In the evolving landscape of therapeutic nuclear medicine, five radionuclides stand at the forefront of innovation and treatment efficacy: Lutetium-177, Astatine-211, Yttrium-90, Rhenium-186, and Rhenium-188. These radionuclides are pivotal in diagnosing and treating a myriad of diseases, offering hope and enhanced quality of life to patients worldwide. This article explores each radionuclide’s characteristics, applications, and future prospects, exploring their integral roles in the medical field.
The Role of Radionuclides in Therapeutic Nuclear Medicine
Therapeutic nuclear medicine represents a significant leap forward in medical diagnostics and treatment, particularly in the fight against cancer. This innovative field utilises radionuclides—atoms characterised by their instability and the emission of radiation—to identify and combat various diseases. Radionuclides have the dual capability to diagnose and treat, marking them as powerful tools in contemporary medicine. Among the plethora of radionuclides available for medical use, five have risen to prominence due to their specific attributes and efficacy in treatment: Lutetium-177 (Lu-177), Astatine-211 (At-211), Yttrium-90 (Y-90), Rhenium-186 (Re-186), and Rhenium-188 (Re-188). Each of these radionuclides offers unique properties, making them indispensable in the arsenal of therapeutic nuclear medicine.
The journey of therapeutic nuclear medicine began with the realisation that the energy emitted by radionuclides could be harnessed for medical purposes. When introduced into the body, these radioactive elements seek out and localise in specific tissues, including cancerous cells. This targeting ability stems from the radionuclides’ attachment to certain molecules or compounds that have an affinity for the diseased cells. Once localised, they emit radiation that can diagnose or obliterate the targeted cells, offering a highly selective approach to treatment.
Lutetium-177 has emerged as a cornerstone in the treatment of various cancers, including neuroendocrine tumours and prostate cancer. Its popularity stems from its ability to emit beta radiation, which possesses the right balance of energy and penetration depth to effectively treat small to medium-sized tumours while minimising damage to surrounding healthy tissue.
Astatine-211, although less widely used than Lutetium-177, holds great promise due to its emission of alpha particles. These particles have a high energy release within a short range, making At-211 particularly effective in eradicating small clusters of cancer cells with minimal collateral damage. This precision targets the cancer cells more effectively and reduces the risk of damage to the surrounding healthy tissues.
Yttrium-90 can be used in radioembolisation, a procedure that treats liver cancer by injecting microspheres coated with Y-90 directly into the liver’s blood supply. This method allows for a high dose of targeted radiation, offering a potent treatment option for patients with inoperable tumours.
Rhenium-186 and Rhenium-188, isotopes of the same element, have found their niche in the treatment of pain associated with bone metastases, a common complication in cancer patients. These radionuclides are incorporated into pharmaceuticals that home in on bone tissue, delivering radiation that alleviates pain by reducing the size of bone tumours and lesions.
The significance of these five radionuclides in therapeutic nuclear medicine cannot be overstated. Their ability to provide targeted treatment options marks a turning point in the management of cancer and other diseases. By harnessing the power of these radioactive elements, medical professionals can offer treatments that are not only effective but also minimally invasive, paving the way for a new era in medical care. As research continues and technology advances, the role of these radionuclides is set to expand, further solidifying their status as essential components of therapeutic nuclear medicine.
Lutetium-177: Pioneering Precision in Therapeutic Nuclear Medicine
Lutetium-177 (Lu-177) stands out as a beacon of hope for patients battling various cancers in therapeutic nuclear medicine. This beta-emitting radionuclide boasts properties that make it exceptionally suited for precise therapeutic applications. With a half-life of approximately 6.65 days, Lu-177 strikes the perfect balance between efficacy and safety, providing ample time for the radionuclide to target and destroy tumour cells while its radioactivity naturally decays, thereby reducing exposure to healthy tissues.
