Radiotheranostics is an innovative approach that combines both therapeutic and diagnostic techniques in cancer treatment. Due to their unique physical and biological properties, Alpha particles have emerged as a key tool in this field. Their high linear energy transfer (LET) and short penetration range make them particularly effective for targeting and destroying cancer cells while limiting damage to surrounding healthy tissue. This article explores the fundamental characteristics of alpha particles, their application in radiotheranostics, the development of alpha-emitting radionuclides, and the associated challenges, concluding with future directions in the field.
Introduction to Radiotheranostics
Radiotheranostics, a portmanteau of “radiotherapy” and “theranostics,” represents a breakthrough in cancer treatment that merges diagnostic imaging with targeted radionuclide therapy. This dual approach offers clinicians the ability to precisely locate, visualise, and treat tumours, allowing for personalised treatment plans that can significantly improve patient outcomes.
A vital aspect of radiotheranostics is the choice of radionuclides for both diagnosis and treatment. While beta particles and gamma emitters have been traditionally employed, alpha particles have gained increasing attention due to their superior cytotoxicity against cancer cells. Alpha-emitting radionuclides have unique properties that are particularly advantageous in killing malignant cells while sparing surrounding healthy tissue.
Properties of Alpha Particles
Alpha particles are essentially helium nuclei, consisting of two protons and two neutrons. They are emitted during the radioactive decay of certain heavy elements, such as radium, thorium, or uranium. Alpha particles are characterised by a high LET, which refers to the amount of energy they deposit per unit length of tissue. LET is a crucial factor in radiotherapy, as it determines how effectively radiation can damage the DNA of cancer cells.
High Linear Energy Transfer (LET)
The high LET of alpha particles means that they are extremely effective in causing double-strand breaks in DNA, leading to cell death. This property makes alpha particles highly potent when it comes to eradicating cancerous cells. A single alpha particle can deliver enough energy to break both strands of a DNA molecule, which is often irreparable by cellular mechanisms. This contrasts with beta particles, which have a lower LET and may require several hits to achieve a similar level of damage.
Short Range in Biological Tissues
Alpha particles have a very short range in biological tissues, typically between 50 and 100 micrometres. This limited range means that the damaging effects of alpha radiation are highly localised, targeting only cells in the immediate vicinity of the emission source. This is highly advantageous for therapeutic purposes, as it minimises damage to healthy tissues surrounding the tumour. The short range of alpha particles is particularly beneficial in treating micrometastases, where a small cluster of cancer cells can be targeted with minimal collateral damage.
Alpha Particles in Cancer Treatment
Alpha particles have shown great promise in treating various cancers, particularly those resistant to conventional therapies such as chemotherapy and beta-particle radiotherapy. The cytotoxicity of alpha particles is highly effective in killing slow-growing or dormant cancer cells that are often resistant to other forms of treatment.
Targeted Alpha Therapy (TAT)
One of the primary applications of alpha particles in radiotheranostics is Targeted Alpha Therapy (TAT). In TAT, alpha-emitting radionuclides are attached to molecules such as monoclonal antibodies or peptides that specifically target cancer cells. Once these molecules bind to the cancer cells, the alpha-emitting radionuclides decay, releasing alpha particles that destroy the cancer cells while sparing healthy tissue.
Examples of alpha-emitting radionuclides used in TAT include:
- Actinium-225: Actinium-225 is a potent alpha emitter with a half-life of around 10 days. It decays through a series of steps, producing several alpha-emitting daughter isotopes. This makes it particularly effective for TAT, as it delivers a prolonged dose of alpha radiation to the tumour site.
- Radium-223: Radium-223 is another alpha-emitting radionuclide that has been approved for the treatment of metastatic prostate cancer. It targets bone metastases due to its chemical similarity to calcium, which is naturally absorbed by bones. Radium-223 has a short half-life of 11.4 days, which limits radiation exposure to the patient.
- Astatine-211: Astatine-211 is a relatively rare alpha-emitting radionuclide, but it has shown promise in preclinical studies for the treatment of leukaemia and brain tumours. Its short half-life (7.2 hours) makes it suitable for targeting rapidly proliferating tumours.
