MRI-Guided Radiotherapy
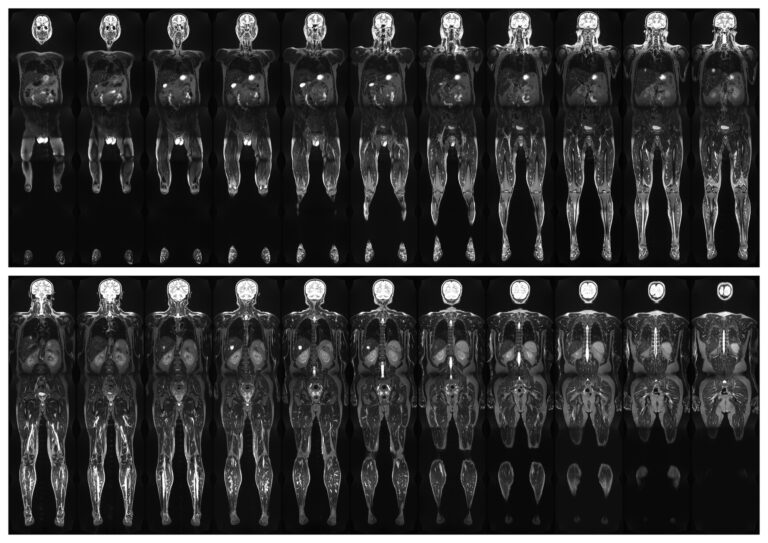
Magnetic Resonance Imaging (MRI)-guided radiotherapy represents a significant technological advancement in the field of oncology, offering unparalleled precision in targeting tumours while sparing healthy tissues. Combining the superior imaging capabilities of MRI with the therapeutic potential of radiotherapy, this approach addresses key challenges associated with conventional treatment modalities, such as limited tumour visualisation and organ motion management.
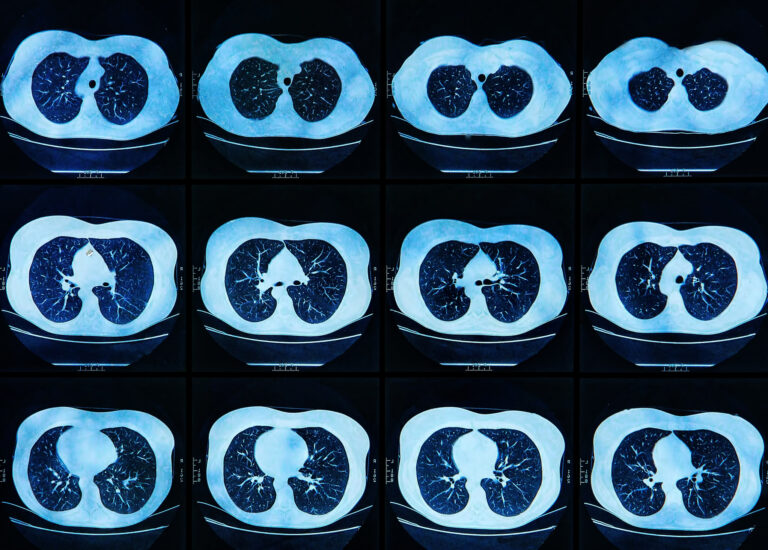
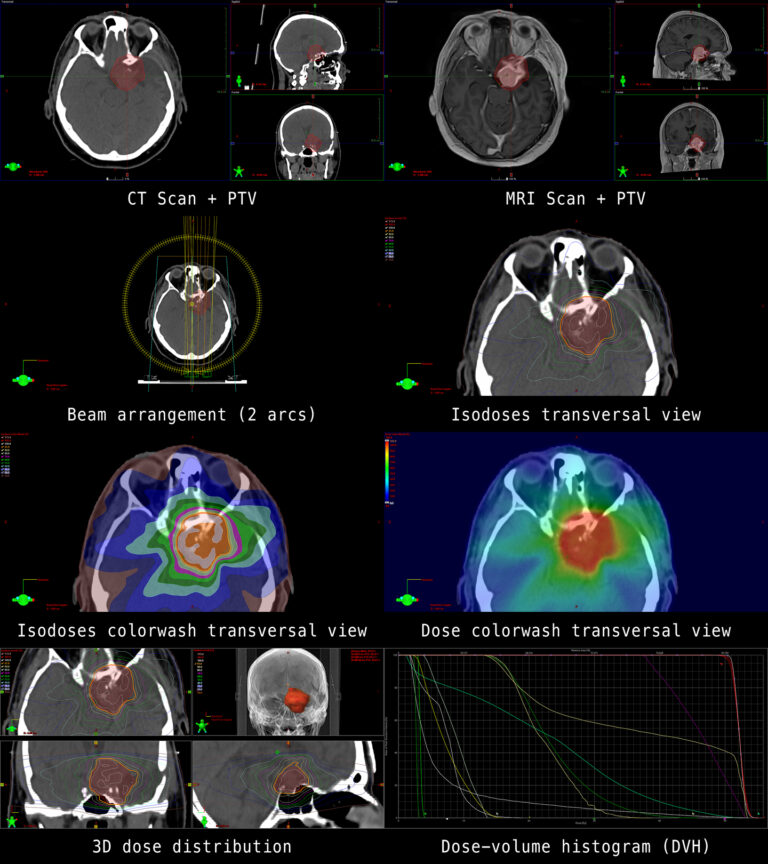
Traditional radiotherapy relies heavily on computed tomography (CT) for treatment planning and delivery. While effective, CT scans often lack the soft tissue contrast necessary to distinguish tumours from surrounding healthy structures, particularly in anatomically complex areas. MRI, with its exceptional soft tissue imaging, overcomes this limitation, enabling clinicians to more accurately define tumour boundaries and adapt treatment plans in real time.
