The integration of artificial intelligence into modern healthcare has brought significant changes to how diseases are detected, diagnosed, and managed. Among the most transformative applications is AI-powered radiology, which enhances clinicians’ ability to identify diseases at an early stage—sometimes before symptoms even appear. This combination of human expertise and machine intelligence is shaping a new future for diagnostic imaging, making healthcare more predictive, precise, and personalised.
The Shift from Reactive to Proactive Medicine
Traditional medical approaches have been mainly reactive. Patients seek help once symptoms develop, prompting diagnostic tests and subsequent treatments. However, many diseases, including cancer, cardiovascular disorders, and neurological conditions, progress silently long before clinical signs emerge. By the time they are discovered, they may already be advanced, reducing treatment success and survival rates.
Artificial intelligence is changing this approach. With the ability to analyse medical images rapidly and in great detail, AI-powered systems can identify subtle changes that might be invisible to the human eye. This enables earlier detection of abnormalities, offering a chance for intervention when conditions are still treatable. In this way, AI in radiology is not only improving diagnostic accuracy but also helping healthcare systems shift towards preventive and predictive models of care.
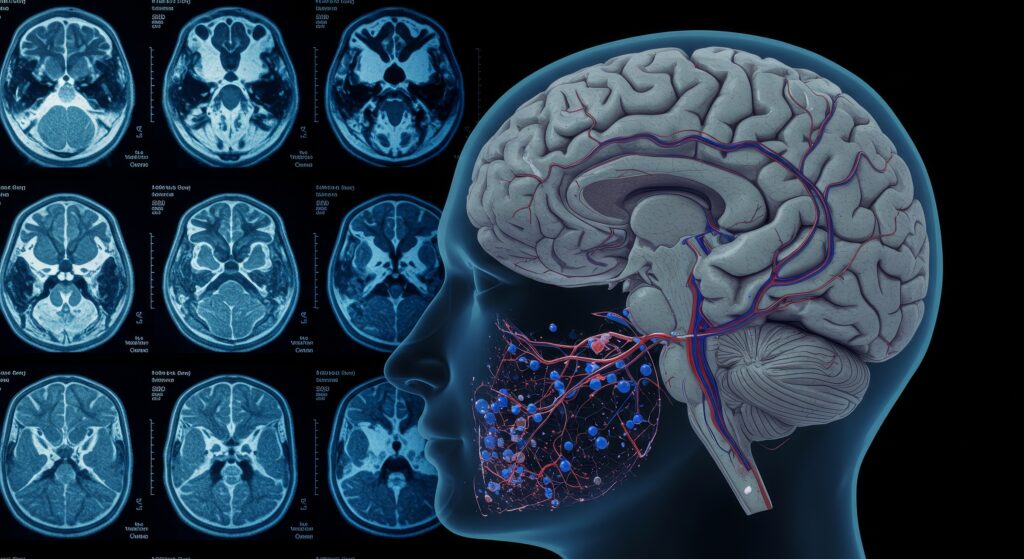
The Role of AI in Modern Radiology
Radiology has always been central to disease detection. Techniques such as X-ray, CT, MRI, PET, and ultrasound provide non-invasive insights into the human body. Yet, the sheer volume of imaging data produced daily has made it increasingly difficult for radiologists to keep pace. Studies have shown that the number of imaging studies per radiologist has increased dramatically over the last two decades. AI addresses this challenge by acting as a digital assistant that processes vast amounts of data quickly and accurately.
AI systems use algorithms based on deep learning—a subset of machine learning inspired by the human brain’s neural networks. These algorithms are trained using thousands or even millions of medical images labelled by experts. Over time, the system learns to recognise patterns, identify abnormalities, and even predict outcomes. Once trained, AI can interpret new images independently, highlighting areas of concern for human review.
Detecting Cancer at Its Earliest Stage
One of the most significant benefits of AI in radiology is its application in oncology. Early cancer detection is critical, as it dramatically improves survival rates and treatment options. In breast cancer screening, for instance, AI systems have been developed to analyse mammograms with sensitivity comparable to or exceeding that of human radiologists. These algorithms can identify microcalcifications and subtle tissue distortions that might indicate the presence of early-stage tumours.
