Chronic disease management is one of the most significant challenges facing modern healthcare systems. Conditions like diabetes, cardiovascular disease, and hypertension account for a substantial burden on both individual health and healthcare resources. Innovations in this field are essential to improve long-term patient outcomes, reduce hospital admissions, and increase the quality of life for millions of people worldwide. This article explores recent innovations in the management of chronic diseases, focusing on diabetes, cardiovascular disease, and hypertension. It highlights the integration of technology, personalised care approaches, patient education, and the importance of preventative measures in addressing these conditions. The article discusses how remote monitoring, artificial intelligence, and personalised medicine are reshaping care delivery, providing real-time insights and proactive interventions that improve long-term patient health outcomes.
Introduction
Chronic diseases such as diabetes, cardiovascular disease (CVD), and hypertension are among the leading causes of morbidity and mortality worldwide. In the UK, the National Health Service (NHS) is under considerable pressure, with these conditions accounting for a significant portion of healthcare spending. Managing these diseases involves a complex, long-term approach aimed at preventing complications and ensuring patients maintain a good quality of life.
Over the past decade, innovations in chronic disease management have gained momentum. These innovations are centred on technology, personalisation, and preventative care. The aim is to not only reduce the burden on healthcare providers but to empower patients to take control of their health, thus improving their long-term outcomes.
This article looks into the current trends and innovations in managing chronic conditions like diabetes, cardiovascular disease, and hypertension, examining how these approaches are transforming patient care.
Innovations in Diabetes Management
Continuous Glucose Monitoring (CGM) Systems
Continuous Glucose Monitoring (CGM) systems have revolutionised diabetes management, offering real-time monitoring of blood glucose levels. These systems use a sensor inserted under the skin to track glucose levels continuously, sending data to a mobile device or smartwatch. This innovation allows patients to monitor their blood sugar in real-time, rather than relying on periodic finger-prick tests.
CGM systems help patients identify trends in glucose fluctuations, particularly in response to food, exercise, or stress. By providing a more dynamic view of blood glucose, patients and healthcare providers can make more informed decisions about treatment. Furthermore, CGMs can alert patients when glucose levels are too high or low, enabling prompt action to avoid complications like hypoglycaemia.
In the long term, CGM systems can lead to better glycaemic control, fewer diabetes-related complications, and improved patient quality of life. For instance, Dexcom and Abbott’s Freestyle Libre are popular CGM devices that have improved diabetes self-management and provided patients with more autonomy over their care.
Artificial Pancreas Systems
The development of an artificial pancreas is another game-changing innovation in diabetes management. This system combines a CGM with an insulin pump, creating a closed-loop system that mimics the function of a healthy pancreas. By using algorithms to automatically adjust insulin delivery based on real-time glucose readings, the artificial pancreas reduces the burden of managing insulin doses manually.
Hybrid systems are already in use, and fully automated artificial pancreas systems are in development. This technology has the potential to vastly improve the management of Type 1 diabetes, offering patients more stable blood glucose control and reducing the risk of both hyperglycaemia and hypoglycaemia. As the technology becomes more widespread, it could revolutionise the standard of care for people with diabetes.
Personalised Medicine and Genetic Profiling
Personalised medicine is becoming an important factor in diabetes care. Advances in genetic profiling allow for the identification of individuals at higher risk for developing Type 2 diabetes. This early detection means that lifestyle modifications and targeted interventions can be implemented sooner, potentially delaying or even preventing the onset of the disease.
For those already living with diabetes, genetic profiling can offer insights into how different patients respond to medications, leading to more tailored treatment plans. In the near future, precision medicine could refine the management of diabetes, providing a more personalised approach to insulin therapy and other treatments.
Cardiovascular Disease: Technological and Preventative Innovations
Wearable Technology for Cardiac Monitoring
Wearable technology is at the forefront of innovation in managing cardiovascular disease. Devices such as smartwatches can monitor heart rate, detect irregular heartbeats, and provide alerts when abnormalities are detected. This real-time data enables earlier interventions for patients at risk of heart attacks or strokes.
For instance, the Apple Watch’s electrocardiogram (ECG) feature can detect atrial fibrillation (AFib), a leading cause of strokes. Early detection of AFib allows healthcare providers to initiate preventative treatments, such as blood thinners before a major cardiovascular event occurs. Wearables offer an affordable and accessible way for patients to track their heart health daily.
