Medical imaging plays an essential role in diagnosing, managing, and understanding ear disorders. The ear is a complex sensory organ responsible not only for hearing but also for balance, and its small size and intricate structure present unique diagnostic challenges. Over the past few decades, advances in imaging technology have transformed how clinicians evaluate ear diseases, guiding both medical and surgical interventions with remarkable precision.
This blog article explores the anatomy of the ear, the main imaging modalities used to examine it, the conditions these techniques help diagnose, and recent innovations that are shaping the future of otological imaging.
Understanding the Anatomy of the Ear
The ear is divided into three main regions: the external ear, the middle ear, and the inner ear. Each has distinct structures and functions, and understanding their anatomy is key to interpreting medical images effectively.
The external ear comprises the pinna (auricle) and the external auditory canal. Its primary role is to capture and funnel sound waves towards the tympanic membrane (eardrum).
The middle ear is an air-filled cavity that contains three small bones called the ossicles – the malleus, incus, and stapes – which transmit vibrations from the eardrum to the inner ear. The middle ear also includes the Eustachian tube, which regulates air pressure, and several important nerves and blood vessels.
The inner ear houses the cochlea, responsible for hearing, and the vestibular apparatus, which governs balance. These structures are enclosed within the dense petrous portion of the temporal bone and contain delicate membranous labyrinths filled with fluid.
Because of this structural complexity, imaging the ear requires techniques capable of capturing fine details at high resolution. The most commonly used imaging modalities are computed tomography (CT) and magnetic resonance imaging (MRI), each offering distinct advantages.
Computed Tomography (CT) in Ear Imaging
CT scanning is one of the most widely used imaging methods for evaluating ear disorders, particularly those involving bone structures. By using X-rays to create detailed cross-sectional images, CT provides excellent visualisation of the temporal bone and its intricate anatomy.
High-Resolution CT (HRCT) is the gold standard for temporal bone imaging. With slice thicknesses as thin as 0.5 mm, HRCT can reveal subtle changes in bony structures that are invisible on conventional radiographs. This level of detail is essential for assessing the ossicles, semicircular canals, cochlea, and facial nerve canal.
CT is especially valuable for diagnosing:
- Chronic otitis media and cholesteatoma: CT helps detect bone erosion, ossicular damage, and the extent of soft tissue involvement.
- Congenital malformations: It can identify anomalies in the external auditory canal, ossicular chain, or cochlear formation.
- Otosclerosis: CT visualises abnormal bone remodelling around the stapes footplate and oval window.
- Temporal bone fractures: Following head trauma, CT can quickly reveal fractures, fluid collections, and potential damage to the facial nerve or inner ear.
Because of its speed and availability, CT is also the first-line imaging choice in emergency settings. However, it exposes patients to ionising radiation and provides limited soft tissue contrast, which is why MRI is often used as a complementary technique.
Magnetic Resonance Imaging (MRI) of the Ear
MRI uses powerful magnets and radiofrequency waves to generate detailed images without ionising radiation. Its strength lies in visualising soft tissue structures, fluids, and nerve pathways – aspects that CT cannot show as clearly.
In ear imaging, MRI is particularly useful for assessing the inner ear and internal auditory canal. It can detect abnormalities of the cochlea, vestibular system, and cranial nerves VII (facial) and VIII (vestibulocochlear), as well as soft tissue masses that might indicate tumours or inflammatory processes.
MRI is essential for diagnosing:
- Vestibular schwannoma (acoustic neuroma): These benign tumours of the vestibulocochlear nerve are often first detected on MRI. High-resolution sequences like T2-weighted constructive interference in steady state (CISS) or fast imaging employing steady-state acquisition (FIESTA) provide excellent detail of the internal auditory canal.
- Labyrinthitis and inner ear inflammation: MRI can detect enhancement patterns within the membranous labyrinth and cochlea, indicating infection or inflammation.
- Endolymphatic hydrops: Specialised MRI techniques allow visualisation of fluid compartments in the inner ear, aiding the diagnosis of Ménière’s disease.
- Soft tissue masses and tumours: Lesions such as glomus tumours, meningiomas, or metastases are better characterised on MRI than CT.
Contrast-enhanced MRI further improves diagnostic accuracy, particularly when evaluating tumours, inflammatory lesions, or vascular malformations. The absence of radiation makes MRI particularly suitable for paediatric patients and repeated follow-up imaging.
Ultrasonography in Ear Imaging
While not a first-line modality for internal ear structures, ultrasound has a limited role in specific clinical situations. It is most useful for examining superficial structures of the external ear, such as cysts, abscesses, or soft tissue masses.
Ultrasound can also aid in image-guided procedures like needle aspirations or drainage. However, because ultrasound waves do not penetrate bone well, its use in imaging the middle or inner ear is highly restricted.
