Radiopharmaceuticals are transforming modern medicine, reshaping how disease is detected, monitored, and treated. Once confined to diagnostic imaging, these compounds now sit at the heart of a new therapeutic strategy known as theranostics, which unites diagnosis and treatment within a single molecular framework. The pace of innovation in this field has accelerated, driven by advances in isotope chemistry, molecular targeting, artificial intelligence, and regulatory support. Collectively, these developments mark the beginning of a new era in nuclear medicine, where personalised and targeted therapies are becoming a clinical reality.
The Rise of Theranostics
Theranostics combines diagnostic and therapeutic isotopes within a single targeting compound. This approach enables clinicians to visualise disease, predict therapeutic response, and deliver targeted treatment directly to diseased tissue. The approval of radiolabelled therapies for neuroendocrine tumours and prostate cancer established a new clinical model, demonstrating that targeted radionuclide therapy could achieve substantial tumour control with tolerable side effects.
Following these successes, researchers have expanded the approach to other cancers, including colorectal, thyroid, and breast malignancies. Beyond oncology, new applications are being explored in cardiovascular, neurological, and inflammatory conditions. The concept has evolved from matching one isotope to one tumour type to a more adaptable platform that allows multiple isotopes to be paired with a single molecular target. This flexibility allows for diagnostic imaging, therapy, and post-treatment monitoring to be integrated into a unified treatment pathway.
Expanding the Range of Isotopes
The effectiveness of a radiopharmaceutical depends heavily on the physical and chemical properties of its radionuclide. Historically, beta emitters such as yttrium-90 and lutetium-177 were the mainstay of therapeutic applications due to their well-understood decay characteristics and availability. However, new isotopes are emerging that offer greater precision, higher energy transfer, and shorter tissue penetration, all of which can improve clinical outcomes.
Alpha Emitters
Alpha-emitting radionuclides such as actinium-225, astatine-211, and thorium-227 are generating significant interest. Alpha particles deliver extremely high energy over very short distances, producing dense ionisation that can destroy cancer cells with remarkable efficiency while minimising damage to healthy tissue. These isotopes are particularly promising for treating small clusters of cancer cells and micrometastases that are resistant to conventional therapies.
Actinium-225 is being tested in various prostate and neuroendocrine tumour therapies, showing activity in patients who have stopped responding to lutetium-based treatments. Astatine-211 offers a favourable balance between energy output and half-life, making it well-suited to smaller peptides and antibodies. Production remains technically challenging, but investment in new accelerator technologies is beginning to address supply limitations.
Emerging Beta and Conversion-Electron Emitters
Other isotopes, such as terbium-161 and copper-67, are attracting attention for their dual therapeutic and imaging potential. Terbium-161 emits both beta particles and conversion electrons, enabling more efficient radiation delivery at the cellular level. Copper-67 can be paired with its diagnostic counterpart copper-64, creating a fully matched theranostic pair.
Improvements in cyclotron design and isotope separation methods are increasing access to these isotopes, allowing more institutions to participate in research and clinical trials. As availability improves, these new radionuclides are expected to complement or even replace traditional beta emitters in certain clinical settings.
Rethinking Targeting: From Agonists to Antagonists
Early radiopharmaceuticals were mainly based on receptor agonists — molecules that activate specific cellular receptors to deliver radioactive payloads. However, there has been a clear shift towards using receptor antagonists, which bind without triggering receptor activation. Studies show that antagonists often display higher tumour uptake, better lesion contrast, and improved stability.
In neuroendocrine tumours, somatostatin receptor antagonists have demonstrated superior imaging performance and potential therapeutic benefits compared with agonists. This change in strategy has encouraged the development of new targeting molecules across other receptor systems, including gastrin-releasing peptide receptors and fibroblast activation protein. The latter is especially promising because it targets the tumour stroma, providing a way to treat a broader range of solid tumours regardless of their cellular heterogeneity.
