Magnetic Resonance Imaging (MRI) is a powerful diagnostic tool that provides detailed internal images of the human body. However, interpreting these images can be complex and requires a foundational understanding of anatomy, MRI technology, and image analysis. This brief guide will walk you through the basic principles of reading an MRI scan, from understanding the types of images produced to recognising normal anatomy and identifying common pathologies. The article also includes a history of MRI, providing context for how this technology has evolved.
Introduction to MRI Technology
Magnetic Resonance Imaging (MRI) is a non-invasive diagnostic tool that uses magnetic fields and radio waves to create detailed images of the body’s internal structures. Unlike X-rays or CT scans, MRI does not use ionising radiation, making it safer for repeated use. Understanding how MRI technology works is crucial for interpreting the images it produces.
The History of MRI
The development of MRI is a story of scientific innovation spanning several decades, involving contributions from multiple fields, including physics, chemistry, and medicine.
Early Foundations (1930s-1970s)
- Nuclear Magnetic Resonance (NMR) Discovery: The foundational principle behind MRI, known as Nuclear Magnetic Resonance (NMR), was discovered in the 1930s. Physicists Isidor Rabi, Felix Bloch, and Edward Purcell were instrumental in this discovery. Rabi demonstrated that atomic nuclei could absorb and re-emit radio waves when placed in a magnetic field, a concept that would later be critical to MRI technology. Bloch and Purcell expanded on Rabi’s work and were awarded the Nobel Prize in Physics in 1952 for their discoveries concerning NMR.
- Medical Application Conceptualised: In the early 1970s, researchers began exploring the potential medical applications of NMR. Dr. Raymond Damadian, an American physician and scientist, proposed that NMR could be used to detect cancerous tissues, as they produced different NMR signals compared to healthy tissues. In 1971, Damadian published a paper demonstrating that cancerous tissues could be distinguished from normal tissues using NMR, laying the groundwork for what would become MRI.
Development of MRI Technology (1970s-1980s)
- First MRI Images: In 1973, Paul Lauterbur, an American chemist, expanded on Damadian’s work by introducing the concept of using gradients in the magnetic field to generate two-dimensional images. This breakthrough enabled the spatial localisation of NMR signals, allowing for the creation of images. Lauterbur’s work marked the transition from NMR spectroscopy to MRI imaging.
- Further Refinements: Around the same time, Sir Peter Mansfield, a British physicist, further refined MRI technology by developing mathematical techniques that made it possible to create detailed images more quickly. Mansfield’s improvements in gradient techniques significantly reduced the scan time and improved image resolution.
- First Human MRI Scan: The first MRI scan of a human was performed in 1977 by Raymond Damadian and his team, marking a significant milestone in medical imaging. The scan took nearly five hours to complete but demonstrated the potential of MRI as a diagnostic tool.
- Nobel Prize: In 2003, Paul Lauterbur and Sir Peter Mansfield were awarded the Nobel Prize in Physiology or Medicine for their contributions to the development of MRI. Notably, Raymond Damadian was controversially excluded, leading to considerable debate within the scientific community.
Advancements and Modern MRI (1990s-Present)
- Widespread Adoption: By the 1980s and 1990s, MRI had become a widely used tool in medicine, with advancements in technology leading to faster scan times, higher resolution images, and the development of new imaging sequences and techniques.
- Functional MRI (fMRI): In the 1990s, functional MRI (fMRI) was developed. It allows for the visualisation of brain activity by detecting changes in blood flow and has since become a crucial tool in neuroscience research.
- High-Field MRI: The introduction of high-field MRI scanners (such as 3 Tesla and later 7 Tesla) has provided even greater image resolution and has enabled more detailed studies of brain and body structures, further expanding the clinical and research applications of MRI.
Today, MRI is an indispensable tool in medical diagnostics. It provides unparalleled detail of soft tissues, the brain, and the spinal cord and offers insights into both structural and functional aspects of the body.
Understanding MRI Anatomy
Before interpreting any abnormalities on an MRI scan, it is essential to be familiar with normal anatomy as seen in different sequences.
