Summary: Radionuclide therapy has become a promising approach for treating various forms of cancer and other medical conditions. While this targeted therapy offers benefits by selectively delivering radiation to diseased cells, it is not without adverse effects. These side effects vary widely depending on the radionuclide used, the dose administered, and the individual patient’s profile. This article explores the adverse effects of radionuclide therapy, covering the biological mechanisms behind these side effects, common toxicities, and long-term risks. Emphasis is placed on the need for effective management strategies and the direction of future research to improve patient safety and outcomes.
Introduction to Radionuclide Therapy
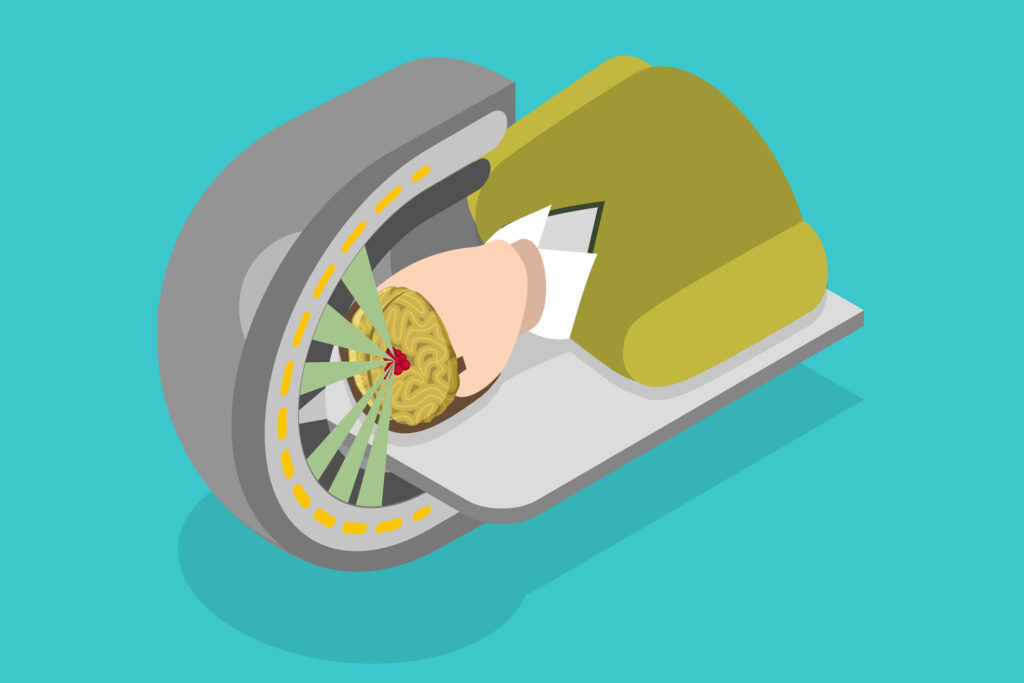
Radionuclide therapy is a form of targeted therapy used in oncology and nuclear medicine, where radioactive isotopes are administered to treat various conditions, particularly cancers such as thyroid cancer, neuroendocrine tumours, and prostate cancer. By delivering ionising radiation directly to affected cells, radionuclide therapy offers a way to minimise the damage to surrounding healthy tissue compared to traditional external radiation. However, this therapy does carry inherent risks, primarily due to radiation exposure, which can lead to both short- and long-term adverse effects.
Mechanisms of Action and Potential for Adverse Effects
Radionuclide therapy relies on the emission of alpha, beta, or gamma particles to destroy cancerous cells by causing DNA damage. However, this radiation can also affect normal cells, particularly those in close proximity to the targeted tissues. The extent of adverse effects depends on the type and energy of the radionuclide, its half-life, and its distribution in the body. Additionally, factors like patient age, health status, and pre-existing conditions influence susceptibility to these effects.
Common Adverse Effects of Radionuclide Therapy
- Gastrointestinal Toxicity
- Nausea and Vomiting: These are common after radionuclide therapy, particularly when administered orally or intravenously. This side effect is often transient but can affect patients’ quality of life.