Personalised Dosimetry and Artificial Intelligence
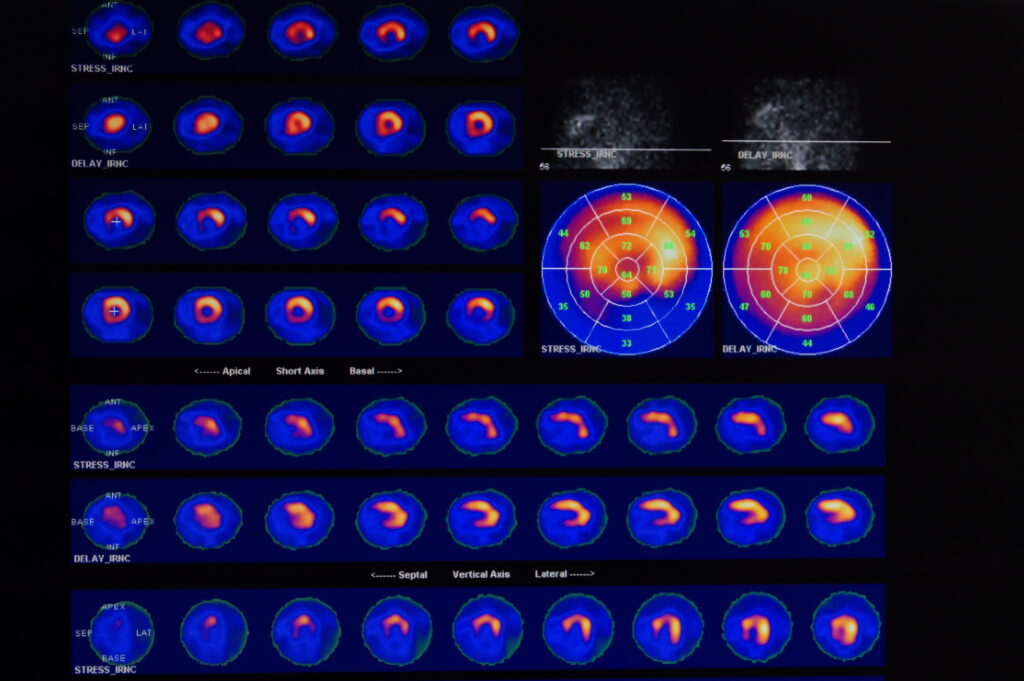
One of the defining trends in radiopharmaceutical therapy is the move towards personalised dosimetry — calculating the precise radiation dose delivered to tumours and normal organs for each individual. Historically, many treatments used fixed activity levels based on average population data. However, as understanding of radiobiology and patient variability has improved, the need for accurate, individualised dose assessment has become clear.
New computational tools are now enabling this personalisation. Population pharmacokinetic models use limited imaging data to predict organ uptake and clearance, offering reliable dose estimates without the need for multiple scans. Artificial intelligence is enhancing these models by learning from large datasets to simulate complex biodistribution patterns and to predict therapeutic outcomes.
Machine learning is also being applied to image reconstruction, noise reduction, and activity quantification in PET and SPECT imaging. By improving image quality and analysis speed, AI is helping to make dosimetry more accessible and consistent across treatment centres. These advances are laying the foundation for precision-guided radiopharmaceutical therapy, where each patient receives the optimal dose based on their unique physiology and disease profile.
Regulation, Manufacturing, and Supply
The growing clinical demand for radiopharmaceuticals has prompted regulators and manufacturers to strengthen the frameworks supporting their production and approval. Recent regulatory initiatives have focused on simplifying clinical development pathways and encouraging early integration of pharmacokinetic modelling and dose optimisation in trial design.
At the same time, governments and industry are addressing long-standing issues with isotope supply. Many therapeutic isotopes are produced in nuclear reactors or particle accelerators under tight time constraints, and disruptions in supply can delay treatment or halt research programmes. New facilities are being commissioned to produce isotopes such as actinium-225, copper-67, and terbium-161, reducing dependence on a small number of international sources.
Private investment is also expanding, with several pharmaceutical companies forming partnerships to scale up radiopharmaceutical manufacturing. These collaborations aim to build robust, distributed supply chains capable of supporting both clinical trials and commercial distribution.
Current Clinical Developments
Radiopharmaceutical therapy is moving rapidly from research into mainstream clinical practice. Numerous Phase 3 trials are underway across a wide spectrum of cancers, including prostate, neuroendocrine, thyroid, and colorectal tumours. The most advanced programmes focus on optimising isotope selection, dosing strategies, and combination therapies to improve patient outcomes.