Clinical Applications
TAT has been used in clinical trials to treat various forms of cancer, including leukaemia, prostate cancer, and neuroendocrine tumours. The results have been promising, with patients experiencing significant reductions in tumour size and, in some cases, complete remission. Furthermore, the highly localised nature of alpha particles helps to minimise the side effects typically associated with radiation therapy, such as damage to healthy organs and tissues.
In prostate cancer, for instance, Radium-223 has been successfully used to treat patients with metastatic bone disease, providing pain relief and extending survival. The use of Actinium-225 conjugated to prostate-specific membrane antigen (PSMA) ligands has also shown significant efficacy in reducing prostate-specific antigen (PSA) levels in advanced prostate cancer cases.
Challenges in Using Alpha Particles for Radiotheranostics
While alpha particles offer distinct advantages in radiotheranostics, there are several challenges associated with their use. These challenges are largely related to the production, delivery, and safety of alpha-emitting radionuclides.
Production of Alpha-Emitting Radionuclides
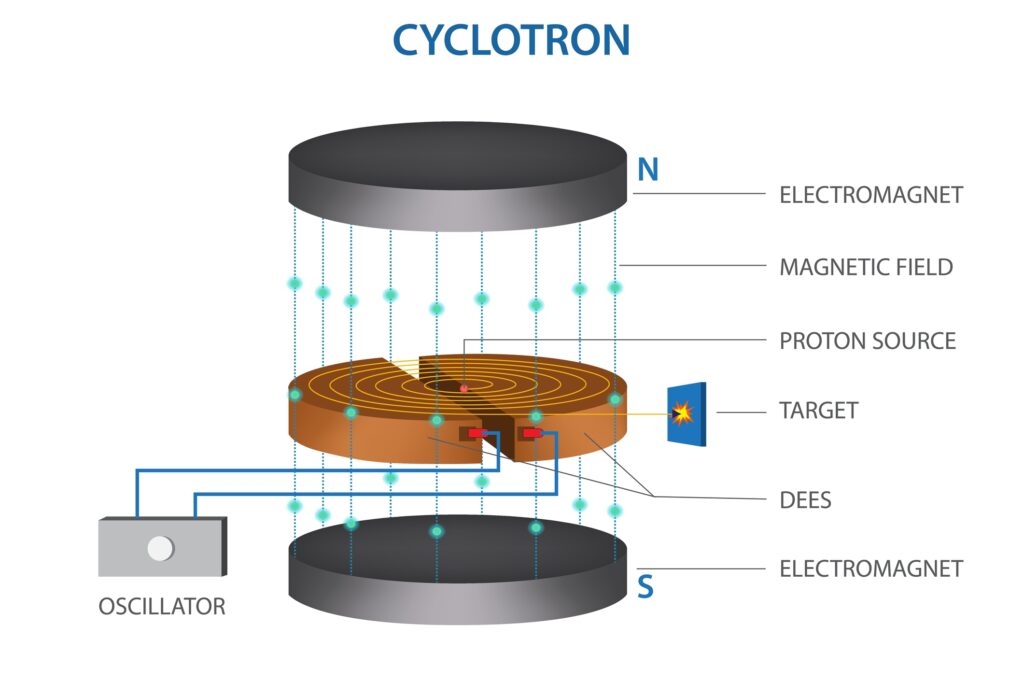
The availability of suitable alpha-emitting radionuclides is one of the primary challenges facing the widespread adoption of alpha particle-based radiotheranostics. Many alpha emitters are either rare or difficult to produce in sufficient quantities for clinical use. For instance, Actinium-225 is produced in small amounts through the decay of Thorium-229 or in particle accelerators, but these methods are currently limited in their ability to meet the growing demand for this radionuclide.
Furthermore, alpha emitters must be produced in highly controlled environments due to the hazards associated with handling radioactive materials. The production facilities must comply with stringent safety regulations, which adds to the cost and complexity of producing alpha-emitting radionuclides.
Delivery to Tumours
Another significant challenge is the effective delivery of alpha-emitting radionuclides to the tumour site. While TAT shows great promise, ensuring that the alpha-emitting radionuclides remain attached to their targeting molecules and do not degrade or lose efficacy before reaching the tumour is a complex task. If the radionuclide detaches from the targeting molecule, it could cause unintended damage to healthy tissues or organs.
To address this, researchers are developing more stable chelators and conjugates to improve the binding of alpha-emitting radionuclides to their targeting agents. This will help to enhance the precision of alpha particle delivery, increasing the therapeutic efficacy while minimising off-target effects.
