Cancer care is entering a new era, where the traditional association between treatment and surgery is being challenged by technology once used only for diagnosis. Ultrasound — long known for imaging unborn babies and internal organs — is now being harnessed to treat tumours without incisions or invasive procedures. This transformation is not a distant prospect; it is unfolding in hospitals and research centres across the world, offering patients safer, quicker, and more precise alternatives to surgery.
From Imaging Tool to Therapeutic Powerhouse
For decades, ultrasound was purely diagnostic — a way to “see” inside the body. Therapeutic ultrasound takes this same principle and turns it into a treatment weapon. Instead of merely visualising tissue, it uses high-frequency sound waves to target and destroy tumour cells deep within the body.
The most established technique, known as High-Intensity Focused Ultrasound (HIFU), concentrates sound energy onto a pinpoint within a tumour. The focused energy rapidly raises the temperature in that exact spot, killing the cancer cells while leaving surrounding healthy tissue intact.
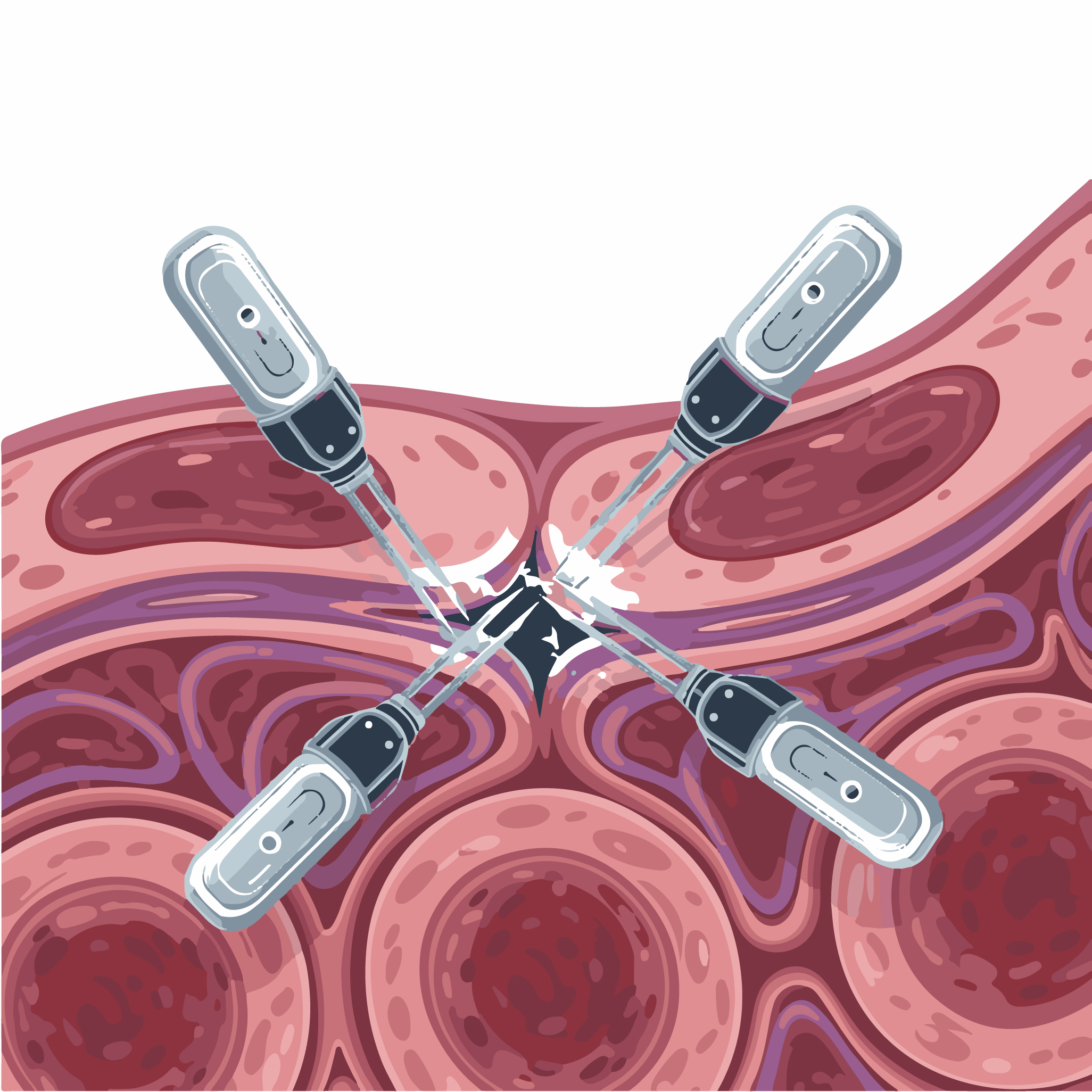
A newer technique, histotripsy, uses powerful sound pulses to create microscopic bubbles within the tumour. These bubbles expand and collapse, mechanically disrupting the cancer cells rather than heating them. The body then naturally clears away the damaged tissue.