In prostate cancer, newer PSMA-targeted compounds labelled with alpha emitters are being developed to overcome resistance to existing lutetium-based treatments. In neuroendocrine tumours, somatostatin receptor antagonists are achieving improved imaging accuracy and potentially greater therapeutic benefit.
Beyond oncology, the applications of radiopharmaceuticals are expanding. In neurology, radiotracers designed to bind amyloid and tau proteins are being adapted for both imaging and targeted therapy in neurodegenerative diseases. In cardiology, isotopes targeting fibroblast activation protein and integrins are showing promise for assessing myocardial fibrosis and post-infarction healing. Early research in inflammation and infection imaging is also opening the door to therapeutic approaches for autoimmune diseases and chronic inflammatory conditions.
Challenges to Overcome
Despite the remarkable progress, the field faces several persistent challenges.
Isotope supply remains one of the most significant. Many promising isotopes are produced only in small quantities and require highly specialised facilities. Their short half-lives further complicate transport and storage, making reliable supply a critical issue for clinical translation.
Dosimetry standardisation is another concern. Although AI and modelling tools are improving accuracy, there is no universal consensus on best practice for dose estimation and reporting. Differences in imaging protocols, reconstruction methods, and instrumentation can affect results, making comparisons between institutions difficult.
Cost and infrastructure also limit wider adoption. Setting up a radiopharmacy or theranostic centre requires substantial capital investment, specialist staff, and regulatory oversight. Smaller hospitals may find these requirements prohibitive without regional collaboration or centralised production models.
Finally, patient selection continues to evolve. Biomarkers that predict therapeutic response are essential for identifying patients who will benefit most from treatment while avoiding unnecessary exposure. Molecular imaging and genomic profiling are increasingly used to guide these decisions, but further validation is required before they can be routinely implemented.
Expanding Beyond Cancer
While most radiopharmaceutical research has focused on oncology, new directions are emerging in non-malignant diseases. In cardiology, radiotracers that track tissue repair and fibrosis could provide early indicators of heart failure or post-infarction recovery. In neurology, therapeutic isotopes capable of crossing the blood–brain barrier may open new treatment avenues for conditions such as glioblastoma, Parkinson’s disease, and Alzheimer’s disease.
Inflammatory disorders also present a promising frontier. Targeting activated macrophages and immune cell receptors could enable precise modulation of immune responses, offering new strategies for treating diseases like rheumatoid arthritis and multiple sclerosis. These non-oncological applications may eventually broaden the impact of radiopharmaceuticals beyond cancer care, bringing molecular precision to a wider range of chronic conditions.
The Future of Radiopharmaceuticals
Radiopharmaceuticals are at the forefront of personalised medicine, uniting diagnostic imaging with targeted therapy in a single process. The rapid progress in isotope development, receptor targeting, dosimetry, and artificial intelligence is creating new standards for how disease is managed.
The next decade will likely see radiopharmaceuticals integrated into routine clinical practice across multiple disease areas. Success will depend on building sustainable isotope supply chains, harmonising dosimetry protocols, and expanding access to specialised facilities. Collaboration between academia, industry, and healthcare systems will be essential to realise the full potential of this technology.
Radiopharmaceuticals represent far more than a new class of drugs — they embody a shift in how medicine is practised. By allowing clinicians to both see and treat disease at the molecular level, they are transforming the principles of diagnosis and therapy into a single, precise, and patient-centred process.
Disclaimer
The information presented in The Latest Developments in Radiopharmaceuticals: Advancing Precision Imaging and Therapy is provided for educational and informational purposes only. It does not constitute medical, scientific, or professional advice and should not be relied upon for clinical decision-making, diagnosis, or treatment. Readers are encouraged to consult qualified healthcare professionals or subject matter experts before applying any information discussed in this article.
Open MedScience makes every effort to ensure that the content is accurate and up to date at the time of publication; however, no guarantees are made regarding the completeness, reliability, or ongoing accuracy of the information provided. References to specific products, technologies, or organisations do not imply endorsement or recommendation.
Neither Open MedScience nor its authors accept responsibility for any loss, injury, or damages arising from the use or interpretation of this material. All opinions expressed are those of the author(s) and do not necessarily reflect the views of Open MedScience, its affiliates, or contributors.
You are here: home » diagnostic medical imaging blog »