Summary: Emergency medicine is a critical field that addresses the immediate healthcare needs of patients experiencing acute illness or injury. This article explores the evolution, current challenges, and advancements in emergency medicine, from triage processes to the integration of telemedicine and artificial intelligence. Topics covered include pre-hospital care, trauma management, the role of emergency practitioners, and emerging technologies transforming emergency response. The piece also highlights the importance of a multidisciplinary approach in managing complex cases and the ongoing need for research and training in emergency settings.
Introduction to Emergency Medicine
Emergency medicine is a medical specialty focused on providing urgent and unscheduled care to patients experiencing acute illness, trauma, or other life-threatening conditions. Emergency departments (EDs) are the frontline in managing a diverse range of cases, from minor injuries to severe medical emergencies requiring immediate attention. The field has evolved considerably over the past few decades, with advancements in both clinical practice and technology.
Historical Context and Evolution
Emergency medicine, as a distinct field, developed in response to the growing demand for specialised, immediate care. Prior to its formal establishment, emergency care was typically handled by general practitioners or surgeons on call. The creation of dedicated emergency departments and the formal recognition of emergency medicine as a specialty in the 20th century brought a new focus on rapid, multidisciplinary care and the development of protocols designed to stabilise patients as quickly as possible. Today, emergency medicine encompasses a wide range of skills, requiring practitioners to have knowledge in fields such as internal medicine, trauma surgery, paediatrics, and psychiatry.
Key Principles of Emergency Medicine
Emergency medicine operates on several core principles that guide the care of patients in acute settings:
- Triage: Assessing the severity of a patient’s condition and prioritising care accordingly is fundamental in emergency settings. Triage ensures that resources are allocated effectively, especially in high-demand situations.
- Rapid Diagnosis and Treatment: Emergency medicine practitioners must quickly assess, diagnose, and begin treatment, often under challenging conditions where time is critical. This requires a combination of clinical expertise and decision-making skills.
- Multidisciplinary Approach: Effective emergency care often requires collaboration among various healthcare providers, including nurses, paramedics, radiologists, and specialist consultants, to provide comprehensive treatment for complex cases.
- Resource Management: Emergency departments often face resource limitations, and practitioners must work within these constraints to provide high-quality care.
- Adaptability and Resilience: Working in emergency medicine demands adaptability and resilience, as practitioners frequently encounter high-stress situations and unpredictable challenges.
Pre-Hospital Care: The First Line of Response
Pre-hospital care, provided by paramedics and emergency medical technicians (EMTs), is crucial in emergency medicine. This stage involves the initial assessment, stabilisation, and transportation of patients to appropriate healthcare facilities. Effective pre-hospital care can significantly impact patient outcomes, especially in cases of trauma, cardiac arrest, or stroke.
Key Components of Pre-Hospital Care
- Early Intervention: Administering life-saving interventions, such as CPR, defibrillation, and administering medication, can prevent further deterioration of the patient’s condition.
- Communication and Coordination: Pre-hospital care relies on seamless communication with hospital emergency departments to prepare for the patient’s arrival and ensure a smooth transition of care.
- Use of Technology: Advanced equipment, such as portable ventilators, defibrillators, and telemedicine support, enables paramedics to deliver high-quality care even before reaching the hospital.
Trauma Management and Critical Care
Trauma management is a primary responsibility in emergency medicine, given the high rates of road accidents, falls, and other traumatic incidents. Effective trauma care requires a structured approach, often following the Advanced Trauma Life Support (ATLS) guidelines, which focus on stabilising the patient’s airway, breathing, and circulation (the ABCs) before addressing secondary injuries.
Key Elements of Trauma Management
- Airway and Breathing Management: Ensuring an open airway and adequate ventilation is critical for trauma patients, as compromised breathing can lead to severe complications.
- Circulation and Haemorrhage Control: Uncontrolled bleeding is a leading cause of preventable deaths in trauma cases. Techniques such as applying pressure, tourniquets, and fluid resuscitation are used to control haemorrhage.