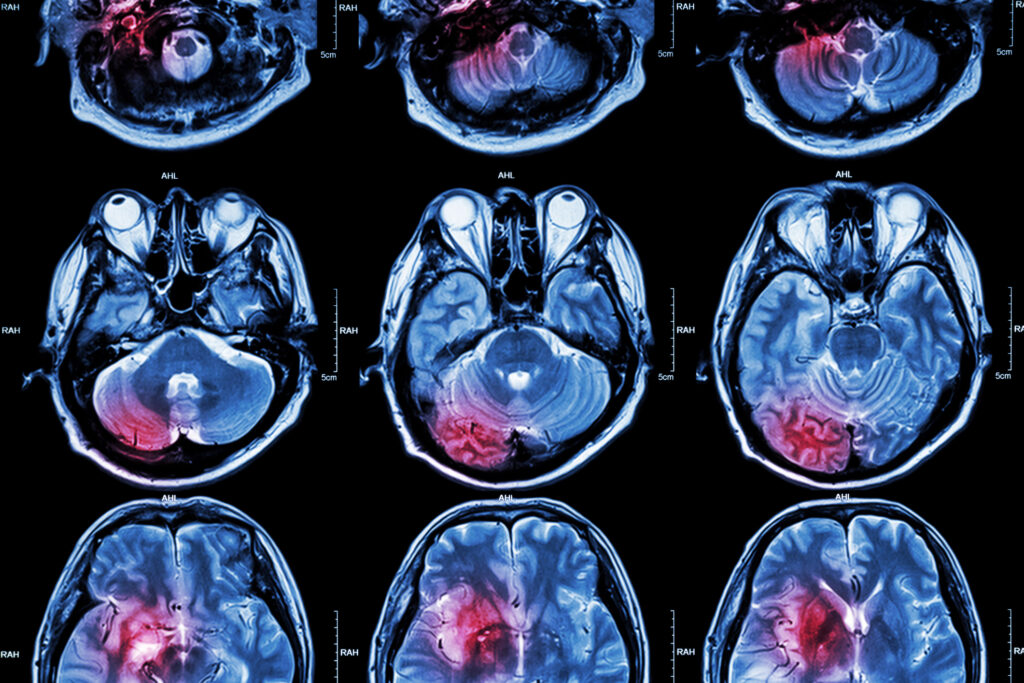
Brain MRI Anatomy
When viewing a brain MRI, it is crucial to identify key structures and differentiate between grey matter, white matter, and cerebrospinal fluid.
- Grey Matter: This appears darker on T1-weighted images and brighter on T2-weighted images.
- White Matter: This appears brighter on T1-weighted images and darker on T2-weighted images.
- Cerebrospinal Fluid (CSF): This appears very dark on T1-weighted images and bright on T2-weighted images.
Key anatomical landmarks in brain MRI include the cerebral cortex, ventricles, brainstem, and major sulci and gyri. Familiarising yourself with these structures on different sequences is crucial for identifying any deviations from the norm.
Spinal MRI Anatomy
Spinal MRI scans are primarily used to evaluate the vertebrae, spinal cord, and intervertebral discs. Key points to focus on include:
- Vertebrae: These should appear as block-like structures on sagittal images, with the intervertebral discs visible as dark spaces between them on T1-weighted images.
- Spinal Cord: This appears as a cylindrical structure running through the vertebral canal, with CSF surrounding it.
- Intervertebral Discs: These appear bright on T2-weighted images and are crucial for assessing disc herniation or degeneration.
Step-by-Step Approach to Reading an MRI Scan
Interpreting an MRI scan requires a systematic approach to avoid missing any important findings. Below is a step-by-step guide that you can follow when analysing an MRI.
Review Patient History and Clinical Context
Before examining the images, always review the patient’s history and clinical presentation. Understanding the context can guide your interpretation and help you focus on relevant areas. For example, if a patient presents with symptoms of a stroke, you would pay particular attention to the Diffusion-Weighted Imaging (DWI) sequence.
Choose the Appropriate Sequence
Different sequences provide different information. Select the sequence that best addresses the clinical question. For instance:
- Use T1-weighted images for detailed anatomical information.
- Use T2-weighted images to assess for fluid or oedema.
- Use FLAIR to detect lesions in the brain that are not apparent on T2-weighted images due to CSF suppression.
