X-rays have revolutionised modern medicine, providing a non-invasive way to peer inside the human body to diagnose fractures, infections, tumours, and a range of other medical conditions. Over the course of more than a century of use, the science behind X-rays and radiation exposure has become well-established and rigorously regulated. However, occasional confusion still arises from lesser-known or misunderstood terms. One such term that has surfaced in both scientific discussions and public speculation is “dark radiation.”
This article aims to explore the concept of dark radiation, its relevance to X-ray imaging, and how it differs from standard radiation forms. It also examines why a proper understanding of radiation is essential in the context of medical diagnostics and public health. It also clarifies some of the myths and misconceptions surrounding radiation exposure and outlines the measures taken to maintain safety in clinical practice.
The Origins of the Term “Dark Radiation”
The term “dark radiation” does not originate in medical physics or radiology. Instead, it comes from theoretical physics and cosmology. In cosmological models, dark radiation is proposed as a type of hypothetical radiation that, like dark matter, does not interact with light in the same way as ordinary matter does. It cannot be directly observed through traditional electromagnetic means, such as visible light or radio waves, and is inferred from its effects on the expansion of the universe or on gravitational behaviour.
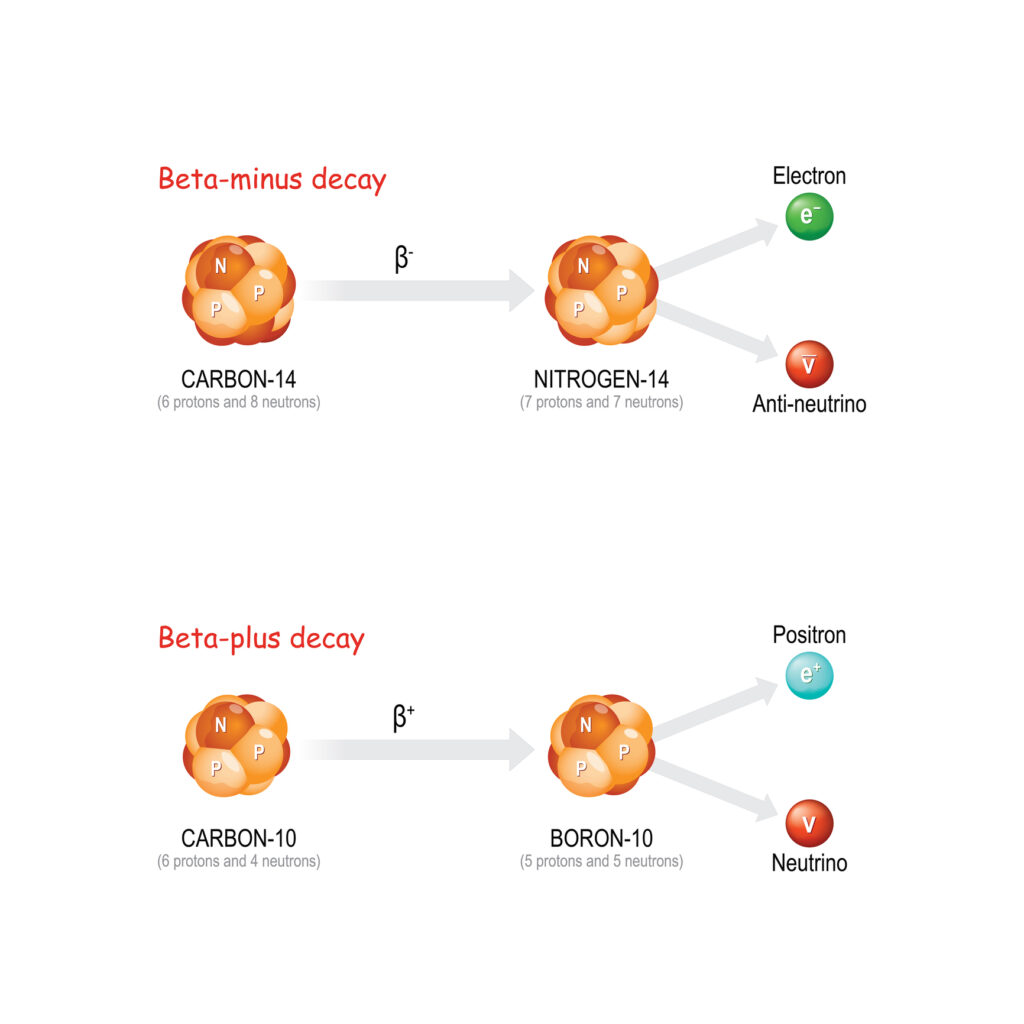
In these contexts, dark radiation is often considered as a potential energy component related to light, nearly massless particles like neutrinos. Some cosmological models suggest that there may be unknown particles or forces contributing to the universe’s total energy balance, which have yet to be directly observed. However, this concept belongs firmly within the area of cosmology, string theory, and high-energy particle physics, rather than in practical medical imaging or clinical diagnostics.