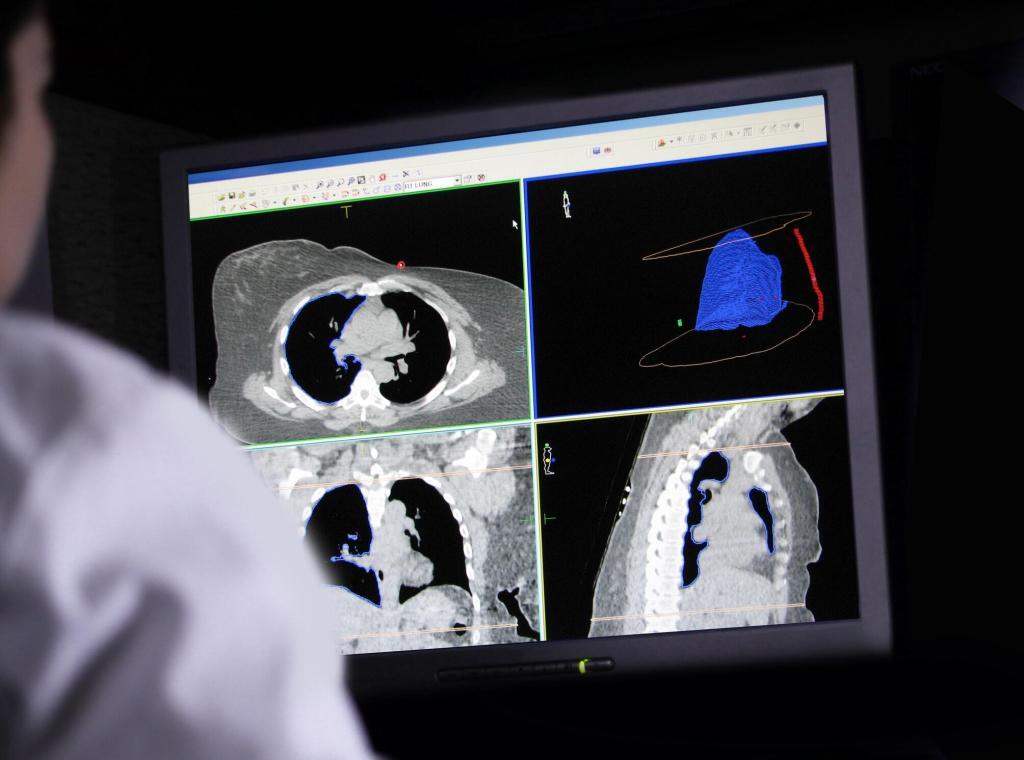
- Rapid Imaging and Diagnostics: Diagnostic tools such as X-rays, CT scans, and ultrasounds play an essential role in identifying internal injuries and guiding further treatment decisions.
- Surgical Interventions: Some trauma cases require immediate surgical intervention. In such cases, emergency departments often work closely with trauma surgeons to stabilise and manage injuries quickly.
The Role of Emergency Practitioners
Emergency practitioners are highly trained professionals who must be skilled in a variety of medical disciplines to handle the wide range of cases that are present in an ED. In addition to clinical skills, they need strong communication and leadership abilities, as they often coordinate teams and make rapid decisions that can have life-or-death consequences.
Responsibilities and Challenges
- Decision-Making Under Pressure: Emergency practitioners are frequently required to make quick decisions in high-stress situations, balancing the need for speed with the importance of accuracy.
- Emotional Resilience: Dealing with trauma, loss, and intense pressure can take a toll on practitioners. Emotional resilience is crucial, and many EDs are now providing psychological support to help staff cope with the demands of the job.
- Continuous Learning and Training: Given the rapid advancements in medical knowledge and technology, emergency practitioners must engage in ongoing education to stay updated on best practices.
Innovations in Emergency Medicine
Advancements in technology and medical research are continually transforming emergency medicine, improving patient outcomes, and enhancing the efficiency of care delivery.
Telemedicine and Remote Consultations
Telemedicine has revolutionised emergency care by allowing practitioners to consult with specialists remotely, providing expertise in real-time and aiding in faster decision-making. For instance, stroke patients in rural areas can now receive consultations from neurologists through telemedicine, expediting critical treatment decisions such as the administration of thrombolytic therapy.