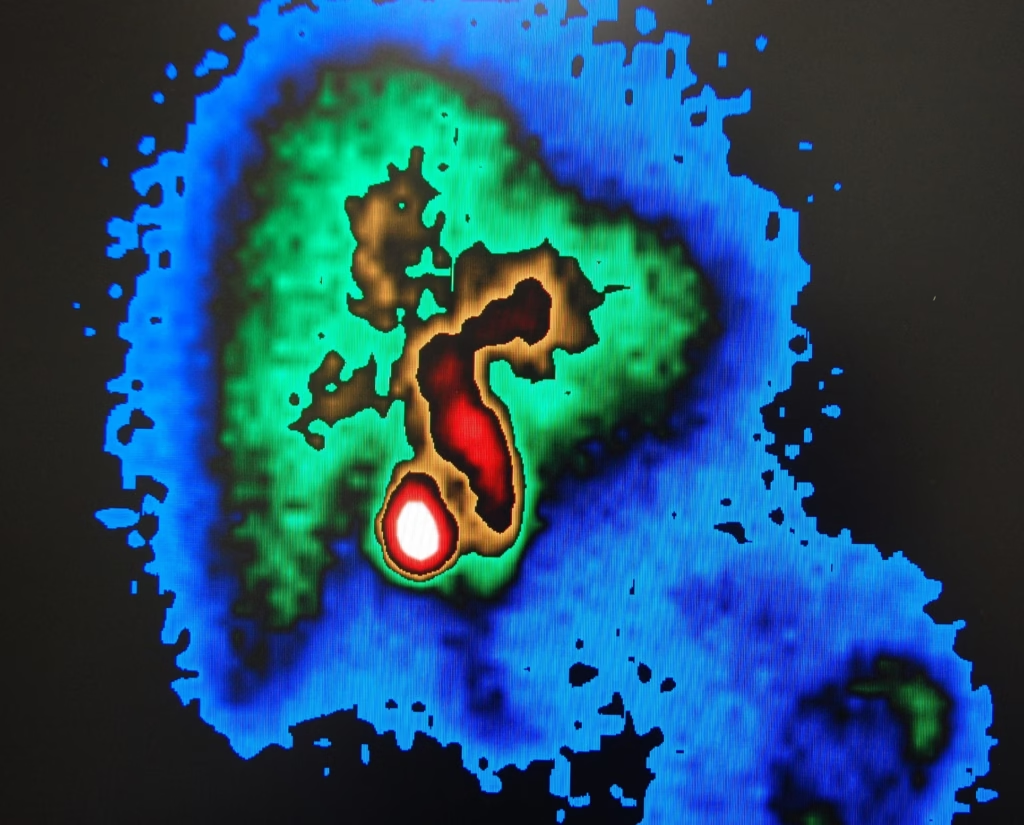
Positron Emission Tomography (PET) and Functional Imaging
Although not commonly used for routine ear imaging, PET-CT and PET-MRI have emerging roles in oncology and research. PET can detect metabolic activity and is useful for identifying malignant tumours, staging disease, and monitoring treatment response.
For instance, PET imaging can differentiate recurrent cholesteatoma from postoperative granulation tissue or help evaluate the spread of temporal bone malignancies. Research is also exploring functional imaging of the auditory pathways and brain regions involved in hearing, potentially advancing the understanding of sensorineural hearing loss.
Imaging of Specific Ear Disorders
Medical imaging is integral to diagnosing a broad range of ear conditions. Below are some of the most significant disorders and how imaging contributes to their evaluation and management.
Chronic Otitis Media and Cholesteatoma
Chronic otitis media can cause persistent inflammation, perforation of the tympanic membrane, and erosion of ossicles. CT is the preferred imaging modality to assess the extent of disease, ossicular damage, mastoid involvement, and potential intracranial complications.
Cholesteatoma, a destructive keratinising lesion, often arises as a complication of chronic otitis media. CT helps detect bony erosion and guide surgical planning, while diffusion-weighted MRI is useful for identifying residual or recurrent disease after surgery.
Otosclerosis
Otosclerosis is characterised by abnormal bone remodelling in the otic capsule, leading to conductive or mixed hearing loss. CT can reveal demineralised foci around the oval window and stapes footplate, as well as cochlear involvement in advanced cases. Accurate imaging is crucial for surgical planning, particularly when considering stapedectomy.
Vestibular Schwannoma
Vestibular schwannoma is a benign tumour that arises from the vestibular portion of the vestibulocochlear nerve. It typically presents with unilateral hearing loss, tinnitus, or balance disturbances. MRI is the imaging modality of choice, as it provides detailed information about tumour size, location, and involvement of adjacent structures. Serial MRI scans are often used to monitor growth in patients managed conservatively.
Temporal Bone Trauma
Temporal bone fractures often result from head injuries and can cause hearing loss, facial nerve paralysis, or cerebrospinal fluid leakage. CT is indispensable in detecting fractures, ossicular chain disruption, and inner ear involvement. MRI may be added if there is suspicion of soft tissue injury, nerve damage, or labyrinthine haemorrhage.