Remote Monitoring and Telemedicine
Remote monitoring technologies are also making a substantial impact on cardiovascular disease management. Patients with heart failure or other cardiovascular conditions can now use remote monitoring devices to track metrics like blood pressure, heart rate, and weight. These devices transmit data to healthcare providers, who can intervene when necessary.
Telemedicine platforms complement remote monitoring by providing patients with virtual consultations. This approach ensures that patients with cardiovascular conditions can receive timely advice and adjustments to their treatment plans without needing to visit the clinic frequently. Remote monitoring and telemedicine reduce hospital admissions and allow for earlier identification of potential complications, improving long-term outcomes for patients.
AI and Predictive Analytics in Cardiology
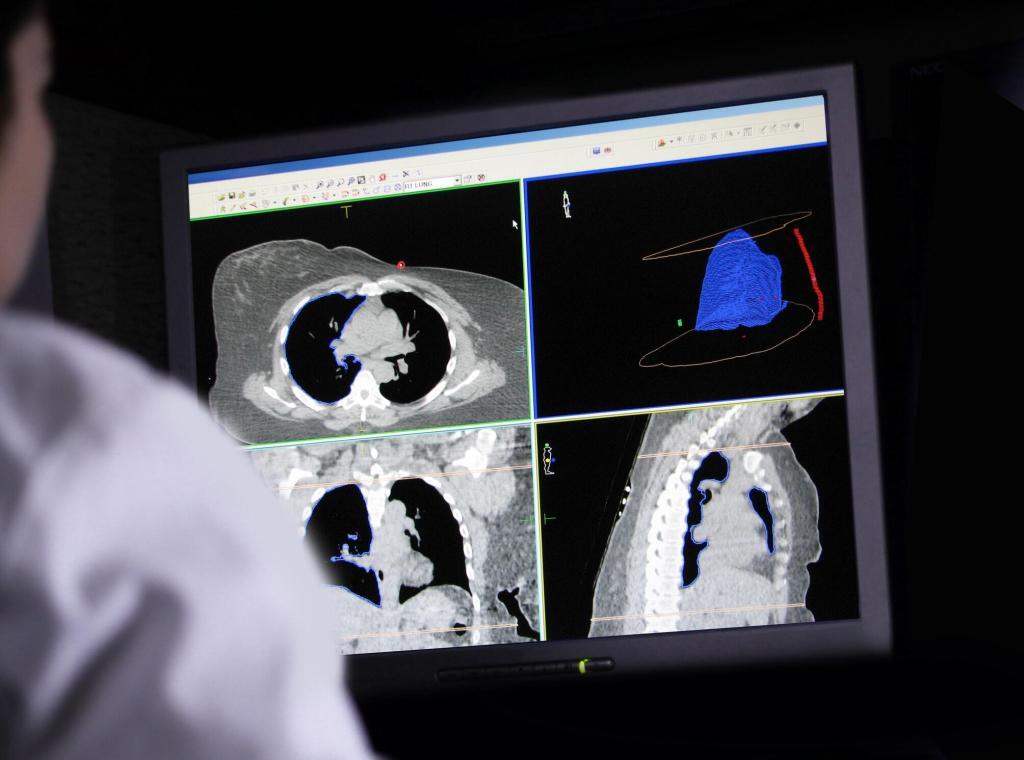
Artificial intelligence (AI) is transforming the field of cardiology. Machine learning algorithms can analyse large datasets to predict which patients are at the highest risk of developing cardiovascular diseases. Predictive analytics can identify risk factors, allowing healthcare providers to recommend lifestyle changes or preventative medications to at-risk patients.
Moreover, AI-driven tools are being used to enhance the accuracy of imaging techniques like echocardiograms and MRI scans, improving the diagnosis and treatment of heart disease. AI’s ability to quickly process vast amounts of data provides healthcare professionals with deeper insights, leading to more personalised treatment plans and better management of cardiovascular conditions.
Hypertension Management: The Role of Digital Health
Home Blood Pressure Monitoring
Home blood pressure monitoring (HBPM) has become a vital tool in the management of hypertension. Modern digital blood pressure monitors are easy to use and allow patients to track their blood pressure regularly. This real-time data can be shared with healthcare providers to adjust treatment plans as needed.
Home monitoring reduces the problem of “white coat hypertension,” where patients exhibit elevated blood pressure readings due to anxiety during medical appointments. It empowers patients to manage their condition actively and provides a more accurate representation of their blood pressure trends over time.