Start with an Overview of the Entire Scan
Begin by reviewing the entire scan, moving from one slice to another. This will help you get a sense of the structures’ general condition and ensure you don’t overlook any large or obvious abnormalities.
Evaluate Each Structure Systematically
Adopt a systematic approach, examining each structure in turn. For a brain MRI, this could involve:
- Evaluating the cerebral hemispheres: Check for symmetry, abnormal signals, or mass effects.
- Assessing the ventricles: Ensure they are of normal size and shape, without signs of hydrocephalus or midline shift.
- Reviewing the brainstem and cerebellum: Look for lesions or structural abnormalities.
For a spinal MRI, each vertebra and disc is examined, checking for alignment, disc height, and signal changes in the spinal cord.
Compare Different Sequences
Cross-referencing findings across different sequences is crucial. For example, if you identify a bright spot on a T2-weighted image, check the same area on a T1-weighted image. This can help distinguish between different types of tissue and fluid and can aid in the diagnosis.
Identify Any Abnormalities
Look for common abnormalities, such as:
- Lesions: These could indicate tumours, infections, or demyelination.
- Atrophy: A reduction in the size of brain structures, often seen in neurodegenerative diseases.
- Haemorrhages: Identified by areas of signal loss on Gradient Echo (GRE) sequences.
- Herniation: In spinal MRI, look for disc material that has protruded into the spinal canal.
Correlate Findings with Clinical Symptoms
Once you have identified potential abnormalities, correlate them with the patient’s clinical symptoms. This will help you determine the relevance of your findings and guide further management.
Recognising Common Pathologies on MRI
Understanding how common pathologies appear on MRI is essential for accurate diagnosis. Below are some of the most frequent conditions seen on MRI.
Brain Tumours
Brain tumours can present in various ways depending on their location, size, and type. Common features to look for include:
- Mass Effect: Displacement of brain structures due to the size of the tumour.
- Enhancement: After the administration of contrast, tumours often enhance due to increased vascularity.
- Oedema: Surrounding areas of high signal on T2-weighted images indicating swelling.
Stroke
MRI is highly sensitive for detecting acute stroke, particularly with Diffusion-Weighted Imaging (DWI).
- Acute Stroke: It appears as an area of restricted diffusion on DWI, often accompanied by a corresponding low signal on Apparent Diffusion Coefficient (ADC) maps. This helps in the early detection and management of stroke, which is crucial for patient outcomes.
- Chronic Stroke: Over time, areas affected by a stroke may appear as encephalomalacia, which shows up as regions of increased signal on T2-weighted images and a loss of brain volume. Identifying these areas is important for understanding the long-term effects of a stroke.
Multiple Sclerosis (MS)
Multiple Sclerosis (MS) is a chronic disease characterised by the formation of demyelinating plaques in the central nervous system. MRI is the most sensitive tool for detecting these plaques, especially in the brain and spinal cord.
- T2 Hyperintense Lesions: In MS, these plaques often appear as areas of increased signal on T2-weighted images, particularly in the periventricular, juxtacortical, and infratentorial regions. The distribution and size of these lesions are key to diagnosing and monitoring the progression of MS.
- FLAIR Sequences: FLAIR is particularly useful in highlighting these lesions because it suppresses the cerebrospinal fluid signal, making the plaques stand out more clearly. This sequence is crucial for diagnosing MS and monitoring disease activity.
Disc Herniation
Disc herniation is a common cause of back pain and can lead to nerve root compression. MRI is the imaging modality of choice for assessing disc herniation because it provides excellent visualisation of soft tissues.
- Protrusion of Disc Material: On MRI, a herniated disc is seen as the protrusion of disc material into the spinal canal. This is best visualised on sagittal T2-weighted images, where the herniated portion of the disc will appear bright against the darker background of the spinal cord and surrounding tissues.
- Nerve Root Compression: The MRI can also show the effect of the herniated disc on adjacent nerve roots, which may appear compressed or displaced. This is particularly important for surgical planning and determining the need for intervention.
Hydrocephalus
Hydrocephalus is a condition where there is an abnormal accumulation of cerebrospinal fluid (CSF) within the brain’s ventricles, leading to increased pressure and potential damage to brain tissues.
