Summary: Early detection of lung cancer has long been a major challenge, especially when dealing with small or difficult-to-reach nodules in the lungs. Robotic-assisted lung biopsy aims to address this challenge through precise navigation, enhanced manoeuvrability, and improved imaging capabilities. By obtaining tissue samples more accurately and safely, clinicians can reduce waiting times for conclusive diagnoses, offer targeted treatments sooner, and potentially improve long-term patient outcomes in the fight against lung cancer.
Keywords: Robotic technology; Early detection; Minimally invasive; Lung biopsy; Oncology; Clinical outcomes.
Introduction to Lung Cancer
Lung cancer remains one of the leading causes of cancer-related deaths worldwide. A significant part of this tragic statistic stems from patients being diagnosed once the cancer has already progressed to advanced stages. In such scenarios, treatment options can become limited, and the prognosis is often poor. One of the primary reasons for late diagnosis is the inherent difficulty in detecting and sampling lung nodules, especially if they are small or located in challenging sections of the lung. Fortunately, ongoing developments in medical technology are changing how doctors approach lung cancer diagnosis. Robotic-assisted lung biopsy has emerged as a cutting-edge technique that promises to enhance diagnostic accuracy and enable earlier detection.
Traditional biopsy methods can be cumbersome, involving either a needle biopsy performed through the chest wall or a bronchoscopy guided by a flexible scope. Although these techniques have made significant contributions to lung cancer care for years, they can be limited by certain factors. For instance, needle biopsies may pose a higher risk of complications such as pneumothorax, particularly if the nodule is situated deep in the lung tissue. Traditional bronchoscopies, on the other hand, might not always permit direct access to very small nodules or those in complicated segments of the bronchial tree. By integrating robotic systems, clinicians may overcome these obstacles, offering patients a more precise, reliable, and potentially safer pathway to diagnosis.
Robotic-assisted lung biopsy involves sophisticated tools that allow specialists to navigate the airways more accurately, obtaining adequate tissue samples for pathological examination. This improved accuracy can potentially reduce the number of repeat procedures needed, diminish patient anxiety, and speed up treatment decisions. In this discussion, we will explore how lung cancer develops, why early diagnosis poses such a challenge, the mechanics of robotic-assisted lung biopsies, their benefits, potential drawbacks, and what the future may hold for these advanced medical systems.
Understanding Lung Cancer
Lung cancer occurs when abnormal cells in the lung begin to multiply uncontrollably, forming a tumour that can disrupt normal respiratory function. It can also spread (metastasise) to other organs, further complicating treatment. There are two main forms of lung cancer: non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). NSCLC represents the majority of diagnoses, comprising subtypes such as adenocarcinoma, squamous cell carcinoma, and large cell carcinoma.
Identifying the precise type of lung cancer is essential for determining the best treatment approach. For example, targeted therapies are particularly relevant for certain gene mutations in NSCLC, while SCLC often requires more aggressive treatment, such as chemotherapy and radiotherapy. In every case, detecting lung cancer at the earliest possible stage is key to improving survival rates. However, obtaining a tissue sample in early lung cancer can be an uphill task because nodules often remain small and do not always display overt symptoms.
Another factor contributing to the complexity of diagnosing lung cancer is the airways’ structure. The lungs comprise a maze of bronchial passages, each branching into progressively smaller segments. A suspicious lesion may be located in a segment that is difficult to access using conventional biopsy methods. Moreover, because some nodules fail to cause clear symptoms, they can go unnoticed until they have significantly enlarged or spread; at this point, the available treatments might be less effective.
The Challenges of Early Diagnosis
Several major hurdles often hamper early diagnosis of lung cancer. First, the majority of individuals with early lung cancer do not exhibit prominent or specific symptoms. Coughing, mild chest discomfort, and shortness of breath can be easily mistaken for more benign conditions such as respiratory infections or underlying chronic lung diseases. Patients might only seek medical attention once their symptoms escalate without conclusive early indicators, making an early and accurate diagnosis challenging.