One of the key advantages of Lu-177 is its relatively short-range radiation emission, typically spanning only a few millimetres. This characteristic ensures that the radiation’s destructive power is concentrated on tumour cells with minimal collateral damage to surrounding healthy tissues. This precision targeting makes Lu-177 an invaluable asset in the fight against cancer, particularly when dealing with small tumours and metastases that require targeted intervention without compromising the integrity of the surrounding healthy tissue.
Applications in Medicine
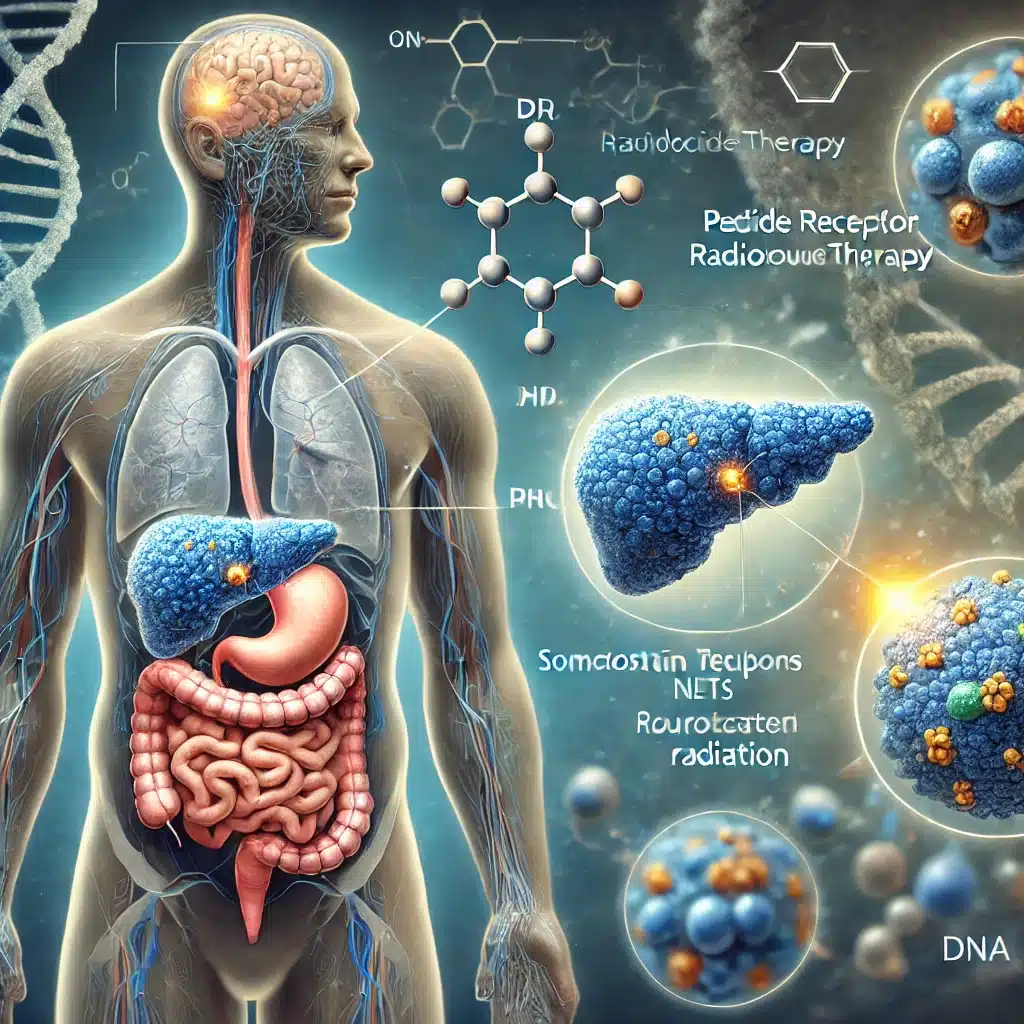
Lu-177 has a versatile and safe profile which leads to its widespread adoption in Peptide Receptor Radionuclide Therapy (PRRT), especially in the management of neuroendocrine tumours. Neuroendocrine tumours, which can occur in various parts of the body, including the pancreas and the gastrointestinal tract, often present a significant treatment challenge due to their unique characteristics and behaviour. PRRT with Lu-177 leverages the radionuclide’s ability to deliver targeted radiation to tumour cells expressing specific receptors, offering a highly effective treatment modality that can significantly improve patient outcomes.