- Diarrhoea: Radiotherapy-induced damage to the intestinal mucosa can lead to diarrhoea. This occurs more frequently with certain radionuclides that localise in the gastrointestinal tract.
- Loss of Appetite: Patients may experience reduced appetite, which can lead to nutritional deficiencies, further complicating their overall health and recovery.
- Haematological Toxicity
- Bone Marrow Suppression: Many radionuclides used in therapy accumulate in the bone marrow, which can lead to myelosuppression. Symptoms include anaemia, neutropenia, and thrombocytopenia, increasing the risk of infections and bleeding complications.
- Anaemia: Low red blood cell counts due to bone marrow suppression can cause fatigue and decreased oxygenation, impacting the patient’s overall energy levels and physical capacity.
- Neutropenia: Reduced white blood cell counts make patients more susceptible to infections, necessitating additional medical interventions and sometimes hospitalisation.
- Renal Toxicity
- Nephrotoxicity: Certain radionuclides are excreted primarily through the kidneys, exposing renal tissues to high radiation doses. Over time, this can cause kidney damage, leading to renal impairment or even chronic kidney disease.
- Electrolyte Imbalances: Kidney damage can disrupt the body’s ability to regulate electrolytes, causing imbalances that can lead to symptoms such as weakness, confusion, and cardiac irregularities.
- Hepatotoxicity
- Liver Function Impairment: The liver metabolises many radionuclides, and exposure to high doses of radiation can lead to hepatotoxicity. Symptoms include jaundice, elevated liver enzymes, and in severe cases, liver failure.
- Fatty Liver Changes: Radionuclide therapy may induce changes in hepatic fat metabolism, which can lead to fatty liver disease and affect overall liver function.
- Pulmonary Toxicity
- Pneumonitis: Radionuclide therapy for conditions near the lungs, such as certain thoracic cancers, can cause inflammation of the lung tissue, leading to pneumonitis. Symptoms include cough, shortness of breath, and chest pain.
- Fibrosis: Over time, radiation exposure to the lungs can lead to scarring or fibrosis, which decreases lung elasticity and affects respiratory function.
- Neurological Effects
- Neurotoxicity: Some radionuclides cross the blood-brain barrier, affecting brain tissue and potentially causing cognitive impairment, mood changes, and motor dysfunction.
- Peripheral Neuropathy: Radiation-induced nerve damage can lead to peripheral neuropathy, characterised by numbness, tingling, and pain, especially in the extremities.
- Endocrine Effects
- Thyroid Dysfunction: Radionuclide therapy, particularly with iodine-131 used in thyroid cancer treatment, can lead to hypothyroidism or hyperthyroidism due to damage to thyroid cells.
- Adrenal Insufficiency: In rare cases, radionuclide therapy can impact adrenal function, leading to insufficient production of hormones essential for stress response and metabolic regulation.
- Reproductive and Gonadal Toxicity
- Infertility: Radiation can impair reproductive organ function, leading to temporary or permanent infertility, particularly concerning for younger patients.
- Hormonal Imbalance: Radiation-induced damage to the ovaries or testes can disrupt hormone levels, potentially causing issues such as menstrual irregularities in women and low testosterone in men.
Long-term Risks and Late-Onset Effects
- Secondary Malignancies
- Patients exposed to radiation have an increased risk of developing secondary cancers, sometimes years after treatment. This risk is associated with DNA damage in healthy cells exposed to scattered or unintended radiation.
- Common Secondary Malignancies: Leukaemia, lung cancer, and solid tumours in other organs are among the most common secondary malignancies seen in patients who have undergone radionuclide therapy.
- Cardiotoxicity
- Certain radionuclides, especially when targeting cancers near the chest area, can lead to late-onset cardiotoxicity. This includes damage to the heart muscle, increased risk of arrhythmias, and, in severe cases, heart failure.