Second, imaging studies like chest X-rays or CT scans might reveal suspicious nodules that need further investigation. However, confirming whether a nodule is malignant depends on obtaining a sample of the suspicious tissue. Traditional methods of accessing the lungs for sampling can sometimes be limited. A needle biopsy through the chest wall can help in retrieving cells, but it carries a risk of accidental damage to surrounding lung tissue, potentially leading to air leaks or bleeding. Moreover, very small nodules might be located in areas that are not straightforward to reach without increasing the chances of complications.
Third, bronchoscopy procedures are relatively safe and have guided diagnostic protocols for decades. Yet, the design of a conventional bronchoscope might not always enable the operator to guide it with enough precision in the deeper bronchial network, especially when dealing with tiny nodules or those situated in anatomically tricky positions. This limitation may lead to inconclusive samples or the need for multiple biopsies, prolonging the diagnostic process and adding additional stress for patients.
Robotic-assisted lung biopsy tackles these drawbacks by fusing imaging, robotics, and advanced navigation tools. Doctors can diagnose lung cancer earlier and with greater certainty by delivering a more refined approach to sampling tissue. This technique aligns with modern healthcare’s emphasis on patient-centred treatment, expediting the route to answers and ensuring minimal discomfort.
Robotic-Assisted Lung Biopsy: How It Works
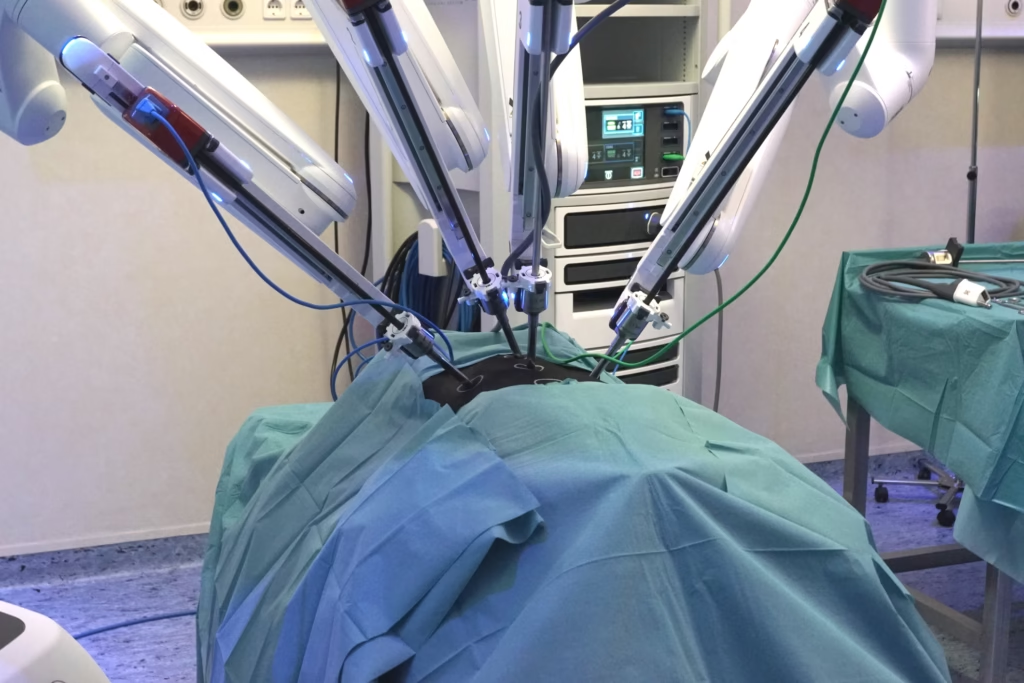
A robotic-assisted lung biopsy can be understood as the integration of robotic arms, miniature scopes, and advanced navigation software that work in harmony to guide a biopsy tool into the precise location of the lung nodule. The procedure typically begins with a high-resolution CT scan of the patient’s chest, capturing detailed images of the tumour’s structure and location. These images are then fed into the robotic system’s software, which constructs a three-dimensional map of the airways.