Beyond its established role in neuroendocrine tumour therapy, Lu-177 is making strides in the treatment of prostate cancer, a prevalent and sometimes aggressive malignancy affecting millions of men worldwide. The advent of Prostate-Specific Membrane Antigen (PSMA) targeting therapies utilising Lu-177 has opened up new horizons in prostate cancer treatment. PSMA is a protein abundantly expressed on the surface of prostate cancer cells which makes it an ideal target for radionuclide therapy. By attaching Lu-177 to molecules that specifically bind to PSMA, clinicians can deliver radiation directly to prostate cancer cells, regardless of their location in the body. This targeted approach not only enhances the effectiveness of the treatment but also minimises the side effects associated with traditional systemic therapies.
The promising results of Lu-177-based therapies in prostate cancer treatment underscore the radionuclide’s potential to revolutionise cancer therapy. As research continues and new applications are explored, Lu-177 is poised to expand its role in therapeutic nuclear medicine, offering hope to patients with advanced or hard-to-treat cancers. With its unique combination of properties and growing list of applications, Lutetium-177 embodies the future of precision oncology, marking a significant milestone in the journey towards more effective and less invasive cancer treatments.
Astatine-211: A Cornerstone in Precision Oncology
Astatine-211 (At-211) stands out as a radionuclide with profound implications in the area of therapeutic nuclear medicine, particularly due to its role as an alpha emitter. Unlike its beta-emitting counterparts, At-211 is characterised by the emission of high-energy alpha particles, which have a very short range and are capable of delivering a highly concentrated dose of radiation. This feature of At-211 makes it uniquely suited for applications where precision and targeted therapeutic effects are crucial. The short range of alpha particles—typically a few cell diameters—ensures that the radiation damage is confined to the immediate vicinity of the targeted cells, minimising the risk to surrounding healthy tissue.
The physical and chemical properties of At-211 contribute to its suitability for medical applications. With a half-life of approximately 7.2 hours, At-211 provides a practical window for therapeutic use, allowing for the administration of treatment and the decay of radioactivity within a manageable timeframe. This relatively brief half-life is advantageous for reducing long-term radiation exposure to the patient, thereby enhancing the safety profile of treatments involving At-211.
Applications in Medicine
The primary appeal of Astatine-211 lies in its potential for targeted alpha therapy (TAT), an innovative approach to cancer treatment that seeks to exploit the high linear energy transfer (LET) of alpha particles. TAT aims to maximise the therapeutic effect on cancer cells while minimising collateral damage to normal tissues, a principle that is especially important in the treatment of small, localised cancers and micrometastases.
One of the most promising areas of application for At-211 is in the treatment of brain tumours, including gliomas, which are known for their poor prognosis and limited treatment options. The ability of At-211 to deliver potent, localised radiation makes it an attractive candidate for targeting these highly aggressive and difficult-to-treat cancers. Similarly, in thyroid cancer, particularly in cases that are refractory to traditional treatments like surgery and radioiodine therapy, At-211 offers a novel therapeutic pathway by targeting cancer cells with precision and minimal impact on healthy thyroid tissue.
Ovarian cancer, another area where At-211 is being explored, presents unique challenges due to its tendency to present at advanced stages and its frequent development of micrometastatic disease. The targeted delivery of alpha radiation through At-211 could provide a significant advantage in treating such cases, offering hope for improved outcomes in a disease where advances in treatment have been elusive.