Smart Medication Adherence Tools
Medication adherence is critical in the management of hypertension. However, many patients struggle to take their medication consistently, leading to poorly controlled blood pressure and an increased risk of complications. Smart pill bottles and mobile apps have been developed to help patients adhere to their medication regimens. These tools can remind patients to take their medications and alert healthcare providers if doses are missed.
By improving medication adherence, these innovations can help patients maintain stable blood pressure, reducing the risk of strokes, heart attacks, and kidney disease. The use of such technology is particularly beneficial for elderly patients who may have trouble remembering their medications.
AI-Driven Risk Stratification
AI is playing an increasingly important role in hypertension management. Predictive models can analyse patient data to identify individuals at high risk of developing hypertension or related complications. Early identification allows healthcare providers to implement preventative strategies, such as lifestyle changes or medications, to reduce the patient’s risk of long-term damage.
AI-driven tools can also help stratify patients based on their risk of developing severe complications from hypertension. This information allows healthcare professionals to tailor treatment plans more effectively, ensuring high-risk patients receive more intensive monitoring and care.
The Role of Patient Education and Lifestyle Changes
While technological innovations are essential, patient education and lifestyle changes remain the cornerstone of chronic disease management. Educating patients about their condition, the importance of medication adherence, and the role of diet and exercise can significantly improve outcomes.
Diabetes
For diabetes, patient education is vital in ensuring that individuals understand how to manage their blood sugar levels effectively. Structured education programmes, such as the NHS’s Diabetes Education and Self-Management for Ongoing and Newly Diagnosed (DESMOND), teach patients how to manage their condition, recognise symptoms of complications, and adopt a healthier lifestyle.
Cardiovascular Disease
In cardiovascular disease management, lifestyle changes such as quitting smoking, reducing alcohol consumption, and increasing physical activity are critical. Cardiovascular rehabilitation programmes focus on helping patients make these changes and educating them about the risk factors associated with heart disease.
Hypertension
For hypertension, dietary changes, such as reducing salt intake and maintaining a healthy weight, are key strategies in controlling blood pressure. Many patients are unaware of how lifestyle factors impact their blood pressure. Providing patients with clear, actionable advice is an important aspect of hypertension management.
Future Directions in Chronic Disease Management
As healthcare continues to evolve, the integration of personalised medicine, artificial intelligence, and telehealth will become more prominent in managing chronic conditions. Furthermore, the use of wearable devices and real-time data collection will offer patients and healthcare providers unprecedented insights into disease progression and management.
One key area for future development is the increased use of machine learning algorithms to identify patterns in patient data that may not be immediately apparent to human clinicians. By identifying early warning signs of complications, these tools could enable preventative interventions that improve long-term outcomes and reduce the need for hospital admissions.
Additionally, the future of chronic disease management will likely see a shift towards more holistic care models. These models will focus not only on treating the disease itself but also on addressing the broader social, psychological, and economic factors that contribute to disease management.
Conclusion
Chronic disease management is undergoing a transformation driven by technological innovations, personalised care, and preventative strategies. The integration of tools such as CGM systems, wearable cardiac monitors, and AI-driven analytics is reshaping how patients with diabetes, cardiovascular disease, and hypertension are treated.
These innovations not only improve long-term patient outcomes but also empower individuals to take a more active role in their healthcare. As we move forward, it is essential to continue fostering advancements that prioritise patient-centred care and promote sustainable, long-term health outcomes for individuals living with chronic diseases.
Disclaimer
The information provided in Innovations in Chronic Disease Management: A New Frontier for Diabetes, Cardiovascular Disease, and Hypertension is intended for general informational purposes only. It does not constitute medical advice, diagnosis, or treatment and should not be relied upon as a substitute for professional healthcare guidance. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
Open Medscience does not endorse or recommend any specific tests, devices, procedures, or treatment methods mentioned in this article. References to particular technologies or products are for illustrative purposes and do not imply commercial endorsement. While efforts have been made to ensure the accuracy of the content, Open Medscience makes no representations or warranties about the completeness, accuracy, reliability, or suitability of the information contained herein.
Use of the information in this article is at your own risk. Open Medscience and its contributors disclaim any liability for any loss or damage arising from the use of this content.
You are here: home » diagnostic medical imaging blog »