Medical physics, a vital field at the intersection of physics and healthcare, plays a crucial role in the advancement of medical diagnostics and treatment. This discipline harnesses the principles of physics to enhance medical technology applications, from sophisticated imaging processes to precise radiation therapies. As we navigate the complexities of human health, medical physics offers a unique perspective, merging rigorous scientific methodology with clinical needs to significantly improve patient outcomes.
The historical development of medical physics dates back to the late 19th century, when Wilhelm Conrad Röntgen discovered X-rays, setting the stage for a series of innovations that have fundamentally transformed medical diagnostics and treatments. Over the decades, the field has evolved, incorporating cutting-edge technologies such as magnetic resonance imaging (MRI), computed tomography (CT), and nuclear medicine, each contributing to more accurate diagnoses and effective treatments.
Today, emerging technologies like artificial intelligence (AI), machine learning (ML), and advanced imaging techniques are reshaping the landscape of medical physics. These tools not only streamline and enhance diagnostic and therapeutic processes but also promise to make medical services more accessible worldwide. As technology advances, medical physicists face new challenges and ethical considerations, balancing the benefits of innovative technologies with patient safety and ethical medical practice.
This article looks into the core concepts, applications, and future direction of medical physics. It explores how the field continues to influence global healthcare, which is driven by technological advancements and a commitment to improving health outcomes. Through a detailed examination of its development, current impact, and potential future innovations, we gain insight into the critical role medical physics plays in the ongoing evolution of healthcare.
Historical Development of Medical Physics
Early Beginnings
The discipline of medical physics, as we understand it today, began with a groundbreaking discovery by Wilhelm Conrad Röntgen in 1895. While experimenting with cathode rays in his laboratory, Röntgen identified a new type of radiation, which he called X-rays. This discovery was monumental, as it allowed for the visualisation of internal structures of the body without invasive surgery. Röntgen’s first notable experiment involved taking an X-ray photograph of his wife’s hand, showcasing not just the soft tissues but also the bones and her wedding ring, thus demonstrating the potential medical applications of X-rays.
This discovery quickly found its way into diagnostic medicine, with the first use of X-rays to locate bullets in wounded soldiers during the Balkan War in 1897. It revolutionised the approach to diagnosis and treatment, reducing unnecessary surgeries and providing unprecedented insights into the human body’s internal workings. For his contributions, Röntgen was awarded the first Nobel Prize in Physics in 1901, acknowledging the immense potential of his discovery for medical science.
The 20th Century: Expansion and Specialisation
As the 20th century progressed, the field of medical physics experienced significant growth, both in the development of new technologies and the specialisation of the field. The advent of new imaging modalities extended beyond basic X-rays into more complex systems that offered new perspectives on human anatomy and physiology.
The Development of Computed Tomography
In 1972, British engineer Godfrey Hounsfield developed computed tomography (CT), which uses computer-processed combinations of many X-ray measurements taken from different angles to produce cross-sectional (tomographic) images of specific areas of a scanned object. This allows users to see inside the object without cutting it open. Simultaneously developed by Hounsfield and South African-born physicist Allan Cormack, CT imaging represented a leap forward in medical imaging, providing three-dimensional views and greatly enhancing the detail with which doctors could assess and diagnose conditions. The development of CT was recognised with a Nobel Prize in Physiology or Medicine in 1979, shared by Hounsfield and Cormack.
Advances in Magnetic Resonance Imaging
Another significant advancement was the development of magnetic resonance imaging (MRI), which emerged from the principles of nuclear magnetic resonance (NMR), a technique used by chemists to gain molecular information. In the 1970s, Raymond Damadian, an American physician and scientist, demonstrated that MRI could be used to scan the human body and produce clear images of tissues and organs. Unlike X-rays and CT scans, which use ionising radiation, MRI uses strong magnetic fields and radio waves to produce detailed images of the organs and tissues in the body. This was particularly useful for imaging the brain, muscles, and connective tissues, areas where X-rays provided limited information.
Radiation Therapy Developments
Parallel to diagnostic advancements, medical physics also made significant contributions to therapeutic practices, particularly in the treatment of cancer. The development of radiation therapy, which uses high doses of radiation to kill cancer cells and shrink tumours, benefited greatly from the work of medical physicists. Techniques such as brachytherapy, where radioactive sources are placed inside or next to the area requiring treatment, and teletherapy, where the radiation source is at a distance from the body, were refined and made more effective with the understanding and calculations provided by physicists.