When the term “dark radiation” is invoked in relation to X-rays or radiology, it often causes confusion. In medical contexts, it is sometimes used informally or inaccurately to refer to forms of radiation that are not visible to the naked eye, or to scattered or secondary radiation that does not contribute directly to image formation. This usage is scientifically imprecise and risks misleading people into thinking there are unknown or hidden dangers present in routine imaging procedures.
The Physics of X-rays
To understand why “dark radiation” is irrelevant in clinical radiography, it is helpful first to explain how X-rays are generated and used in medicine.
X-rays are a form of electromagnetic radiation, similar in nature to light but with far shorter wavelengths and much higher energy. These rays are produced artificially in an X-ray tube, where high-speed electrons are fired at a metal target, usually made of tungsten. When the electrons collide with the atoms in the target, they lose energy rapidly, and this energy is emitted in the form of X-ray photons.
Once produced, the X-ray beam is directed at the part of the patient’s body being examined. As the beam passes through the body, different tissues absorb varying amounts of radiation. Dense tissues such as bone absorb more X-rays and appear white on the resulting image, while softer tissues absorb less and appear in shades of grey. Air-filled spaces, such as the lungs, allow most of the X-rays to pass through and thus appear black on the image.
The key point here is that all the radiation used in this process is electromagnetic in nature, specifically ionising radiation, which is a well-understood physical phenomenon. There is no known or proposed mechanism by which an additional, hidden type of radiation – so-called dark radiation – would play any role in this process.
Different Types of Radiation in X-ray Imaging
In clinical practice, radiologists and radiographers classify radiation involved in imaging into different categories, all of which are measurable and accounted for using established physical laws and instrumentation.
The first is primary radiation, which refers to the main beam of X-rays that travels from the tube towards the patient. This is the radiation that passes through the body and creates the diagnostic image.
Next, there is secondary or scattered radiation. As X-rays interact with matter, especially within the body, they can be deflected in different directions. This scattered radiation does not contribute usefully to the image and can reduce image quality or increase exposure to people nearby. This is why shielding, such as lead aprons or walls, is used to minimise exposure.
Another form is leakage radiation. This refers to a minimal amount of radiation that may escape from the X-ray tube housing in directions other than the primary beam. Modern machines are designed to keep this to negligible levels.
Finally, background radiation is naturally present in our environment, originating from cosmic rays, radon gas, and radioactive materials in the Earth’s crust. Although not part of the imaging process, background radiation is a vital consideration when evaluating total cumulative exposure over time.
None of these forms of radiation is hidden or mysterious. All are well-characterised, and their effects have been extensively studied over decades. Medical physics departments routinely monitor and regulate these exposures to ensure they remain within safe limits. There is no additional “dark” component that eludes detection or poses unknown risks.
Misinterpretation of “Dark” as “Unknown” or “Hidden”
The reason the term “dark radiation” occasionally surfaces in public discourse about medical imaging is due in part to the everyday meaning of the word “dark.” In common language, dark implies something unseen or hidden. When patients hear about radiation that is “invisible” or cannot be felt, they may understandably become concerned that there is something harmful occurring beyond the awareness or control of medical staff.
However, in the context of physics, the term “dark” in “dark radiation” or “dark matter” refers to forms of energy or mass that do not emit, absorb, or reflect light, and therefore cannot be directly observed with electromagnetic instruments. It does not mean that they are harmful, undetectable in principle, or ignored by scientists. In fact, extensive research efforts are underway in astrophysics to detect and characterise such phenomena.
In medical imaging, all relevant radiation, including X-rays, is invisible to the naked eye, but that does not mean it is dark in the cosmological sense. Radiographers and physicists utilise highly sensitive instruments to measure radiation levels accurately. Devices such as dosimeters, ionisation chambers, and digital detectors are capable of quantifying exposure with high precision. There is no credible evidence that additional, unmeasured forms of radiation are present during medical imaging.