With a clear digital model in hand, the clinician can plot the path to the targeted lesion. The robotic arm is designed to move steadily and with a high degree of control, eliminating the slight hand tremors or limitations that might be encountered during a conventional bronchoscopy. Using a combination of real-time imaging, positional feedback, and predefined pathways, the system can deliver the biopsy instrument precisely where it needs to go.
One of the major breakthroughs of robotic-assisted procedures lies in the improved visualisation of the lung’s internal structures. The flexible scope’s camera view typically limits traditional bronchoscopy, but the robotic system’s software can merge different imaging modalities, enabling the operator to track the biopsy instrument’s position in real-time. Some platforms use electromagnetic navigation technology, which works like a GPS for the lungs. This helps the medical team adjust their approach on the spot, ensuring they reach the target with enhanced precision.
When the biopsy tool is in place, a sample of the suspected tissue is taken. This tissue is then sent to pathology for close examination under the microscope. Depending on the findings, additional tests, such as molecular profiling for certain genetic mutations in the tumour cells, can be performed. These details help clinicians recommend the most effective therapies for each individual patient. Through this streamlined approach, robotic-assisted lung biopsy aims to reduce the number of procedures a patient must undergo and hasten the time to a definitive diagnosis.
Advantages and Possible Drawbacks
Advantages
Greater Diagnostic Accuracy: By combining precise navigation and stable robotic control, clinicians can gather samples from the exact regions of interest. This higher level of accuracy often leads to more definitive results, reducing the need for follow-up biopsies.
Early Detection: Because the robotic systems can access small nodules in tricky areas of the lung, there is a better chance of detecting cancer while it is still in an early stage. Early-stage lung cancer carries a much better prognosis, especially if treatments such as surgery, radiotherapy, or targeted therapies can be initiated promptly.
Less Invasive and Quicker Recovery: The minimally invasive nature of robotic-assisted lung biopsy frequently results in fewer complications compared to surgical biopsy techniques. Most procedures are performed through the natural airways, circumventing the need for large incisions. This means less pain, a lower likelihood of infection, and a faster return to normal activities.
Reduced Anaesthesia Time and Hospital Stay: Because of its targeted approach, a robotic-assisted biopsy can shorten the length of the procedure and hospital stay, making it more cost-effective for healthcare providers as well as more convenient for patients. Shorter procedures often mean reduced exposure to anaesthetics, mitigating certain risks associated with prolonged sedation.
Improved Patient Confidence: Many patients feel reassured knowing that cutting-edge technology is being used to diagnose their condition. This positive outlook can lessen anxiety and contribute to a more comfortable healthcare experience. Clear, high-resolution images and real-time navigation often provide them with visual confirmation that the process is targeted and thorough.
Possible Drawbacks
Cost and Resource Allocation: One of the primary concerns about any new medical technology is cost. Robotic systems are typically expensive to purchase, maintain, and upgrade. Healthcare institutions must weigh the long-term benefits of better diagnostic accuracy against the initial financial outlay. Accessibility may be restricted, especially in smaller hospitals or regions with limited healthcare budgets.
Steep Learning Curve: Although the introduction of robotic systems aims to simplify certain aspects of the procedure, clinicians need specialised training to navigate them effectively. A learning curve is inevitable, which might lead to variability in diagnostic accuracy while practitioners gain experience. Institutions must invest in robust training programmes and ensure medical staff are proficient in operating the equipment.
Potential for Technology Glitches: No technology is immune to malfunction. Although robotic platforms for lung biopsies are generally reliable, unexpected software or hardware issues can occur. Contingency plans, backup systems, and appropriate protocols are essential to maintain patient safety and avoid procedure disruptions.
Lack of Universal Availability: Large teaching hospitals and dedicated cancer centres may have the resources to offer robotic-assisted lung biopsy, but access might be limited in smaller or rural healthcare settings. This can create disparities in care, with some patients lacking the opportunity to benefit from advanced diagnostic methods.