Specialisation and Professional Development
As these technologies developed, the need for specialised knowledge in medical physics became clear, leading to the establishment of training programs and certification processes. Medical physics as a distinct profession came into prominence, with roles defined not only in research and development but also in clinical settings to ensure the safe and effective application of these technologies. Professional bodies, such as the American Association of Physicists in Medicine (AAPM) in the United States, were established to set standards, promote professional development, and support the integration of physics into the medical landscape.
Core Concepts in Medical Physics
Diagnostic Imaging
Medical imaging is a cornerstone of modern medicine and a significant area within medical physics. It includes a variety of techniques that utilise different physical principles to create detailed images of the human body. These images are crucial for accurate diagnosis, treatment planning, and monitoring of diseases.
X-ray Radiography
The most familiar form of medical imaging is X-ray radiography. It uses X-ray radiation, a form of electromagnetic radiation, to create images of the internal structures of the body. When X-rays pass through the body, they are absorbed by different tissues at different rates. Bones, for example, absorb more X-rays than soft tissues, allowing for the clear visualisation of skeletal structures. This technique is essential not only in diagnosing fractures but also in detecting conditions such as lung infections and certain types of tumours.
Ultrasound Imaging
Ultrasound imaging, or sonography, uses high-frequency sound waves to create images of the inside of the body. A small probe called a transducer emits sound waves, which bounce off tissues and return to the probe. The time it takes for the echo to return is used to create real-time images of the internal organs. This method is particularly useful in obstetrics for monitoring the development of the fetus, as well as in cardiology for examining the heart’s structure and function.
Magnetic Resonance Imaging (MRI)
MRI uses powerful magnets and radio waves to generate images of the body. Unlike X-rays, MRI does not involve ionising radiation, making it a safer alternative for imaging soft tissues such as the brain, spinal cord, and muscles. The technique exploits the magnetic properties of atoms within the body. Certain atomic nuclei align with the field when placed in a strong magnetic field. Radio waves are then used to disrupt this alignment, and the MRI sensors detect the energy released as the nuclei return to their original alignment.
Computed Tomography (CT)
Computed tomography (CT) combines X-ray equipment with computers to produce multiple images or pictures of the inside of the body. These cross-sectional images can be assembled to create a comprehensive three-dimensional model of a patient’s internal structures. CT scans are exceptionally good at imaging a combination of soft tissue, bone, and blood vessels and are crucial for diagnosing diseases such as cancer and monitoring its progression.
Radiation Therapy
Radiation therapy is another critical aspect of medical physics, focusing on the use of high-energy radiation to treat diseases, primarily cancer. Medical physicists play a vital role in this area, from the initial treatment planning to the precise delivery of therapy.
Treatment Planning
The process begins with treatment planning, which involves determining the correct dose of radiation to effectively treat a tumour while minimising exposure to the surrounding healthy tissues. Medical physicists use sophisticated software and computing tools to calculate and simulate the best radiation delivery angles and doses.
Techniques of Delivery
There are several techniques of radiation delivery, including external beam radiation therapy, which directs high-energy beams of radiation at the tumour from outside the body, and brachytherapy, where radioactive sources are placed inside or near the tumour. Each technique requires meticulous planning to ensure the radiation targets only the cancerous cells and causes the least possible damage to normal tissue.
Safety and Efficacy
Ensuring the safety and efficacy of radiation therapy is paramount. Medical physicists are responsible for calibrating and maintaining the equipment used in radiation therapy to ensure it delivers the precise amount of radiation prescribed by the radiation oncologist. They also develop and oversee quality control procedures to maintain high safety standards.
Nuclear Medicine
Nuclear medicine is a specialised area of medical physics that uses small amounts of radioactive materials, or radiopharmaceuticals, to diagnose and treat disease. It provides unique information that often cannot be obtained using other imaging procedures.