Research into the use of At-211 is also expanding into other cancers, including prostate and breast cancers, where its ability to selectively irradiate cancer cells could enhance the effectiveness of existing treatment modalities and potentially introduce new therapeutic strategies.
Astatine-211 represents a cutting-edge element in the arsenal of therapeutic nuclear medicine. Its distinctive properties as an alpha emitter enable the delivery of highly targeted radiation therapy, offering a beacon of hope for patients with cancers that are challenging to treat with conventional methods. As research and clinical trials progress, the potential of At-211 to revolutionise cancer treatment continues to unfold, promising to usher in a new era of precision oncology.
Yttrium-90: A Cornerstone in Therapeutic Nuclear Medicine
Yttrium-90 (Y-90) stands out as a pivotal radionuclide within the area of therapeutic nuclear medicine, primarily due to its unique physical characteristics and therapeutic capabilities. As a beta emitter, Y-90 possesses a medium energy level, which, coupled with its half-life of approximately 64 hours (roughly 2.67 days), endows it with a remarkable ability to treat a broad spectrum of tumours. The energy emitted by Y-90 is sufficiently potent to penetrate tissue to a few millimetres, bridging the gap between targeting surface-level cells and reaching deeper tumoral structures without excessive collateral damage to surrounding healthy tissues.
The specificity of Y-90 beta radiation is instrumental in achieving therapeutic efficacy, particularly in scenarios where the precise delivery of a significant radiation dose is required to eradicate tumour cells. This characteristic ensures that Y-90 can be utilised in a controlled manner, optimising the balance between maximising tumour cell kill rates and minimising adverse effects on neighbouring non-cancerous cells.
Applications in Medicine
The practical applications of Yttrium-90 in the medical field are diverse and impactful, particularly in the treatment of various forms of cancer. One of the most notable uses of Y-90 is in radioembolisation, a procedure that has revolutionised the approach to managing liver cancer. Radioembolisation involves the targeted delivery of Y-90 embedded microspheres directly into the liver tumours via the hepatic artery. This method allows for the precise irradiation of tumoral tissues while sparing the majority of the healthy liver, thereby offering a significant therapeutic advantage for patients with inoperable or advanced liver cancer.
Beyond liver cancer, Y-90 has also found application in the development of radiolabelled antibodies, specifically targeting non-Hodgkin’s Lymphoma (NHL). This approach, known as radioimmunotherapy (RIT), leverages the targeting capability of monoclonal antibodies to deliver Y-90 directly to lymphoma cells, thereby providing a mechanism to selectively irradiate lymphoma cells dispersed throughout the body. The effectiveness of RIT in treating lymphoma highlights the versatility of Y-90 as a therapeutic agent capable of being integrated into complex treatment paradigms to achieve improved patient outcomes.
Moreover, the ongoing exploration into the potential applications of Y-90 in other cancer types underscores the radionuclide’s versatility and adaptability. Its ability to be conjugated with various molecules and compounds enhances its potential as a tool in the broader spectrum of nuclear medicine, particularly in scenarios where precise, targeted therapy can make a significant difference in treatment outcomes.
Yttrium-90 embodies a critical component of the arsenal against cancer, facilitated by its unique properties and the innovative treatment methodologies it enables. From liver cancer radioembolisation to the targeted treatment of lymphoma through radioimmunotherapy, Y-90 continues to demonstrate its value in improving the quality of life and survival rates of patients facing cancer. As research progresses and new therapeutic techniques are developed, the role of Y-90 in therapeutic nuclear medicine is poised to expand, further solidifying its status as an indispensable tool in the fight against cancer.
Rhenium-186 and Rhenium-188
Rhenium-186 (Re-186) and Rhenium-188 (Re-188) are notable isotopes within the area of therapeutic nuclear medicine, each playing a pivotal role due to their unique radioactive properties and medical applications. Both isotopes emit beta particles, but their different half-lives and emission energies cater to various therapeutic needs, highlighting the versatility and importance of radionuclides in modern medicine.
