Summary: The use of radioactivity in cancer treatment has revolutionised modern medicine, providing both effective therapeutic strategies and diagnostic advancements. This article examines the types of radiation therapies available, their mechanisms of action, benefits, and associated risks while exploring the promising future that research and innovation hold in this domain.
Introduction to Radioactive Cancer Treatment
The concept of using radiation to combat cancer dates back over a century and remains one of the most significant breakthroughs in oncology. Radioactive cancer treatment leverages high-energy particles or waves to target and destroy cancerous cells, impeding their ability to grow and divide. This approach has become a cornerstone in cancer care, playing a crucial role either as a primary treatment or as a complementary measure alongside surgery and chemotherapy.
Understanding Radiation Therapy
Radiation therapy utilises specific forms of ionising radiation to damage the DNA within cancer cells, triggering cellular death or preventing further cell division. The key forms of radiation therapy include:
- External Beam Radiation Therapy (EBRT): EBRT is the most common form of radiation therapy and involves the use of high-energy X-rays or proton beams directed at the tumour from outside the body. Techniques such as Intensity-Modulated Radiation Therapy (IMRT) and Stereotactic Radiosurgery (SRS) allow for precise targeting, sparing nearby healthy tissue.
- Internal Radiation Therapy (Brachytherapy): Brachytherapy entails placing radioactive sources directly inside or next to the tumour. This method allows for a high dose of radiation in a localised area and is often employed in treating cancers such as cervical, prostate, and breast cancer.
- Systemic Radiation Therapy: Systemic treatment involves the oral or intravenous administration of radioactive substances that travel through the bloodstream to target cancerous cells. Radioisotopes such as iodine-131 and radium-223 are commonly used for thyroid and bone cancers, respectively.
Mechanism of Action: How Radiation Works Against Cancer
Radiation therapy operates on the principle of ionisation, where energy particles create charged particles within the cancer cells. This process results in:
- DNA Damage: Ionising radiation damages the DNA in cancer cells, either directly or indirectly, through the production of free radicals. This DNA damage disrupts the replication process, eventually leading to cell death.
- Cell Cycle Disruption: Cancer cells are more vulnerable to radiation than healthy cells due to their rapid division. Radiation targets these rapidly dividing cells, ensuring a higher impact on malignant growths.
Advancements in Radiation Technology
The field of radiation oncology has witnessed significant technological advancements that have enhanced the efficacy and precision of treatments. Key innovations include:
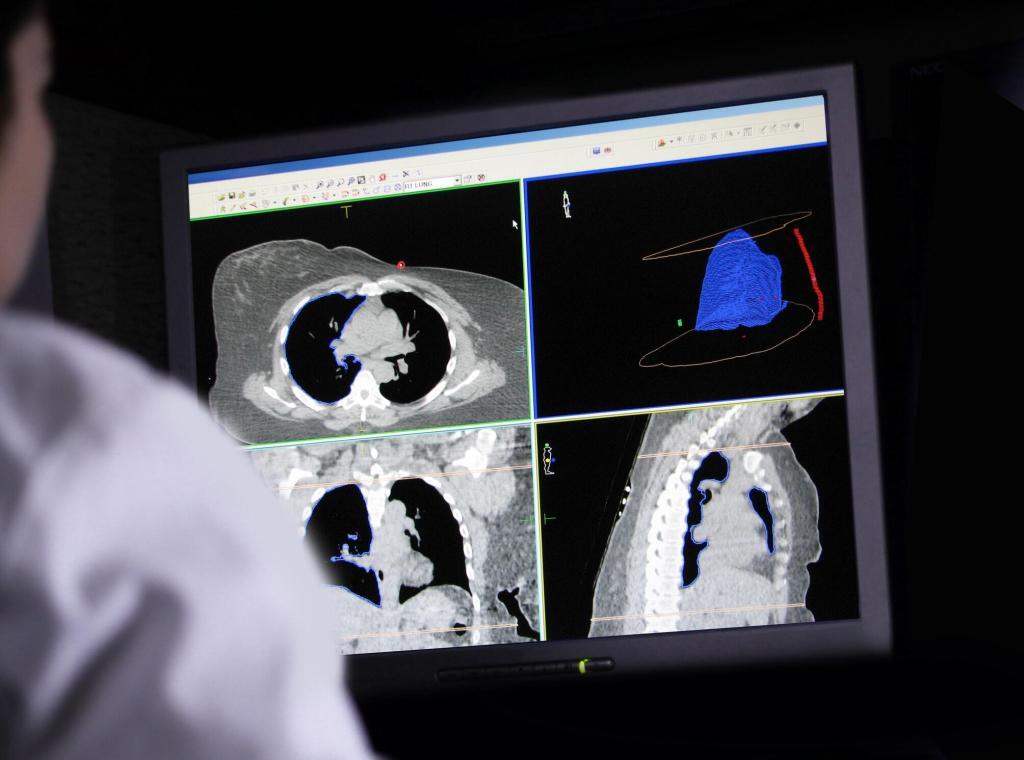
- Image-Guided Radiation Therapy (IGRT): IGRT uses imaging technologies such as CT scans and MRIs during radiation sessions to monitor and adjust treatment delivery in real-time. This ensures more accurate targeting of tumours that may shift due to patient movement or changes in organ positioning.