Diagnostic Techniques
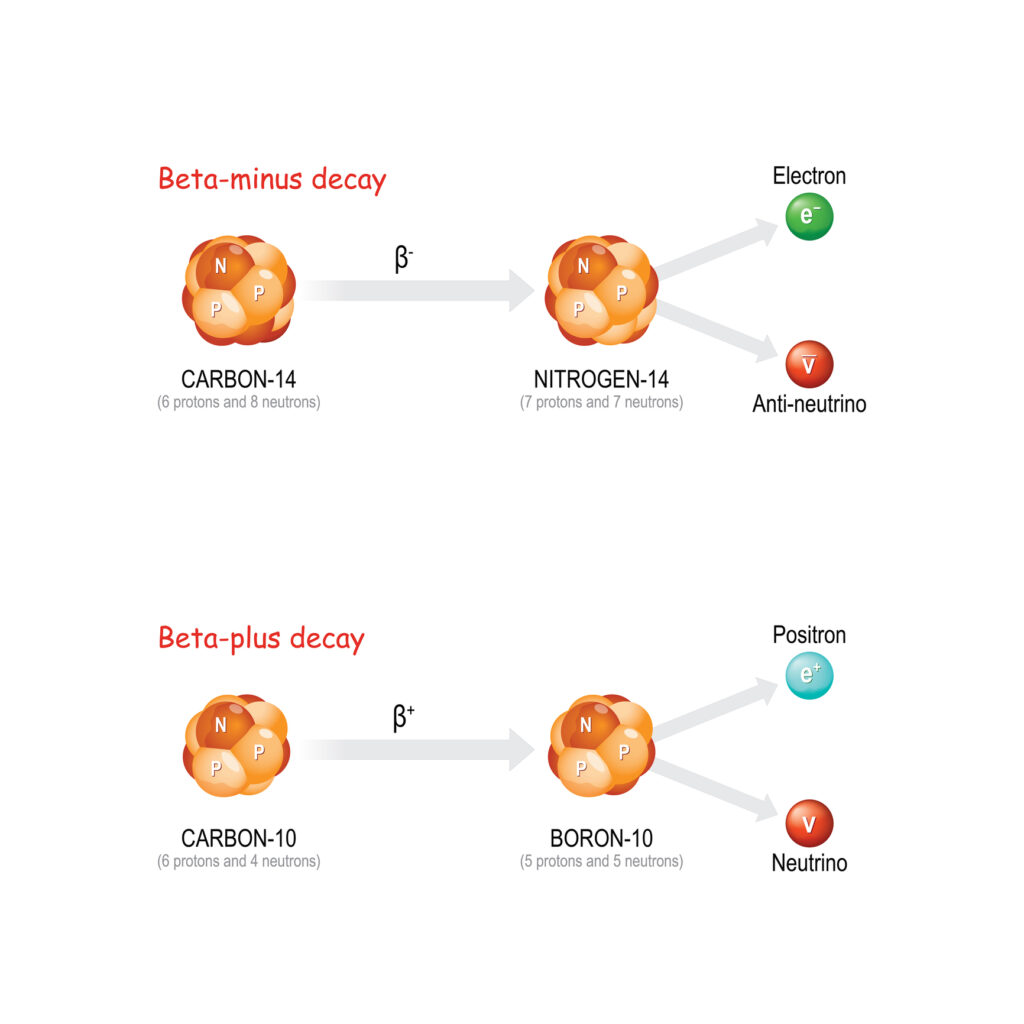
In diagnostic nuclear medicine, techniques such as positron emission tomography (PET) and single-photon emission computed tomography (SPECT) are used to visualise the dynamic chemical and biological processes taking place in the body. PET scans detect the gamma rays emitted by a tracer (typically fluorodeoxyglucose, which includes a radioactive atom) introduced into the body. This tracer accumulates in organs and tissues, highlighting areas of high chemical activity, which often correspond to disease sites.
Therapeutic Applications
Nuclear medicine is not limited to diagnostics; it also includes therapeutic procedures, such as the treatment of hyperthyroidism or certain types of cancer using radiopharmaceuticals. These radioactive substances can target specific organs, tissues, or cells, providing treatment by damaging the DNA of the target cells, thus impeding their ability to grow and divide.
Optimising Imaging Techniques
In diagnostic imaging, medical physicists contribute to the refinement and optimisation of techniques such as MRI, CT, and ultrasound. Their expertise in the underlying physics of these technologies enables them to improve image quality, reduce scanning times, and enhance the overall safety of these procedures. For instance, in MRI, physicists work to develop sequences that can provide clearer images with less noise. In contrast, in CT, their work on dose reduction techniques is critical to minimising patient exposure to ionising radiation.
Ensuring Patient Safety
The safety of patients during procedures involving radiation or high-energy equipment is a paramount concern in medical physics. Physicists are responsible for the rigorous testing and maintenance of equipment to ensure it meets safety standards. They also develop safety protocols to protect both patients and healthcare workers from accidental exposure to radiation, contributing to a safer healthcare environment.
Research and Development
Medical physics is inherently linked to research and development, with continuous efforts aimed at advancing technology to improve diagnostic and therapeutic techniques.
Developing New Technologies
Innovations in medical physics can lead to the development of new technologies that revolutionise patient care. For example, the advent of digital imaging over traditional film has significantly improved the way images are processed, stored, and interpreted, leading to quicker and more accurate diagnoses. Furthermore, recent advances in areas like proton therapy and stereotactic radiosurgery offer new possibilities for treating cancers that are difficult to address with conventional radiation therapy techniques.