Re-186 and Re-188 are distinguished by their physical characteristics, which dictate their suitability for specific therapeutic purposes. Re-186 has a half-life of 3.7 days, providing a sufficient window for therapeutic action without unnecessarily prolonging radioactive exposure. In contrast, Re-188, with a half-life of 17 hours, offers a more rapid decay, making it suitable for treatments where a quick therapeutic effect is desirable.
The emission of beta particles by both isotopes means they can deposit energy within a limited range of their target, minimising the impact on surrounding healthy tissues. This targeted approach is essential in nuclear medicine, where the objective is to maximise the therapeutic effect on diseased cells while minimising collateral damage.
Applications in Medicine
Treatment of Bone Metastases
One of the primary applications of Re-186 and Re-188 is in the treatment of bone metastases, a common and painful condition where cancer cells spread to bones. These radionuclides are incorporated into pharmaceuticals that specifically target bone tissue, providing dual benefits: pain relief and inhibition of tumour growth. The beta particles emitted by Re-186 and Re-188 effectively kill cancer cells in the bone, helping to manage symptoms and potentially prolong life.
Re-188, particularly with its shorter half-life and higher energy emission, is highly effective for this application. Its rapid decay and potent therapeutic effect make it especially useful for delivering targeted doses of radiation quickly and efficiently.
Liver Cancer and Skin Cancer Treatments
Beyond bone metastases, Re-188 demonstrates versatility in treating other cancers, including liver and certain skin cancer types. In the case of liver cancer, Re-188 can be used in radioembolisation therapy, where radioactive particles are delivered directly to the liver’s blood supply, targeting tumours with minimal impact on healthy liver tissue. This approach allows for a high dose of radiation to be concentrated precisely where it is needed, offering a valuable treatment option for patients with inoperable tumours.
Moreover, Re-188’s properties are being explored in the treatment of specific skin cancers, where its beta radiation can effectively target and destroy cancerous cells. This is particularly promising for superficial skin cancers, where the precision and controlled range of beta particles can achieve optimal therapeutic outcomes.
Rhenium-186 and Rhenium-188 exemplify the critical role of radionuclides in therapeutic nuclear medicine. Their unique properties, including half-lives and beta particle emissions, enable targeted treatments that can significantly alleviate suffering and improve the quality of life for patients with cancer. As research continues and these treatments become more refined, the potential of Re-186 and Re-188 in expanding and enhancing therapeutic options in nuclear medicine is immense, marking a significant step forward in the fight against cancer.
Future Prospects and Challenges in Therapeutic Nuclear Medicine
The integration of radionuclides such as Lutetium-177, Astatine-211, Yttrium-90, Rhenium-186, and Rhenium-188 into therapeutic nuclear medicine heralds a transformative era in the treatment of cancer and other diseases. With their unique properties and targeted therapeutic capabilities, these radionuclides offer hope for conditions that were once considered intractable. The potential for these radionuclides to revolutionise medical treatment is immense, yet the path forward is not without its challenges.
The Promise of Radionuclides
The promise held by these radionuclides is grounded in their ability to deliver targeted therapy to cancer cells, minimising damage to surrounding healthy tissues. This targeted approach enhances the efficacy of treatment and reduces the side effects associated with traditional cancer therapies. Moreover, the versatility of these radionuclides across a range of applications—from bone metastases to liver cancer—underscores their potential to cater to diverse medical needs.
Overcoming Challenges
Despite the promising prospects, several challenges need to be addressed to fully realise the potential of these radionuclides in therapeutic nuclear medicine:
- Long-term Effects: There is a pressing need for comprehensive research into the long-term effects of radionuclide therapy. Understanding the implications of radiation exposure over time is crucial to ensuring patient safety and improving treatment outcomes.