Artificial Intelligence in Diagnostics
AI applications in emergency medicine are showing significant promise, particularly in diagnostic imaging and triage. AI algorithms can rapidly analyse imaging results, helping practitioners to identify issues like fractures, internal bleeding, or pulmonary embolisms with greater speed and accuracy. In some emergency departments, AI-powered triage systems assess patient symptoms and vital signs to determine the urgency of treatment, improving overall efficiency.
Point-of-Care Testing (POCT)
Point-of-care testing devices, which allow for rapid blood tests and other diagnostics directly in the ED, have improved the speed at which critical information is available. POCT is particularly beneficial for detecting issues like electrolyte imbalances, infections, and heart attacks, as it reduces the need for laboratory processing time.
Ethical and Legal Considerations in Emergency Medicine
Ethics plays a vital role in emergency medicine, where practitioners often face difficult decisions related to patient consent, allocation of limited resources, and end-of-life care. Legal considerations are also significant, as emergency departments are often involved in cases with potential liability issues.
Key Ethical Challenges
- Informed Consent: In emergency situations, it may not always be possible to obtain informed consent, particularly if the patient is unconscious or unresponsive. In such cases, practitioners must act in the patient’s best interests based on available information.
- Resource Allocation: During times of high demand, such as a natural disaster or pandemic, resources like ventilators, medication, and staff may be limited. Practitioners may need to make difficult decisions regarding who receives immediate treatment.
- Confidentiality and Privacy: Ensuring patient confidentiality can be challenging in the high-paced and often crowded environment of an ED. However, maintaining patient privacy is essential for ethical practice.
The Future of Emergency Medicine: Challenges and Opportunities
The future of emergency medicine holds both significant challenges and promising opportunities. With the global population ageing and rates of chronic disease rising, demand for emergency services is expected to increase, putting additional pressure on healthcare systems. Moreover, climate change and geopolitical factors may lead to new patterns of trauma and emergency needs, such as those related to natural disasters and conflict zones.
Addressing Workforce Shortages
Workforce shortages are a growing concern in emergency medicine. To address this issue, healthcare systems are investing in training programmes, improving working conditions, and exploring alternative staffing models, such as using nurse practitioners and physician assistants to support emergency practitioners.
Enhancing Preparedness for Public Health Crises
The COVID-19 pandemic underscored the need for emergency departments to be prepared for large-scale health crises. Future preparedness measures may include investing in surge capacity, establishing protocols for handling infectious disease outbreaks, and increasing stocks of essential medical supplies.
Continued Integration of Technology
Technology will continue to play a crucial role in the evolution of emergency medicine. Future innovations may include the development of smart ambulances, enhanced AI capabilities for diagnostics, and wearable devices that can transmit patient data directly to emergency teams en route to the hospital.
Conclusion
Emergency medicine is a dynamic and demanding field, requiring a blend of medical expertise, quick thinking, and resilience. While the field faces numerous challenges, particularly related to resource limitations and workforce demands, innovations in technology and an emphasis on multidisciplinary collaboration offer hope for improved outcomes and efficiency. As healthcare systems continue to evolve, emergency medicine practitioners will play a pivotal role in addressing the acute healthcare needs of patients worldwide, ensuring that no matter the circumstances, life-saving care is available when it is needed most. The future of emergency medicine will rely not only on technological advancements but also on a continued commitment to training, research, and ethical practices that prioritise patient welfare in the most critical of moments.
Disclaimer
The content presented in this article is for informational and educational purposes only. It does not constitute medical advice, diagnosis, or treatment and should not be relied upon as such. Open Medscience makes no representations or warranties regarding the accuracy, applicability, or completeness of the information provided. Readers should consult qualified healthcare professionals for any medical concerns or decisions.
Any views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of any affiliated institutions, healthcare providers, or regulatory bodies. Mention of specific technologies, practices, or treatments does not imply endorsement or suitability for all clinical settings.
Emergency medicine is a rapidly evolving field. While we aim to highlight current practices and innovations, the information may become outdated as new research and guidelines emerge. Open Medscience accepts no responsibility for any consequences arising from the use of the content herein.
home » blog » medicine »