- Pericarditis: Radiation exposure can inflame the pericardium, causing chest pain and shortness of breath.
- Radiation-induced Fibrosis
- Long-term radiation exposure may lead to fibrosis in tissues exposed to the therapy. This can limit the flexibility and function of organs, impacting patients’ quality of life.
- Psychological Effects
- Cognitive Impairment: Patients may experience memory problems, confusion, or reduced executive functioning, often referred to as “radiation brain.”
- Anxiety and Depression: The experience of undergoing radionuclide therapy and coping with its side effects can increase the risk of anxiety and depression, impacting mental health and overall well-being.
Management of Adverse Effects
- Preventative Measures
- Personalised Dosing: Adjusting the dose according to patient-specific factors can help minimise adverse effects. Radiopharmaceutical dosimetry is a growing field aimed at tailoring doses to individual patients.
- Protective Agents: Drugs such as amifostine have shown promise in protecting healthy tissues from radiation damage.
- Symptom Management
- Anti-nausea and Anti-diarrhoeal Medication: These can improve gastrointestinal symptoms, enhancing patient comfort.
- Growth Factors and Blood Transfusions: For managing haematological side effects, haematopoietic growth factors or blood transfusions can be used to support red and white blood cell levels.
- Long-term Monitoring and Follow-up Care
- Regular Blood Tests: Monitoring blood counts, liver and kidney function, and thyroid levels can detect early signs of organ toxicity.
- Psychosocial Support: Counselling and support groups can help patients cope with the psychological burden of therapy.
- Advances in Radiopharmaceutical Design
- Developing radionuclides with shorter half-lives and more precise targeting capabilities can limit exposure to healthy tissues, reducing the potential for adverse effects.
Future Directions in Minimising Adverse Effects
- Enhanced Imaging Techniques
- Advances in imaging, such as PET/CT and SPECT, allow for more accurate localisation of radionuclides, enabling better treatment planning and minimising unintended radiation exposure.
- Combination Therapy
- Combining radionuclide therapy with other treatments, such as immunotherapy or targeted drugs, may enable lower doses of radiation, reducing side effects without compromising efficacy.
- Nanoparticle-based Delivery Systems
- Nanoparticles offer a promising platform for delivering radionuclides more precisely to tumour cells, thereby reducing off-target effects and improving the safety profile of radionuclide therapy.
- Individualised Treatment Protocols
- With advances in genetic profiling and biomarker analysis, individualised treatment protocols based on a patient’s unique biology can help predict and reduce adverse effects.
Conclusion
While radionuclide therapy represents a significant advancement in cancer treatment, it is accompanied by a range of adverse effects that can impact patients’ quality of life and long-term health. Understanding these risks, improving monitoring and management, and advancing research in targeted delivery mechanisms are essential to enhancing patient outcomes. Moving forward, innovations in personalised treatment, radiopharmaceuticals, and supportive care will continue to play a crucial role in minimising adverse effects and making radionuclide therapy safer and more effective for a broader range of patients.
Disclaimer
The content provided in this article is for informational and educational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Open Medscience does not provide medical services, and no material on this website is intended to replace consultation with a qualified healthcare provider.
Radionuclide therapy and its associated effects can vary significantly depending on numerous individual factors, including but not limited to medical history, treatment protocols, and specific radionuclide compounds. The potential adverse effects discussed in this article are general observations and may not apply to all patients. Always seek the advice of a medical professional regarding any questions you may have about a medical condition or treatment.
While efforts have been made to ensure the accuracy and reliability of the information at the time of publication, Open Medscience makes no guarantees regarding the completeness, timeliness, or current validity of the content. We do not accept any liability for injury, loss, or damage arising from the use of or reliance on the information contained within this article.
This article may refer to ongoing research and emerging technologies in nuclear medicine that are subject to further clinical evaluation. Readers should not interpret these references as endorsements of specific treatments or medical approaches.
Use of this article and any linked resources is entirely at your own risk.
You are here: home » diagnostic medical imaging blog »