- Ventricular Enlargement: The hallmark of hydrocephalus on MRI is the enlargement of the brain’s ventricles. This can be clearly seen on T2-weighted images where the CSF appears bright, and the ventricles are significantly larger than normal.
- Periventricular Oedema: In cases of elevated intracranial pressure, you might also see high signal intensity around the ventricles on T2-weighted images, indicating periventricular oedema. This finding is important for assessing the severity of hydrocephalus and the urgency of treatment.
Advanced MRI Techniques
Beyond basic sequences, advanced MRI techniques provide additional insights into various conditions and are increasingly important in both clinical practice and research.
Functional MRI (fMRI)
Functional MRI (fMRI) measures brain activity by detecting changes associated with blood flow. It is primarily used in research and pre-surgical planning.
- Activation Maps: During fMRI, areas of the brain that are active during a specific task or in response to a stimulus show increased blood flow, which is detected as a signal change. These activation maps are crucial for identifying brain functional areas that should be preserved during neurosurgery.
Magnetic Resonance Angiography (MRA)
Magnetic Resonance Angiography (MRA) is used to visualise blood vessels and detect vascular abnormalities such as aneurysms or stenosis.
- Flow Voids: On T2-weighted images, flowing blood often appears dark, creating voids that correspond to the vessels. MRA provides a non-invasive way to assess the patency and structure of blood vessels, which is critical for diagnosing and treating conditions like atherosclerosis and aneurysms.
Diffusion Tensor Imaging (DTI)
Diffusion Tensor Imaging (DTI) measures the directional movement of water molecules, allowing for the visualisation of white matter tracts in the brain. This technique is particularly useful in studying brain connectivity and assessing white matter integrity in conditions such as multiple sclerosis or after traumatic brain injury.
- Fibre Tractography: DTI allows the reconstruction of the brain’s white matter tracts, which can help identify disruptions due to lesions or tumours. These images can be invaluable in pre-surgical planning to avoid critical tracts during neurosurgery.
Perfusion-Weighted Imaging (PWI)
Perfusion-Weighted Imaging (PWI) measures the passage of blood through brain tissue, providing information about cerebral blood flow, cerebral blood volume, and mean transit time. This is especially useful in the context of stroke and brain tumours.
- Ischaemic Penumbra: In stroke imaging, PWI can help identify areas of the brain that are at risk but potentially salvageable, known as the penumbra. These areas show reduced perfusion but may not yet be infarcted, making them a target for acute intervention.
Common Pitfalls in MRI Interpretation
Interpreting MRI scans can be challenging, and several common pitfalls can lead to misdiagnosis. Being aware of these pitfalls is essential for accurate interpretation.
Motion Artifacts
One of the most common issues in MRI interpretation is motion artefacts, which occur when the patient moves during the scan. These artefacts can create blurring or ghosting effects on the images, making them difficult to interpret accurately.
- Solutions: If motion artefacts are severe, the scan may need to be repeated. Ensuring the patient is comfortable and well-informed about the importance of staying still can help reduce these artefacts.
Partial Volume Effects
Partial volume effects occur when different tissues within a single voxel (the smallest unit of a 3D image) are averaged together, leading to misleading signals.
- Solutions: Using thinner slices or higher resolution sequences can reduce partial volume effects, allowing for more precise localisation of abnormalities.
Susceptibility Artifacts
Susceptibility artefacts are distortions that occur due to the presence of metallic objects or air-tissue interfaces within the body. These artefacts are particularly problematic in areas such as the skull base or near surgical implants.
- Solutions: To minimise susceptibility artefacts, use sequences like Fast Spin Echo (FSE) instead of Gradient Echo (GRE), and remove any metallic objects from the patient before scanning.
Misinterpretation of Normal Variants
Normal anatomical variants can sometimes be mistaken for pathological conditions. For example, prominent perivascular spaces in the brain can mimic small infarcts on certain sequences.
- Solutions: Familiarity with common anatomical variants and a thorough comparison of findings across multiple sequences can help avoid misinterpretation.
Overlooking Small Lesions
Small lesions, such as microbleeds or small tumours, can be easily overlooked, especially in complex scans with many slices.
- Solutions: A systematic approach to reviewing every slice in multiple planes and sequences can help ensure that no small but significant findings are missed.