Radiation Safety
Alpha particles are highly ionising, and while this is beneficial for targeting cancer cells, it also poses a risk to healthcare workers and patients if not handled properly. The short-range nature of alpha particles means that they are most dangerous when inhaled or ingested, as they can cause significant damage to internal tissues. Therefore, strict protocols must be followed during the production, handling, and administration of alpha-emitting radionuclides to minimise the risk of radiation exposure.
Healthcare workers involved in the preparation and administration of TAT must use specialised equipment and shielding to protect themselves from accidental exposure to alpha radiation. Patients must also be carefully monitored to ensure that the alpha-emitting radionuclides are properly eliminated from their bodies after treatment.
Future Directions in Alpha Particle Radiotheranostics
The future of alpha particles in radiotheranostics looks promising, with ongoing research and development aimed at addressing the challenges associated with their use. Several areas of innovation are expected to drive the continued advancement of alpha particle-based therapies.
Development of New Radionuclides
One of the most exciting areas of research is the development of new alpha-emitting radionuclides that are easier to produce and more effective in targeting cancer cells. For instance, researchers are investigating the use of alternative isotopes, such as Thorium-227, which can be produced in larger quantities than some of the more traditional alpha emitters.
The exploration of new production methods, including the use of particle accelerators and nuclear reactors, is also expected to improve the availability of alpha-emitting radionuclides. By increasing the supply of these isotopes, it will be possible to expand the use of alpha particles in clinical settings and make TAT more accessible to patients worldwide.
Combination Therapies
Another promising area of research is the combination of alpha particles with other forms of cancer treatment, such as immunotherapy and chemotherapy. By combining TAT with these therapies, it may be possible to enhance the overall effectiveness of cancer treatment and overcome resistance to individual therapies.
For example, combining alpha particle therapy with immune checkpoint inhibitors could potentially increase the immune system’s ability to recognise and attack cancer cells. Similarly, alpha particles could be used to sensitise tumours to chemotherapy, increasing the effectiveness of drug treatment while reducing the required dosage.
Nanoparticle-Based Delivery Systems
Nanotechnology is also being explored as a way to improve the delivery of alpha particles to tumours. Nanoparticle-based delivery systems can be designed to carry alpha-emitting radionuclides directly to the tumour site, improving the precision of treatment and reducing off-target effects.
These nanoparticles can be engineered to release their radioactive payload only when they reach the tumour, further enhancing the safety and efficacy of alpha particle therapy.
Alpha Particle Therapy in Precision Medicine
As the field of oncology continues to embrace personalised medicine, alpha particles are becoming increasingly relevant in precision treatment strategies. Precision medicine, which tailors treatment based on the genetic, environmental, and lifestyle factors of individual patients, is well-suited to the use of alpha particles in cancer therapy.
In precision radiotheranostics, alpha-emitting radionuclides can be selected and tailored to target specific biomarkers or receptors that are unique to a patient’s tumour. For instance, certain cancers express high levels of specific surface antigens, such as prostate-specific membrane antigen (PSMA) in prostate cancer or HER2 in breast cancer. By conjugating alpha emitters to targeting molecules that bind to these antigens, clinicians can deliver highly focused doses of radiation directly to the tumour cells.
This level of specificity ensures that alpha particle therapy fits well within the precision medicine framework, enabling more effective treatments with reduced side effects. This is especially important for patients with aggressive or recurrent cancers who may not respond well to conventional treatments.
Preclinical and Clinical Trials of Alpha Particle Radiotheranostics
Preclinical studies have shown the powerful cytotoxic effects of alpha particles in a variety of cancer models. These studies have demonstrated that alpha particles can effectively kill cancer cells at doses far lower than those required for beta or gamma radiation, reducing the risk of long-term side effects. Alpha-emitting radionuclides have been tested on several types of cancers in preclinical settings, including prostate cancer, breast cancer, and leukaemia.
Following the success of these preclinical trials, several alpha particle-based therapies have advanced to clinical trials. In clinical studies, alpha particle radiotheranostics has shown promising results in patients with metastatic cancer, particularly in cases where conventional therapies have failed.