These two methods represent a shift from the physical trauma of surgery to precision energy-based treatment, delivered entirely from outside the body.
How Ultrasound Destroys Cancer
HIFU works by focusing multiple ultrasound beams so that they intersect at a single focal point within the tumour. This focal region experiences intense heat — often over 60 °C — while the tissue through which the beams pass remains unharmed. The process is guided in real time using MRI or ultrasound imaging, allowing clinicians to visualise and adjust treatment as it happens.
Histotripsy, in contrast, harnesses the mechanical force of cavitation. High-amplitude sound waves generate tiny vapour bubbles in the tumour. When these bubbles collapse, they create mechanical shear forces that tear apart the cellular structure. This is often referred to as “mechanical ablation”, and its precision means that nearby blood vessels and nerves can remain untouched.
Because the procedure is non-invasive, the patient usually avoids general anaesthesia, hospital stays are short, and recovery is swift. What was once a major operation can now be performed in a treatment suite using real-time imaging and sound energy alone.
Current Uses in Cancer Treatment
In the UK, HIFU has been used primarily for prostate cancer, with encouraging results. It can target small, localised tumours and offers men a way to treat the disease while reducing side-effects such as incontinence and erectile dysfunction.
Research is expanding rapidly. Trials are underway exploring the use of HIFU and histotripsy in liver, breast, pancreatic, kidney, cervical, and brain cancers. The NHS has already started offering histotripsy for patients with liver tumours who are unsuitable for surgery.
In the United States, medical centres such as UC Davis Health have performed hundreds of successful HIFU treatments. Meanwhile, research teams are combining ultrasound with immunotherapy, using the sound waves not only to destroy tumours but also to stimulate the immune system to recognise and attack remaining cancer cells.
Why This Is a Breakthrough
The implications of ultrasound-based therapy go beyond avoiding surgery. It is a redefinition of how we think about cancer treatment.
First, it is non-invasive. There are no incisions, no blood loss, and minimal risk of infection. For many patients — particularly those who are older, medically fragile, or living with other conditions — this can be life-changing.
Second, ultrasound’s precision allows clinicians to focus energy only where it is needed. Healthy tissue surrounding the tumour is spared, greatly reducing side-effects and improving quality of life after treatment.
Third, the treatment can be repeated if necessary, something that is rarely possible with surgery or radiotherapy. This flexibility means ultrasound can be used not only for curative treatment but also for palliative care — reducing tumour burden, relieving pain, and improving comfort in advanced cases.
Finally, ultrasound therapy is a cost-effective, scalable solution for healthcare systems. With shorter recovery times and fewer hospital admissions, it aligns perfectly with the growing need for outpatient cancer care.
A Closer Look: Liver Cancer and Histotripsy
One of the most striking successes of ultrasound-based therapy is in the treatment of liver tumours. Traditionally, liver cancer surgery is complex and risky, and many patients are not eligible due to tumour location or poor liver function. Histotripsy changes this.
By directing focused ultrasound pulses from outside the body, clinicians can destroy tumours that were once unreachable by scalpel. The procedure typically lasts under an hour, requires no incision, and allows patients to go home the same day. Studies have shown that histotripsy can precisely target cancerous tissue while sparing vital blood vessels and bile ducts — an outcome rarely achieved through conventional methods.
For many patients, this represents the difference between having no viable treatment and receiving a therapy that can extend life while preserving quality of life.
The Challenges That Remain
As promising as therapeutic ultrasound is, it still faces hurdles before it becomes mainstream.