- Targeted Delivery Mechanisms: The development of more sophisticated delivery mechanisms is essential to enhance the precision of radionuclide therapy. Advances in molecular biology and nanotechnology could pave the way for innovative approaches that ensure radionuclides are delivered directly to cancer cells, maximising therapeutic efficacy while minimising collateral damage.
- Logistical and Regulatory Hurdles: The production, handling, and transportation of radionuclides present logistical challenges, given their radioactive nature. Moreover, stringent regulatory frameworks govern the use of radioactive materials in medicine. Navigating these logistical and regulatory hurdles is vital for the timely and safe delivery of radionuclide therapies to patients in need.
- Cost and Accessibility: The cost of radionuclide therapy can be prohibitive, limiting access for many patients. Efforts to reduce production costs and streamline treatment protocols are essential to making these therapies more accessible.
Conclusion
The radionuclides Lutetium-177, Astatine-211, Yttrium-90, Rhenium-186, and Rhenium-188 stand at the vanguard of therapeutic nuclear medicine, offering groundbreaking approaches to cancer treatment. Their unique properties and applications represent a leap forward in medical science, providing targeted, effective, and potentially life-saving treatments for a range of conditions. As the field continues to evolve, addressing the challenges and leveraging the opportunities presented by these radionuclides will be crucial. With ongoing research and development, the future of therapeutic nuclear medicine looks promising, heralding new horizons in the quest for more effective, targeted, and personalised treatment options. The journey ahead is complex, but the potential rewards for patients worldwide are vast, marking a significant stride in the battle against cancer and other debilitating diseases.
Q&A on Therapeutic Nuclear Medicine for Advanced Cancer Treatment
Q1: What is therapeutic nuclear medicine and how does it work?
A1: Therapeutic nuclear medicine uses radioactive substances (radionuclides) to identify, target, and treat a variety of diseases, including advanced cancers. When introduced into the body, radionuclides bind to molecules that naturally seek out cancer cells. Once at the tumour site, the radionuclide emits radiation that either aids diagnosis or destroys malignant cells, while aiming to minimise harm to healthy tissue.
Q2: Which radionuclides are currently considered pivotal in therapeutic nuclear medicine?
A2: Five radionuclides have gained prominence:
- Lutetium-177 (Lu-177): A beta emitter, effective for targeting small to medium-sized tumours, particularly neuroendocrine and prostate cancers.
- Astatine-211 (At-211): An alpha emitter known for its precise, high-energy radiation over a short distance, suitable for targeting small clusters of cancer cells.
- Yttrium-90 (Y-90): A beta emitter that can be used in radioembolisation for liver cancers and in radioimmunotherapy for lymphoma.
- Rhenium-186 (Re-186) and Rhenium-188 (Re-188): Beta emitters valuable for alleviating pain from bone metastases and, in the case of Re-188, for treating liver and certain skin cancers.
Q3: What advantages does Lu-177 offer in cancer therapy?
A3: Lu-177 half-life is around 6.65 days and its short-range beta radiation make it ideal for delivering a potent radiation dose directly to tumours. This precision helps target malignant cells effectively while reducing damage to surrounding healthy tissues. Lu-177 is a mainstay in Peptide Receptor Radionuclide Therapy (PRRT) for neuroendocrine tumours and is increasingly applied in treating prostate cancer, improving patient outcomes and lowering side effects.
Q4: How does At-211 differ from other radionuclides?
A4: At-211 emits alpha particles, which release a large amount of energy over a very short distance. This property allows for the targeted destruction of malignant cells without significantly affecting nearby healthy tissues. Its short half-life of about 7.2 hours also limits prolonged radiation exposure, making it highly attractive for treating brain tumours, certain thyroid cancers, ovarian cancers, and potentially other difficult-to-treat malignancies.
Q5: What role does Y-90 play in treating advanced cancers?
