also be used diagnostically in certain cases.
Q5: What are the benefits of Radiotheranostics?
A5:
- Personalised approach: Patients receive tailored treatment based on the confirmed radiopharmaceutical uptake in their tumour.
- Improved accuracy: Diagnostic scans confirm suitability for therapy, reducing the risk of wasted treatment.
- Reduced side effects: Precisely targeting cancer cells helps spare healthy tissues.
- Streamlined process: The same or closely related compound can be used for both diagnosis and treatment
Q6: Are there any advantages unique to Radiotherapeutics in cancer?
A6: Radiotherapeutics have a well-established history with treatments like brachytherapy and iodine-131 for thyroid disorders. They can be simpler to implement in some scenarios, as they do not necessarily require a matching diagnostic agent for every patient. They can also work alongside chemotherapy, immunotherapy, or external beam radiotherapy, allowing integrated treatment strategies.
Q7: What is the role of patient selection in both methods?
A7:
- Radiotheranostics: Patients typically undergo a diagnostic scan with the intended radiopharmaceutical. If there is sufficient tumour uptake, the treatment proceeds.
- Radiotherapeutics: Selection is based on known cancer biology and location. If the tumour type is known to respond to a specific radiopharmaceutical (e.g., I-131 for thyroid cancer), clinicians can proceed with treatment without requiring a preceding scan of the same agent.
Q8: How do emerging trends affect Radiotheranostics and Radiotherapeutics in cancer?
A8: New targeting molecules and advancements in imaging technology enhance precision. There is growing interest in alpha-emitting isotopes like radium-223 and actinium-225 for their potent tumour-killing ability. Research on combination therapies (with immunotherapy or chemotherapy) is underway, aiming for even better clinical outcomes. Additionally, efforts are being made to expand production capacity and access so more patients can benefit.
Q9: Why is there so much interest in these approaches now?
A9: Nuclear medicine techniques have advanced significantly, offering more accurate imaging, safer handling of radioisotopes, and improved production methods. Patients benefit from targeted treatments that can result in fewer side effects and a better quality of life. As health services increasingly favour personalised treatments, Radiotheranostics and Radiotherapeutics align well with modern care priorities.
Q10: What does the future hold for Radiotheranostics and Radiotherapeutics?
A10: They will likely continue to grow, with new radiopharmaceuticals designed for various tumour types. Improved imaging and a deeper understanding of tumour biology will further refine these approaches, making them more precise. Ongoing research, interdisciplinary collaboration, and infrastructure investments will ensure wider adoption and success for patients worldwide.
Radiotheranostics and Radiotherapeutics each hold significant promise for cancer care. Radiotheranostics combines diagnosis and therapy in a single personalised pathway, while Radiotherapeutics targets tumours with radioactive substances to eradicate them. Both approaches form valuable components of modern oncology, with future innovations likely to expand their reach and improve patient outcomes.
Disclaimer
The content of this article is intended for informational and educational purposes only. It does not constitute medical advice, diagnosis, or treatment recommendations. Readers should not rely solely on the information provided herein when making healthcare decisions. Always seek the advice of qualified medical professionals regarding any medical condition or treatment options. The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of Open Medscience or any affiliated institutions. While every effort has been made to ensure the accuracy of the information presented, Open Medscience accepts no responsibility for errors, omissions, or any outcomes arising from the use of this material.