Enhancing Therapeutic Capabilities
Medical physicists are at the forefront of enhancing therapeutic capabilities through technology. For instance, in radiation therapy, the development of intensity-modulated radiation therapy (IMRT) and volumetric-modulated arc therapy (VMAT) are examples of how medical physics has contributed to more precise and effective cancer treatments. These technologies allow for the radiation dose to be shaped exactly to the size and shape of the tumour, thereby maximising the dose to the tumour while sparing surrounding healthy tissue.
Impact on Patient Care
The research and development activities in medical physics directly and significantly impact patient care. Innovations such as real-time imaging during surgical procedures and the use of AI to enhance image analysis are examples of how research in medical physics translates into better clinical outcomes and more efficient patient care.
Education and Training
Education and training are critical components of medical physics applications, ensuring that the next generation of medical physicists and related professionals is well-prepared to apply these advanced technologies safely and effectively.
Training Medical Physicists
Training programs for medical physicists are rigorous, often involving a combination of a master’s or doctoral degree followed by clinical training in hospitals. These programs are designed to cover a broad spectrum of knowledge, from the fundamental principles of physics to specific medical applications, ensuring that graduates are competent to work in diverse clinical environments.
Educating Healthcare Professionals
Medical physicists also play a key role in educating other healthcare professionals, including doctors, nurses, and radiologic technicians, about the safe and effective use of medical technologies. This education often includes training on radiation safety, the principles of medical imaging, and the basics of radiobiology, which are essential for minimising risks in clinical settings.
Contributing to Continuing Education
The field of medical physics is ever-evolving, and continuing education is vital to keep healthcare professionals updated on the latest developments and technologies. Medical physicists contribute to these educational efforts through workshops, seminars, and conferences, where they share their knowledge and research findings with the broader medical and scientific communities.
Challenges and Ethical Considerations in Medical Physics
Technological Challenges
The field of medical physics is continually evolving, driven by rapid technological advancements. While these advancements are beneficial, they present several significant challenges for medical physicists, healthcare institutions, and the broader medical community.
Keeping Pace with Advancements
One of the primary challenges is the pace at which new technologies are developed and introduced into the clinical setting. Medical physicists must constantly update their knowledge and skills to stay current with the latest developments in imaging techniques, radiation therapy, and medical equipment. This requires ongoing education and training, which can be resource-intensive.
Integration of New Technologies
Integrating new technologies into existing healthcare systems poses another challenge. Each new piece of equipment or software comes with its own set of requirements for installation, maintenance, and staff training. Medical physicists play a crucial role in this process, ensuring that new technologies are integrated smoothly and that they interact effectively with other systems, which is essential for delivering coherent and reliable patient care.
Ensuring Safety and Efficacy
As technologies become more complex, ensuring their safety and efficacy becomes increasingly challenging. Medical physicists are tasked with developing and enforcing standards and protocols to test new equipment and procedures thoroughly before they are approved for clinical use. This includes rigorous calibration and regular maintenance of equipment, as well as validation of software used for diagnostic and therapeutic purposes.
Ethical Considerations
The application of advanced technologies in medicine is not only a matter of technical feasibility but also of ethical importance. Medical physicists, like all healthcare professionals, must navigate a landscape filled with ethical dilemmas and decisions.
Balancing Risk and Innovation
One of the most significant ethical challenges in medical physics is balancing the potential benefits of new, cutting-edge technologies against the risks they may pose to patients. Innovative treatments such as new forms of radiation therapy or experimental imaging techniques can offer substantial improvements in patient care, but they may also come with unknown risks. Medical physicists are responsible for ensuring that any new treatment is based on sound scientific evidence and that it is implemented in a way that prioritises patient safety.
Patient Consent and Information
Ensuring informed consent is another crucial ethical consideration. Patients must be adequately informed about the risks and benefits of any new procedure involving advanced technology. This involves translating complex medical and technical information into an understandable format for patients, enabling them to make informed decisions about their treatments. Medical physicists and other healthcare providers have a duty to ensure that patients are fully informed and that their consent is obtained ethically.
Privacy and Data Security
The increased use of digital technologies in medical physics also raises concerns about data privacy and security. Medical imaging and radiation therapy often involve generating, storing, and sharing large amounts of sensitive patient data. Medical physicists must ensure that these data are handled securely and in compliance with relevant privacy laws and regulations to protect patient confidentiality.