For example, Actinium-225 labelled with PSMA ligands has shown great promise in treating advanced prostate cancer. Patients who have undergone this treatment have reported significant reductions in tumour burden and improved quality of life. Furthermore, these therapies have been well-tolerated, with relatively low toxicity compared to traditional forms of radiotherapy.
In another notable study, Astatine-211 was used to treat recurrent brain tumours. Astatine-211 is particularly effective for treating brain tumours due to its ability to cross the blood-brain barrier and target cancerous cells directly. Early clinical trials have shown that Astatine-211 can provide a significant survival benefit for patients with glioblastoma, one of the most aggressive types of brain cancer.
Dosimetry and Alpha Particle Therapy
An essential aspect of alpha particle radiotheranostics is accurate dosimetry—the measurement and calculation of the absorbed dose of radiation delivered to the tumour and surrounding tissues. Due to the high LET of alpha particles, it is crucial to precisely control the dose to maximise therapeutic benefits while minimising side effects.
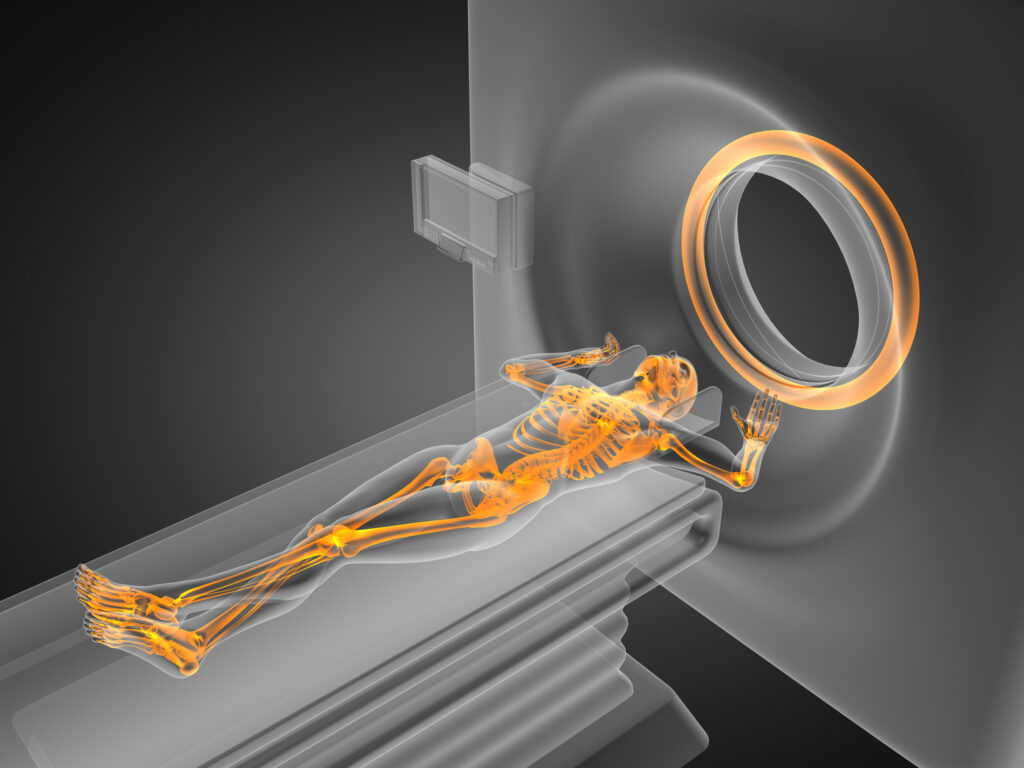
Dosimetry for alpha particle therapy presents unique challenges because the short range of alpha particles makes it difficult to measure their effects using traditional dosimetry techniques. However, advancements in imaging technologies, such as positron emission tomography (PET) and single-photon emission computed tomography (SPECT), are helping to improve the accuracy of dose calculations.
In modern dosimetry, computer simulations and mathematical models are also being employed to predict the behaviour of alpha particles in tissues, allowing for more precise planning of radiotherapy treatments. This ensures that the correct dose is delivered to the tumour, maximising the chances of successful treatment while avoiding excessive radiation exposure to healthy tissues.
Radiation-Induced Bystander Effect
One fascinating phenomenon observed with alpha particle therapy is the radiation-induced bystander effect. This occurs when cells that are not directly hit by alpha particles exhibit signs of damage due to signals received from nearby irradiated cells. The bystander effect suggests that the therapeutic effects of alpha particle therapy may extend beyond the cells that are directly targeted.