Practical Tips for MRI Interpretation
To improve your skills in MRI interpretation, consider the following practical tips:
Practice Regularly
Interpreting MRI scans is a skill that improves with practice. Reviewing a wide variety of cases regularly will help you become more familiar with normal anatomy and the range of possible pathologies.
Use Reference Materials
Access to reference materials, such as anatomy textbooks, atlases, or online resources, can be invaluable when encountering unfamiliar findings.
Collaborate with Colleagues
Discussing challenging cases with more experienced colleagues or specialists can provide new insights and help confirm your findings.
Stay Updated
MRI technology and techniques are continually evolving. Staying updated with the latest developments in the field through continuing education, conferences, or reading current literature will enhance your interpretative skills.
Take a Systematic Approach
Always follow a systematic approach to ensure that you review every aspect of the scan. This reduces the risk of missing important findings and ensures a thorough evaluation.
The Future of MRI Interpretation
The field of MRI interpretation is rapidly evolving, with new technologies and techniques constantly being developed. Here are some trends and future directions that may shape the way we interpret MRI scans in the coming years.
Artificial Intelligence (AI) and Machine Learning
Artificial intelligence and machine learning are beginning to play a significant role in the interpretation of MRI scans. AI algorithms can be trained to recognise patterns in MRI data, potentially identifying abnormalities faster and with greater accuracy than human interpreters in some cases.
- Benefits: AI can assist in detecting subtle abnormalities, improving diagnostic accuracy, and reducing the workload for radiologists by pre-screening scans and highlighting areas of concern.
- Challenges: The integration of AI into clinical practice requires extensive validation, and there are concerns about over-reliance on AI at the expense of clinical judgment. Ethical and legal implications, such as the responsibility for errors, also need to be addressed.
3D Imaging and Visualisation
Advancements in 3D imaging and visualisation techniques are making it possible to view MRI scans in more intuitive ways. 3D reconstructions allow for improved understanding of complex anatomy and pathologies, particularly in planning surgical interventions.
- Applications: 3D visualisation is particularly useful in neurosurgery, orthopaedic surgery, and vascular interventions, where a detailed understanding of spatial relationships is crucial for successful outcomes. Manipulating 3D models of anatomical structures allows surgeons to better understand how to approach complex cases, thereby reducing the risk of complications.
- Interactive Platforms: Interactive 3D platforms are being developed to allow for the real-time manipulation of MRI data, providing an immersive experience that can enhance both learning and clinical decision-making. These platforms are particularly useful in educational settings, allowing students and professionals to explore anatomy and pathologies in a more hands-on manner.
High-Resolution MRI
High-field MRI scanners, such as 7 Tesla (7T) MRI, are pushing the boundaries of image resolution, providing unprecedented detail of anatomical structures.
- Advantages: Higher resolution can lead to better characterisation of small structures and subtle abnormalities, which may be particularly beneficial in early diagnosis of diseases like multiple sclerosis or Alzheimer’s. These scanners allow for more precise imaging of fine structures within the brain, nerves, and other soft tissues, improving the detection and understanding of microstructural changes associated with various conditions.
- Limitations: Higher-field MRI systems are more expensive and may not be widely available. Due to the stronger magnetic field, they also come with increased susceptibility to artefacts and patient discomfort. However, ongoing technological advancements are expected to mitigate some of these challenges, making high-field MRI more accessible and comfortable for patients.
Functional and Molecular Imaging
The future of MRI may also involve a shift towards functional and molecular imaging, which focuses not just on anatomy but also on the biochemical processes within tissues.
- Functional MRI (fMRI): Beyond mapping brain activity, fMRI is being explored for its potential to understand complex neurological disorders and psychiatric conditions by studying the brain’s functional connectivity. This could lead to better treatment strategies and more targeted interventions for conditions like depression, schizophrenia, and epilepsy.
- Molecular Imaging: Techniques are being developed to visualise specific molecules or metabolic processes within the body, which could lead to earlier diagnosis of conditions like cancer, even before structural changes are apparent. Molecular MRI could revolutionise personalised medicine by enabling the monitoring of disease progression and response to therapy at the molecular level.
Telemedicine and Remote Interpretation
The rise of telemedicine is likely to impact MRI interpretation as well, with radiologists reviewing more scans remotely.