Congenital Malformations
Imaging is vital in diagnosing congenital ear anomalies, which can range from atresia of the external auditory canal to cochlear hypoplasia or semicircular canal dysplasia. CT provides detailed views of bony malformations, while MRI offers complementary information on membranous structures and nerve integrity. These findings are essential for surgical planning, including cochlear implantation.
Ménière’s Disease and Endolymphatic Hydrops
Recent MRI techniques can visualise the endolymphatic and perilymphatic spaces within the inner ear after intratympanic or intravenous gadolinium administration. This has enabled non-invasive diagnosis of endolymphatic hydrops, a key feature of Ménière’s disease, allowing earlier intervention and more tailored treatment strategies.
Advances in Ear Imaging Technology
Technological progress continues to enhance the quality, speed, and diagnostic capabilities of ear imaging. One of the most significant developments is the introduction of multi-detector CT (MDCT), which offers faster acquisition times and improved spatial resolution. Iterative reconstruction algorithms further reduce radiation dose while maintaining image quality.
MRI has also advanced significantly, with high-field (3T and above) scanners and improved coil technology delivering higher resolution and faster imaging times. New sequences, such as diffusion-weighted imaging (DWI) and three-dimensional steady-state sequences, have improved the detection of subtle lesions like small cholesteatomas and microstructural changes in the inner ear.
Fusion imaging combining CT and MRI data is becoming increasingly valuable in preoperative planning, particularly for complex otological surgeries such as cochlear implantation. By integrating bony and soft tissue detail into a single dataset, surgeons can plan trajectories with greater accuracy and avoid critical structures.
Artificial intelligence (AI) and machine learning are also beginning to influence ear imaging. AI algorithms are being developed to automate the segmentation of ear structures, detect subtle pathological changes, and even predict outcomes based on imaging data. These tools could enhance diagnostic precision and reduce interpretation times in the future.
Imaging in Surgical Planning and Postoperative Follow-Up
Imaging plays a crucial role not only in diagnosis but also in guiding surgical intervention and monitoring outcomes. Preoperative CT scans are essential for planning procedures like mastoidectomy, ossiculoplasty, and cochlear implantation, as they help identify anatomical variations and potential surgical risks.
Postoperative imaging assesses implant positioning, detects complications, and monitors disease recurrence. For example, diffusion-weighted MRI can detect recurrent cholesteatoma without the need for exploratory surgery, and CT can confirm the correct placement of cochlear implant electrodes.
Paediatric Ear Imaging Considerations
Imaging in children presents unique challenges, including the need to minimise radiation exposure and reduce motion artefacts. MRI is often preferred for paediatric patients due to the absence of ionising radiation, particularly when evaluating congenital anomalies or inner ear malformations. Sedation or anaesthesia may be necessary for younger patients to obtain high-quality images.
CT remains valuable for detailed evaluation of the temporal bone, especially when planning surgical interventions. Low-dose protocols and rapid acquisition techniques help mitigate radiation risks in paediatric imaging.
Future Directions in Ear Imaging
The future of ear imaging is likely to be shaped by further technological refinement and integration with emerging fields such as genomics and regenerative medicine. Ultra-high-resolution CT and MRI scanners are expected to reveal even finer anatomical details, improving early diagnosis and surgical precision.
Functional MRI and advanced diffusion imaging could provide new insights into the physiology of hearing and balance, potentially leading to novel treatments for sensorineural hearing loss and vestibular disorders. AI-powered diagnostic tools may become standard in clinical workflows, enhancing diagnostic accuracy and enabling personalised treatment planning.
Another promising direction is image-guided surgery, where real-time imaging and navigation systems assist surgeons in performing minimally invasive procedures with greater precision. As these technologies evolve, they will likely reduce complications and improve outcomes for patients undergoing ear surgery.
Conclusion
Medical imaging has revolutionised the diagnosis and management of ear disorders, offering detailed insights into the complex anatomy and pathology of this vital sensory organ. CT and MRI remain the cornerstones of ear imaging, each with distinct strengths that complement one another. Advances in imaging technology, from high-resolution scanners to AI-powered analysis, continue to enhance diagnostic capabilities and guide treatment with increasing precision.
As innovation accelerates, ear imaging will play an even greater role in understanding hearing and balance disorders, improving patient outcomes, and shaping the future of otological care. From diagnosing chronic infections and tumours to planning delicate surgical procedures, imaging remains an indispensable tool in modern otology and neurotology.
Disclaimer
The content provided in Medical Imaging of the Ear: Techniques, Applications, and Advances is intended for informational and educational purposes only. It does not constitute medical advice, diagnosis, or treatment and should not be relied upon as a substitute for professional healthcare consultation. Clinicians, researchers, and readers are advised to consult qualified medical professionals and refer to relevant clinical guidelines before making decisions based on the information contained herein. Open MedScience and the authors accept no responsibility or liability for any loss, damage, or injury arising from the use of this material.