The Future of Robotic-Assisted Lung Biopsies
Robotic-assisted lung biopsy is likely to continue evolving, both in terms of the technology itself and the ways it fits into wider clinical practices. For instance, future improvements in imaging capabilities could refine the robotic system’s ability to pinpoint suspicious nodules even more accurately. Higher-resolution scans, combined with novel contrast agents, could enable clinicians to differentiate between benign and malignant nodules faster, minimising invasive procedures for patients who do not require them.
In addition, ongoing research into artificial intelligence (AI) could reshape how biopsies are performed. AI-powered algorithms might assist in identifying promising routes within the airways, optimising the approach, and estimating the likelihood that a nodule is cancerous. By feeding the robotic system data in real-time, AI could automatically adjust the biopsy path and guide clinicians around problem areas. This level of automation might reduce procedure times and further elevate accuracy.
Potential expansions on the robotic-assisted biopsy platform include integrated treatment options. For instance, if a lesion is confirmed as malignant during the procedure, future systems may be equipped with tools to administer local therapy. This could involve delivering specialised drugs or applying energy-based treatments directly to the tumour site. Although such integrated approaches are still in the early investigative stages, they suggest a movement towards a model of lung cancer care that is both more personalised and more immediate.
Collaboration among medical professionals, engineers, and software developers will be key to advancing this field. As robotic systems become more intuitive and possibly more affordable, it is plausible that community hospitals and smaller clinics will also have access to this technology. This shift could level the playing field for early lung cancer diagnosis, giving more patients a chance to benefit from these sophisticated tools.
Conclusion
Lung cancer is a serious public health concern, mainly because it is often detected at later stages. Timely detection is crucial to improving a patient’s treatment options and potential outcomes. Robotic-assisted lung biopsy represents a significant leap forward in reaching nodules that would otherwise be difficult to access. By merging robotics, three-dimensional imaging, and advanced navigation software, this technique aims to deliver more accurate sampling, shorten hospital stays, and alleviate patient stress.
The capacity to acquire a precise and complete tissue sample, even from small or complicated nodules, enhances diagnostic clarity and accelerates the decision-making process for treatment. Although its introduction requires substantial financial investment and well-trained personnel, many clinicians believe that the net benefit to patient care justifies these costs. As the technology evolves, it may become an integral part of standard diagnostic pathways, helping identify cancer earlier than possible.
From the patient’s perspective, robotic-assisted lung biopsy can bring peace of mind at a difficult time. Undergoing fewer procedures, avoiding multiple exposures to sedation, and receiving results quickly can transform what is often a nerve-racking wait. In addition, clear-cut pathology findings enable oncologists to develop tailored treatment plans, thereby improving the likelihood of successful outcomes.
As the fusion of robotics and AI progresses, new avenues for diagnosis and possibly even immediate treatments within the same procedure might emerge. The goal is to offer a more holistic approach to lung cancer care that rapidly, accurately, and safely addresses each patient’s needs. In essence, robotic-assisted lung biopsy is helping to shift the diagnostic process from a game of catch-up towards a more proactive, precise, and patient-friendly approach—an innovation that holds promise for transforming lung cancer care well into the future.
Disclaimer
The content provided in this article is for informational and educational purposes only. It is not intended to replace professional medical advice, diagnosis, or treatment. The technologies, techniques, and procedures discussed—including robotic-assisted lung biopsy—may not be suitable for all patients or available in all clinical settings. Decisions regarding medical care should always be made in consultation with qualified healthcare professionals familiar with the specific circumstances of the patient.
Open MedScience does not endorse any particular product, device, or medical provider mentioned in the article. While efforts have been made to ensure the accuracy of the information at the time of publication, advances in research or changes in clinical guidelines may render parts of this article outdated. Readers are encouraged to consult current clinical resources and healthcare professionals before making any decisions based on the content herein.
home » blog » medical robotics »