- Benefits: Remote interpretation allows for access to expert opinions regardless of geographic location, improving the quality of care in underserved areas. It enables radiologists to consult on cases from anywhere in the world, ensuring that patients receive the best possible diagnostic insights, even in areas with limited resources.
- Challenges: Ensuring the security of patient data and maintaining communication between remote radiologists and on-site clinicians are critical considerations. Additionally, the development of robust systems for transmitting and interpreting MRI scans remotely while maintaining image quality and diagnostic accuracy is essential for the success of telemedicine in this field.
The table below summarises the key MRI sequences, their primary uses, and the typical appearance of various tissues in each sequence.
| MRI Sequence | Primary Use | Appearance of Tissues |
| T1-Weighted Imaging | Detailed anatomical information | – Fat: Bright – Water/Fluid: Dark – White Matter: Bright – Grey Matter: Dark |
| T2-Weighted Imaging | Highlighting fluid, oedema, and pathological changes | – Fat: Dark – Water/Fluid: Bright – White Matter: Dark – Grey Matter: Bright |
| FLAIR (Fluid Attenuated Inversion Recovery) | Identifying lesions in the brain by suppressing CSF | – Fat: Dark – Water/Fluid (CSF): Dark – Lesions: Bright (particularly useful for detecting multiple sclerosis plaques) |
| DWI (Diffusion-Weighted Imaging) | Detecting acute stroke, cellular changes | – Acute Stroke/Infarct: Bright (restricted diffusion) – Chronic Stroke: May appear dark on ADC maps |
| GRE (Gradient Echo) | Detecting blood products, haemorrhages, calcifications | – Blood Products: Dark (signal loss) – Calcifications: Dark (signal loss) |
| PWI (Perfusion-Weighted Imaging) | Assessing cerebral blood flow and volume | – Ischaemic Areas: Reduced perfusion – Normal Brain Tissue: Normal perfusion |
| fMRI (Functional MRI) | Mapping brain activity, research applications | – Active Brain Areas: Show increased signal due to higher blood flow during specific tasks or stimuli |
| MRA (Magnetic Resonance Angiography) | Visualising blood vessels, detecting vascular abnormalities | – Flowing Blood: Appears as flow voids (dark areas) – Aneurysms/Stenosis: Can be visualised clearly |
| DTI (Diffusion Tensor Imaging) | Visualising white matter tracts, brain connectivity | – White Matter Tracts: Visualised as directional coloured lines – Disruptions: Alterations in tract integrity can indicate disease or injury |
Conclusion
Reading and interpreting MRI scans is a complex but essential skill in modern medicine. It requires a deep understanding of both the technology behind MRI and the normal and pathological anatomy as visualised on different sequences. By adopting a systematic approach, staying updated with the latest advancements, and continuing to practice and collaborate with others, healthcare professionals can significantly improve their ability to accurately interpret MRI scans.
As MRI technology continues to advance, the tools and techniques available for interpreting these scans will become even more sophisticated, allowing for earlier and more precise diagnosis of a wide range of conditions. Whether you are a medical student, a junior radiologist, or an experienced healthcare professional, continuing to develop your skills in MRI interpretation is essential for providing the best possible care to your patients. The integration of advanced imaging techniques, AI, and high-resolution scanners promises to enhance the diagnostic capabilities of MRI further, opening new possibilities for personalised medicine and improved patient outcomes.
Disclaimer
The information presented in this article, “Understanding How To Read An MRI Scan: A General Guide,” is intended solely for general educational purposes and should not be construed as medical advice, diagnosis, or a substitute for professional consultation with a qualified healthcare provider.
MRI interpretation is a complex process that requires extensive medical training and clinical experience. While this guide aims to introduce the basic concepts of MRI technology and image interpretation, it is not intended to equip readers with the skills necessary to make clinical judgments or interpret scans independently.
Readers must not attempt to interpret their own or others’ MRI scans based on this article. Any medical concerns or questions arising from an MRI scan should be addressed directly with a licensed radiologist or medical professional. Open Medscience accepts no responsibility for any decisions or actions taken based on the content of this guide.
Always seek the advice of your doctor or other qualified health provider with any questions you may have regarding a medical condition or imaging result.
home » blog » medical imaging modalities »