- Proton Beam Therapy: Proton therapy represents a cutting-edge approach wherein protons, rather than x-rays, are used to treat cancer. Due to the physical properties of protons, they release their energy at a precise depth (the Bragg peak), minimising damage to surrounding healthy tissues. This technique is particularly beneficial for treating tumours near critical organs or in paediatric patients.
- Stereotactic Body Radiation Therapy (SBRT): SBRT delivers a highly concentrated dose of radiation in fewer sessions, focusing on small, well-defined tumours. Its precision reduces the impact on adjacent healthy tissue and shortens treatment duration, which is advantageous for patients.
Benefits of Radioactive Cancer Treatments
Radiation therapy presents several advantages in the management of cancer:
- Minimally Invasive: Unlike surgery, radiation therapy is a non-invasive or minimally invasive treatment, offering a less traumatic option for patients.
- Organ Preservation: By precisely targeting tumours, radiation therapy can preserve organs and structures, maintaining better functionality and quality of life.
- Combinational Synergy: Radiation therapy can be combined with other treatments, such as chemotherapy or immunotherapy, to enhance overall treatment efficacy.
- Pain Management: Palliative radiation therapy is used to alleviate symptoms in patients with advanced cancer, improving their quality of life by reducing pain and discomfort.
Risks and Side Effects
While radiation therapy offers numerous benefits, it is not without risks. Common side effects include:
- Short-Term Side Effects: These may include fatigue, skin irritation, and localised hair loss at the treatment site. Gastrointestinal discomfort, nausea, and other symptoms can occur depending on the treated area.
- Long-Term Side Effects: Some patients may experience long-term effects such as fibrosis, organ damage, or secondary cancers, though these risks have been reduced with advancements in radiation delivery techniques.
- Potential Impact on Healthy Tissue: High doses of radiation can inadvertently damage nearby healthy cells, leading to complications like scarring or impaired organ function.
Safety Measures and Radiation Shielding
Safety protocols in radiation oncology are stringent to protect both patients and healthcare workers. These include:
- Patient Safety: Shielding techniques and precise dosimetry calculations help ensure that radiation doses are optimised to minimise exposure to healthy tissues.
- Professional Safety: Medical personnel use protective gear and maintain safe distances or barriers when handling radioactive materials. Advanced technology, such as automated treatment planning systems, further enhances safety measures.
The Role of Radiopharmaceuticals in Cancer Treatment
Radiopharmaceuticals are compounds that combine radioactive isotopes with drugs targeting specific cancer cells. These substances are used for both diagnostic and therapeutic purposes:
- Diagnostic Radiopharmaceuticals: Techniques such as Positron Emission Tomography (PET) and Single Photon Emission Computed Tomography (SPECT) rely on radiopharmaceuticals to create detailed images of cancerous tissues, aiding in accurate diagnosis and treatment planning.
- Therapeutic Radiopharmaceuticals: Radiopharmaceuticals can deliver radiation directly to cancer cells, reducing damage to surrounding healthy tissue. Examples include lutetium-177 for treating neuroendocrine tumours and iodine-131 for thyroid cancer treatment.
Emerging Trends and Future Prospects
The future of radiation therapy holds exciting potential, driven by research and technological innovation. Noteworthy trends include:
- Personalised Treatment Plans: Advances in genetic and molecular profiling allow for tailored radiation treatments based on individual tumour characteristics, optimising efficacy and reducing side effects.
- AI and Machine Learning: Artificial intelligence is increasingly being used to enhance treatment planning, predict patient responses, and improve workflow efficiency in radiation oncology.
- Combination with Immunotherapy: Combining radiation therapy with immunotherapy is an emerging field that seeks to harness the body’s immune response to improve treatment outcomes. Radiation can act as an immune activator, enhancing the effectiveness of immune checkpoint inhibitors.
- Radiogenomics: The study of how genetic variation affects patient responses to radiation is advancing rapidly. Radiogenomics aims to identify genetic markers that predict how a tumour will respond to radiation, allowing for even more personalised treatment approaches.
Ethical and Accessibility Considerations
Equity in cancer treatment remains a concern. Access to cutting-edge radiation therapy may be limited by geographic and economic factors, leading to disparities in cancer care. Ensuring global access to modern radiation treatments is a priority for international health organisations.
Ethical considerations also encompass the balance between the potential benefits and risks of radiation exposure. Informed consent, patient education, and transparent communication are essential components of ethical radiation oncology practices.
Conclusion
Radioactive cancer treatment stands as a testament to the remarkable progress in modern medicine. With continued advancements in technology and an enhanced understanding of cancer biology, radiation therapy is poised to become even more effective and tailored to individual patients. By combining traditional methods with innovative approaches, such as AI integration and personalised radiopharmaceuticals, the future holds promise for improved patient outcomes and the potential for a higher quality of life post-treatment.
Disclaimer
The content provided in this article is for informational purposes only and does not constitute medical advice, diagnosis, or treatment. Open Medscience does not endorse any specific therapy, treatment, or medical professional referenced herein. While efforts have been made to ensure accuracy, the information may not reflect the most current research or clinical guidelines.
Readers should consult a qualified healthcare professional before making decisions about any medical condition or treatment option, including radiation therapy. The potential benefits, risks, and appropriateness of any medical intervention can vary depending on individual circumstances.
Open Medscience assumes no responsibility or liability for any consequences arising from the use of the information contained in this publication.
You are here: home » diagnostic medical imaging blog »