Addressing Radiation Myths and Public Concerns
Radiation is a subject that often generates anxiety, in part because it cannot be sensed directly. However, many of the fears associated with medical radiation are based on misconceptions.
A common myth is that X-rays leave behind some form of residual radiation in the body. This is untrue. X-rays pass through the body in a fraction of a second and do not linger. Unlike radioactive materials, which can continue to emit radiation over time, X-rays cease to exist once the machine is switched off.
Another myth is that certain forms of radiation cannot be detected but may still cause harm. While it is true that new forms of radiation are proposed in theoretical physics, these are not present in X-ray imaging equipment or procedures. Any radiation capable of ionising atoms, which is the type that can potentially damage DNA or cells, can be detected using standard equipment and accounted for in dose measurements.
Some people also believe that doctors are withholding information about hidden dangers associated with imaging. In reality, medical professionals are subject to strict regulatory oversight and are required to follow evidence-based guidelines for every imaging procedure. Radiation doses are always justified and minimised, especially for children, pregnant patients, and individuals undergoing repeated scans.
The Scientific Consensus on Radiation Exposure
Radiation protection guidelines are developed and enforced by international and national bodies such as the International Commission on Radiological Protection (ICRP), the Health and Safety Executive (HSE), and Public Health England (now part of the UK Health Security Agency). These organisations base their recommendations on decades of peer-reviewed research and epidemiological data.
In medical imaging, radiation exposure is kept as low as reasonably practicable – a principle known as ALARP. This means that procedures are only carried out when the potential clinical benefit outweighs the small risk associated with exposure. Modern equipment is also designed to use the minimum radiation dose necessary to achieve diagnostic image quality. Furthermore, digital imaging technologies have significantly reduced the required exposure compared to older film-based systems.
Staff working with X-rays wear personal dosimeters that record their cumulative exposure over time, ensuring that it remains within safe occupational limits. Patients’ exposure is carefully documented, and repeated scans are only recommended when clinically indicated.
Dark Radiation in Particle Physics and Its Irrelevance to Clinical Imaging
Returning to the original definition, dark radiation in the field of cosmology refers to hypothetical particles or energy that do not interact with light. These could include sterile neutrinos or other entities proposed in extensions to the Standard Model of particle physics. While fascinating from a theoretical standpoint, these forms of radiation are not known to interact with ordinary matter in a way that would affect human biology or medical diagnostics.
Sterile neutrinos, for example, are candidates for dark radiation because they may only interact via gravity and not through the electromagnetic or weak nuclear forces. If such particles do exist, they would pass through matter undetected and without causing harm. They do not produce ionisation, they do not alter imaging results, and X-ray machines do not generate them.
Therefore, from a clinical and practical perspective, dark radiation has no bearing on medical imaging. It is a theoretical construct without real-world impact on radiology.
Concluding Thoughts
The notion of dark radiation, while scientifically intriguing in the context of cosmology, has no relevance to X-ray imaging or medical diagnostics. All radiation used in healthcare is well understood, measurable, and subject to strict safety regulations. Misuse of the term “dark radiation” in clinical contexts can lead to confusion, unwarranted fear, and mistrust among medical professionals.
Patients undergoing X-ray procedures can be assured that every aspect of the imaging process is based on established scientific principles. All forms of radiation involved are monitored using precise instruments, and the risks are thoroughly assessed against the expected clinical benefits. There is no hidden or mysterious energy at play – only the application of well-tested physical principles that continue to save lives and improve health outcomes.
Ultimately, understanding radiation necessitates clear communication, honest engagement with scientific evidence, and a commitment to public education. By demystifying terms like “dark radiation,” we can focus on what truly matters: delivering safe, effective, and transparent healthcare.
Disclaimer
The information presented in this article is intended for general educational and informational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. The concepts discussed, including “dark radiation,” reflect current scientific understanding and are not intended to cause alarm or suggest unrecognised health risks in clinical imaging. All X-ray procedures and technologies mentioned are subject to rigorous regulation and oversight by qualified health and safety authorities. Readers should consult a qualified healthcare professional for advice relating to individual health concerns or diagnostic procedures. Open Medscience does not accept liability for any decisions made based on the content of this article.