Resource Allocation
Finally, the introduction of expensive new technologies in healthcare settings often leads to ethical questions regarding resource allocation. Decisions must be made about which technologies to invest in, considering the potential benefits to patient outcomes and the overall cost to the healthcare system. These decisions can have profound implications, especially in resource-limited settings, and must be guided by ethical principles that prioritise fairness and equity in patient care.
The Future of Medical Physics
Emerging Technologies
The field of medical physics is poised for a transformative era, propelled by rapid technological advancements. Innovations such as artificial intelligence (AI), machine learning (ML), and augmented reality (AR) are set to redefine the landscape of medical diagnostics and treatment, enhancing the precision and effectiveness of medical interventions.
Artificial Intelligence and Machine Learning
AI and ML are poised to revolutionise medical physics by improving diagnostic imaging and treatment planning accuracy and efficiency. AI algorithms can analyse large volumes of imaging data quickly and with high precision, identifying patterns that the human eye might miss. This capability is particularly promising in the early detection of diseases such as cancer, where early diagnosis can significantly enhance treatment success rates. Furthermore, AI-driven systems are being developed to automate routine tasks in radiation therapy planning, such as contouring, which involves delineating the boundaries of tumours and critical organs in imaging scans.
Augmented and Virtual Reality
Augmented reality and virtual reality technologies are finding applications in training and in the execution of complex medical procedures. AR, for instance, can superimpose a patient’s imaging data onto their body during surgery, providing real-time guidance to surgeons. Virtual reality, on the other hand, is being used for immersive training environments where medical physicists and other healthcare professionals can practice procedures in a risk-free, virtual setting before performing them on patients.
Advanced Imaging Technologies
Emerging imaging technologies continue to enhance the capabilities of medical diagnostics. Techniques such as photoacoustic imaging, which combines optical and ultrasound technology, offer new possibilities for visualising the microscopic structure of tissues without the need for invasive biopsies. Similarly, improvements in molecular imaging allow for more precise targeting of diseases at a cellular and molecular level, facilitating personalised treatment strategies tailored to the unique genetic makeup of a patient’s condition.
Global Impact
The global impact of advancements in medical physics cannot be overstated. As technology progresses, its integration into medical practices worldwide has the potential to significantly improve healthcare outcomes across diverse populations.
Bridging the Healthcare Gap
Advanced medical technologies developed through medical physics are increasingly being deployed in low- and middle-income countries, helping to bridge the gap in healthcare access and quality. For example, portable and cost-effective imaging devices are making diagnostic services more accessible in remote and underserved areas, thereby improving early detection and treatment of diseases.
Collaboration and Knowledge Sharing
The future of medical physics also sees an increase in global collaboration and knowledge sharing, facilitated by digital platforms that allow medical physicists and other professionals to exchange information and best practices. This collaborative environment helps to accelerate innovation and the global adoption of best practices in medical physics.
Ethics and Accessibility
As these technologies develop, there is also an increased focus on ethical considerations and the accessibility of advanced medical technologies. Ensuring equitable access to these innovations becomes a priority, requiring policy frameworks that promote fairness and inclusivity in global health.
Conclusion
Medical physics is a dynamic and ever-evolving field that blends the rigorous discipline of physics with the compassionate care of medicine. Its applications, from advanced diagnostic imaging to precision radiation therapy, underscore its vital role in modern healthcare. As we look to the future, the field is set to continue its trajectory of innovation and influence, driven by technological advances and a commitment to improving patient outcomes worldwide.
The ongoing integration of AI, ML, and novel imaging technologies into medical physics is transforming the way diseases are diagnosed and treated. These technologies promise to enhance the precision and effectiveness of medical interventions and aim to make healthcare more accessible and equitable across the globe. As medical physics continues to evolve, it remains at the forefront of medical innovation, shaping the future of healthcare in profound and lasting ways.
Disclaimer
The content of this article, “What is Medical Physics? An Overview”, is intended for informational and educational purposes only. While Open Medscience strives to ensure the accuracy and relevance of the information presented, it should not be considered a substitute for professional medical advice, diagnosis, or treatment. Readers are advised to consult qualified healthcare professionals or medical physicists regarding specific medical conditions or technologies.
Any mention of medical procedures, technologies, or innovations is not an endorsement or recommendation by Open Medscience. The article reflects the state of knowledge as of July 2024 and may not include the latest developments in the field. Open Medscience does not accept any liability for errors, omissions, or outcomes arising from the use of the information contained herein.
Links to third-party websites, where provided, are for convenience and do not imply endorsement. The views expressed are those of the original author(s) and do not necessarily reflect the views of Open Medscience.
home » blog » medical physics »