The exact mechanisms of the bystander effect are still being studied, but it is thought to involve the release of signalling molecules such as cytokines and reactive oxygen species (ROS) from irradiated cells, which can induce DNA damage in neighbouring cells. This could potentially enhance the efficacy of alpha particle therapy by amplifying the effects of the radiation on the tumour.
However, the bystander effect also poses a potential risk, as it could lead to damage in healthy tissues adjacent to the tumour. Understanding and controlling this effect is critical for the future development of alpha particle radiotheranostics.
Emerging Technologies in Alpha Particle Delivery
As research progresses, new technologies are being developed to enhance the precision and effectiveness of alpha particle delivery in radiotheranostics. These emerging technologies include advancements in targeting vectors, improved radionuclide production, and more sophisticated imaging and dosimetry techniques.
Targeting Vectors
Targeting vectors are molecules that carry alpha-emitting radionuclides to cancer cells. Innovations in molecular biology and chemistry are driving the development of more effective targeting vectors, such as monoclonal antibodies, peptides, and small molecules. These vectors are engineered to specifically bind to cancer-specific antigens, receptors, or other molecular markers on the surface of tumour cells.
For instance, bispecific antibodies, which can bind to two different targets simultaneously, are being explored as a means of improving the specificity and efficacy of alpha particle delivery. These antibodies can be designed to bind to both a cancer cell antigen and a radionuclide carrier, ensuring that the alpha-emitting radionuclide is delivered directly to the tumour site.
Theranostic Nanoparticles
Nanotechnology is also opening up new avenues for the delivery of alpha particles. Nanoparticles can be designed to carry multiple alpha-emitting radionuclides, increasing the dose delivered to the tumour while reducing the number of injections required. These nanoparticles can also be modified with targeting ligands to ensure that they selectively bind to cancer cells, minimising damage to healthy tissues.
Theranostic nanoparticles are a particularly exciting development, as they combine both therapeutic and diagnostic capabilities. By incorporating imaging agents into the nanoparticle structure, clinicians can use imaging techniques to track the distribution of the particles in the body in real-time. This allows for more precise monitoring of the treatment’s progress and enables adjustments to be made as needed.
Future Prospects and Conclusion
The use of alpha particles in radiotheranostics represents an exciting frontier in cancer treatment, offering the potential for highly targeted and effective therapies with minimal side effects. The unique properties of alpha particles, including their high LET and short range, make them particularly suited for the treatment of cancerous tissues while sparing healthy cells.
As research into alpha particle radiotheranostics continues to advance, several key areas of development hold great promise for the future. These include improving the production and availability of alpha-emitting radionuclides, enhancing targeting vectors, and further understanding the mechanisms of action, such as the bystander effect and combination with other therapies.
While challenges remain, particularly in the areas of radionuclide production, delivery, and radiation safety, the ongoing research in this field is likely to lead to significant breakthroughs in the coming years. Alpha particle therapy has already demonstrated significant potential in clinical trials, and as these technologies continue to mature, they are expected to play an increasingly important role in the future of personalised cancer treatment.
Ultimately, the integration of alpha particles into radiotheranostic strategies offers a promising path toward more effective, precise, and personalised cancer therapies. By harnessing the power of alpha radiation, clinicians may be able to offer new hope to patients with challenging and resistant forms of cancer, paving the way for better outcomes and improved quality of life.
Disclaimer
The content provided in this article is intended for informational and educational purposes only. Open Medscience does not offer medical, diagnostic, or therapeutic advice, and the information contained herein should not be interpreted as such. While efforts have been made to ensure the accuracy and relevance of the scientific content, the article does not substitute for professional medical guidance or consultation with qualified healthcare providers.
The discussion of alpha particles, radiotheranostic applications, and specific radionuclides reflects current knowledge and research as of the publication date. Clinical use of these therapies should be based on the most recent evidence, approved medical guidelines, and professional judgement.
Any mention of specific radionuclides, treatments, or clinical trials is not intended as an endorsement or recommendation. Readers are encouraged to consult with medical professionals or research specialists before acting on any of the information presented.
Open Medscience accepts no responsibility or liability for any loss or harm arising from the use of information contained in this article.
You are here: home » diagnostic medical imaging blog »