A5: Y-90 is extensively used in radioembolisation for liver cancers, where microspheres containing Y-90 are delivered directly to the liver’s arterial supply. This approach ensures a concentrated radiation dose is deposited in the tumour, preserving healthy liver tissue. Additionally, Y-90’s compatibility with antibodies used in radioimmunotherapy broadens its applicability, for example in treating non-Hodgkin’s Lymphoma.
Q6: How do Re-186 and Re-188 contribute to patient care?
A6: Re-186 and Re-188 both emit beta radiation and are commonly used to treat bone metastases, relieving pain and potentially slowing tumour progression. Re-188’s shorter half-life and higher energy can also benefit liver cancer therapy through radioembolisation, and it shows promise in treating certain skin cancers. These radionuclides help improve patient comfort and quality of life by reducing pain associated with bone lesions.
Q7: What are the future prospects of therapeutic nuclear medicine?
A7: As research advances, the use of these radionuclides is expected to expand, offering more targeted and tailored treatment options. Improvements in radionuclide production, refined targeting mechanisms, and better delivery systems will likely increase accessibility, safety, and effectiveness. Over time, these developments may lead to more personalised oncology treatments with fewer side effects and improved patient outcomes.
Q8: What challenges need to be addressed to maximise the benefits of these radionuclides?
A8: Key challenges include:
- Long-term Safety: Ensuring a thorough understanding of the lasting effects of radiation therapy on patients.
- Targeted Delivery: Improving delivery mechanisms so that radionuclides reach only cancerous cells.
- Logistics and Regulation: Managing the complex production, transportation, and regulatory requirements for radioactive materials.
- Cost and Accessibility: Reducing expenses and improving the infrastructure to make these therapies widely available.
Q9: How could these challenges be overcome?
A9: Progress will involve multidisciplinary collaboration among scientists, clinicians, regulatory bodies, and industry stakeholders. Advancements in molecular biology, nanotechnology, and radiopharmacy could lead to more efficient and specific targeting methods. Streamlined regulatory processes, innovations in production methods, and cost-effective approaches will be crucial for making these cutting-edge therapies broadly accessible.
Q10: Why are these developments significant for patients with advanced cancer?
A10: The shift towards targeted, personalised treatments can dramatically improve the odds of controlling cancer, prolonging life, and reducing treatment-related side effects. As researchers continue to refine and expand the applications of Lu-177, At-211, Y-90, Re-186, and Re-188, patients stand to benefit from more effective therapies that improve their quality of life and potentially offer new hope against advanced or hard-to-treat cancers.
Disclaimer
The content presented in this article is intended for informational and educational purposes only. It is not intended to serve as, nor should it be construed as, medical advice, diagnosis, or treatment recommendation. Open Medscience does not provide medical services or advice, and the information herein should not be used as a substitute for professional healthcare guidance provided by qualified medical professionals.
The article discusses current research and emerging developments in the field of therapeutic nuclear medicine, including the use of specific radionuclides such as Lutetium-177, Astatine-211, Yttrium-90, Rhenium-186, and Rhenium-188. While every effort has been made to ensure scientific accuracy and relevance at the time of publication, Open Medscience makes no guarantees regarding the completeness, accuracy, or timeliness of the information. Scientific understanding, clinical practices, and regulatory guidelines in nuclear medicine are constantly evolving and may differ across jurisdictions.
The mention of specific treatments, procedures, or medical agents does not imply endorsement by Open Medscience. Readers are strongly advised to consult their doctor, oncologist, or a licensed nuclear medicine specialist before making any decisions regarding diagnosis, treatment, or the use of radionuclide therapies.
Any views or opinions expressed in the article are those of the authors and do not necessarily reflect the official policy or position of Open Medscience, its affiliates, or contributors.
Open Medscience disclaims all liability for any direct or indirect loss, injury, or damage incurred as a result of the use or reliance upon the information provided in this article.
home » blog » radiotherapeutics »