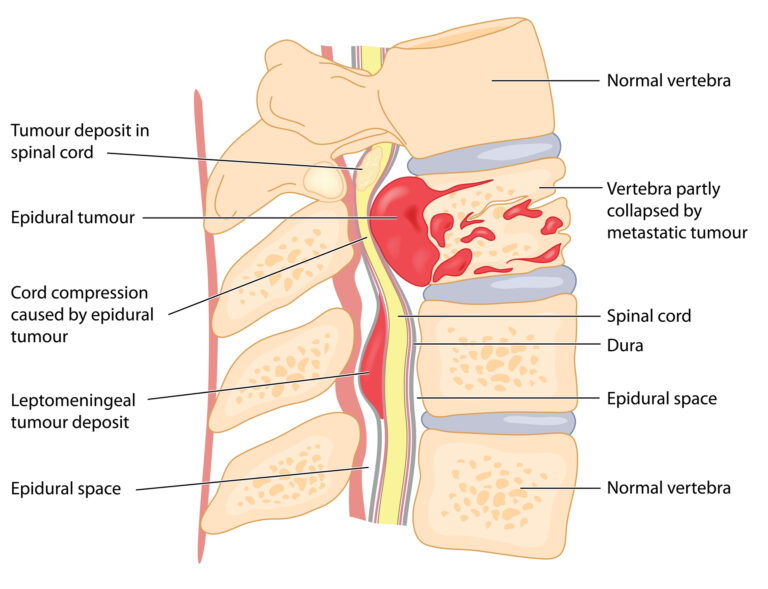
The integration of MRI with linear accelerators (LINACs) has given rise to MRI-guided radiotherapy systems, such as the MR-Linac. These systems allow simultaneous imaging and treatment, enabling real-time monitoring of tumour and organ motion during radiation delivery. This capability is especially beneficial for tumours located in areas subject to significant physiological movement, such as the lungs, abdomen, and pelvis. By continuously visualising the treatment area, clinicians can adjust radiation beams dynamically, ensuring precise targeting even in response to patient breathing or other involuntary movements.
One of the key advantages of MRI-guided radiotherapy is its ability to facilitate adaptive radiotherapy. This approach involves modifying treatment plans during the course of therapy to account for changes in tumour size, shape, or position, as well as variations in surrounding anatomy. Adaptive radiotherapy ensures that each session is tailored to the patient’s current condition, maximising therapeutic efficacy while minimising damage to healthy tissues.
MRI-guided radiotherapy has shown promising results in the treatment of various cancers, including pancreatic, prostate, and liver cancers. For example, the ability to visualise and adjust for organ motion has significantly improved outcomes in pancreatic cancer, a condition previously challenging to treat due to its proximity to critical structures.
Despite its advantages, the widespread adoption of MRI-guided radiotherapy faces several challenges. These include the high cost of equipment, the need for specialised facilities, and the requirement for multidisciplinary expertise in imaging, physics, and clinical oncology. However, ongoing research and technological developments are expected to address these barriers, making this cutting-edge treatment more accessible.
In conclusion, MRI-guided radiotherapy represents a paradigm shift in cancer treatment, offering unprecedented precision and adaptability. As the technology continues to evolve, it holds the potential to transform outcomes for patients with complex or difficult-to-treat cancers, reinforcing the role of innovation in advancing modern oncology.
You are here:
home » MRI-Guided Radiotherapy