Not all tumours are suitable for ultrasound treatment. Deep-seated or large tumours can be difficult to reach, especially in organs that move during breathing, such as the liver or lungs. Sophisticated imaging and motion-tracking technology are helping overcome this challenge, but further refinement is needed.
Another issue is long-term efficacy. While short-term results are highly encouraging, researchers need longer follow-up data to compare recurrence and survival rates with traditional surgery or radiotherapy.
There are also practical barriers — the equipment is expensive, the technique requires specialist training, and integration into national health systems takes time. Yet these obstacles are already being addressed through international research collaborations and new technology investments.
Beyond Destruction: Ultrasound and the Immune System
Perhaps the most exciting development is the growing recognition that ultrasound can do more than simply ablate tumours. When tumour cells are destroyed by ultrasound, they release fragments and antigens into the bloodstream, effectively flagging the immune system to respond.
Scientists are exploring ways to combine ultrasound with immunotherapy, turning the treatment into a form of “in situ vaccination”. In experimental models, ultrasound has been shown to enhance the delivery of cancer drugs, activate immune cells, and improve the body’s natural ability to fight off residual cancer.
A research team at the University of Southern California has even developed engineered immune cells that can be activated by ultrasound. Once triggered, these cells continue to seek and destroy cancerous tissue days after treatment — an approach that could one day lead to long-lasting remission.
What It Means for Patients
For individuals diagnosed with cancer, the psychological burden of facing surgery is immense. The prospect of a surgery-free treatment that can eliminate tumours with minimal side-effects offers new hope and empowerment.
Patients recover faster, experience less pain, and often return to normal activities within days. For many, the treatment is performed as an outpatient procedure, meaning they can go home the same day. The emotional impact of avoiding hospitalisation and lengthy recovery should not be underestimated — it restores a sense of control and normality during an otherwise daunting time.
In cancers such as prostate, liver, and breast, where ultrasound therapy is advancing most rapidly, patient satisfaction scores are high. Many report that they would recommend the treatment to others, citing both the physical comfort and the dignity it preserves.
A Glimpse of the Future
The story of ultrasound in cancer therapy is only beginning. Researchers are exploring combinations of ultrasound with targeted drugs, nanoparticles, and immune-based therapies. Each advance brings the vision of personalised, incision-free cancer care closer to reality.
Future systems will likely integrate artificial intelligence to automatically guide treatment, adjusting energy levels and beam focus in real time based on patient anatomy and tumour response. The same technology that once produced simple grey-scale images will become an intelligent therapeutic platform — capable of treating disease with millimetre precision.
For healthcare systems, the potential savings and efficiency gains are immense. For patients, it represents a gentler, more humane form of medicine. The scalpel may not disappear entirely, but its dominance in cancer treatment is being re-evaluated by something once thought too gentle for the task: sound.
Conclusion
Ultrasound is emerging as one of the most transformative forces in modern oncology. It turns invisible sound waves into a powerful, precise, and compassionate tool for healing — a way to treat cancer without cutting the body open. From HIFU to histotripsy, from prostate to liver tumours, it is proving that the future of cancer care may lie not in surgery, but in sound.
This new generation of ultrasound therapy offers more than medical innovation; it offers patients the promise of recovery without trauma, healing without scars, and hope delivered not by the surgeon’s hand, but by waves of sound.
Disclaimer
The content provided in Sound Without Scalpels: How Ultrasound Is Transforming Cancer Treatment is intended for general informational and educational purposes only. It should not be interpreted as medical advice, diagnosis, or a recommendation for any specific treatment. Readers should not rely on this information to make decisions about their health or medical care.
All medical procedures, including those involving ultrasound-based therapies such as High-Intensity Focused Ultrasound (HIFU) and histotripsy, should be discussed with qualified healthcare professionals who can provide guidance based on individual circumstances and medical history.
While every effort has been made to ensure the accuracy and timeliness of the information presented, Open MedScience makes no representations or warranties, express or implied, regarding the completeness, reliability, or suitability of the content. Research in medical imaging and therapeutic technologies is continually evolving, and clinical practices may vary by region or institution.
Open MedScience, its contributors, and affiliates accept no liability for any loss, injury, or damage arising directly or indirectly from the use of, or reliance on, the information contained in this publication.
For personalised medical advice or treatment options, please consult your doctor or another qualified healthcare professional.
home » blog » medical imaging news »