Similarly, in lung cancer detection, AI-powered analysis of CT scans can detect minute nodules that could be easily missed in manual readings. The AI software measures their size, shape, and density, helping radiologists decide whether further testing or monitoring is required. In some cases, AI has even demonstrated the ability to predict whether a nodule is likely to be malignant based on its radiomic features—patterns in pixel intensity and texture invisible to the naked eye.
Colorectal and prostate cancers are also benefiting from AI-driven imaging analysis. Algorithms designed to review MRI and CT images can assist clinicians in differentiating between benign and malignant lesions and assessing tumour staging with improved precision. These tools not only speed up diagnosis but also reduce the number of unnecessary biopsies and procedures.
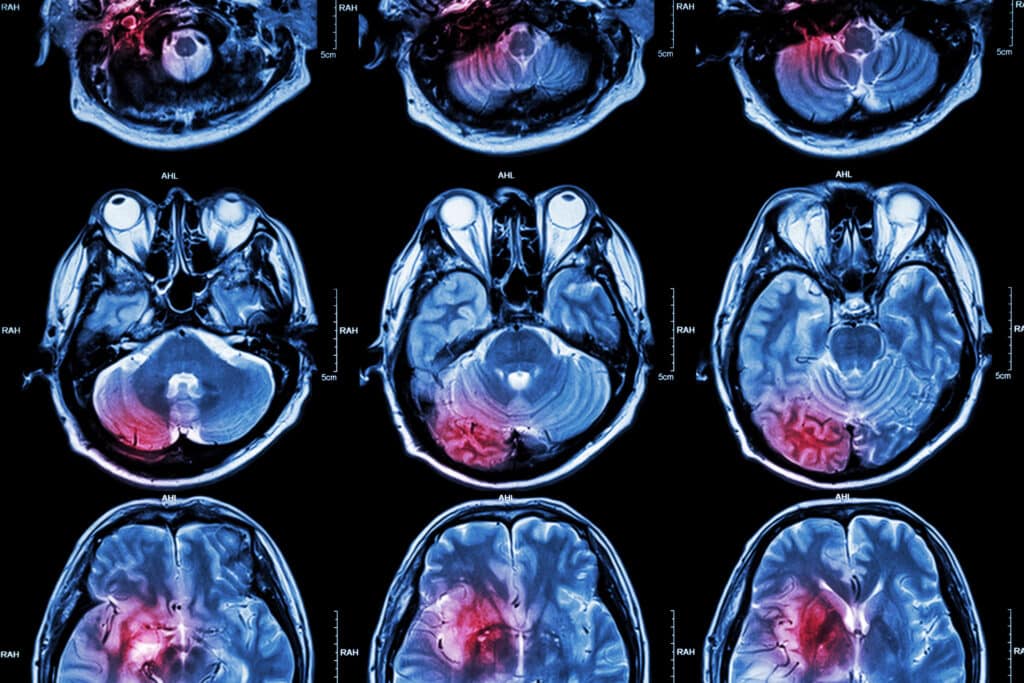
Advancements in Neurological Imaging
AI-powered radiology is also proving invaluable in detecting neurological diseases such as Alzheimer’s, Parkinson’s, and multiple sclerosis. In many cases, these disorders develop gradually, and structural or functional changes in the brain occur long before clinical symptoms appear.
For Alzheimer’s disease, AI algorithms trained on brain MRI scans can detect subtle changes in grey matter volume and patterns of brain atrophy associated with early cognitive decline. Some systems integrate MRI data with PET scans or cerebrospinal fluid biomarkers to improve diagnostic accuracy and predict the likelihood of progression from mild cognitive impairment to Alzheimer’s.
In stroke management, AI tools have revolutionised emergency care. Rapid identification of vessel blockages and assessment of tissue viability are essential for deciding whether a patient is eligible for clot-removal therapies. AI can automatically process CT or MRI scans within minutes, generating colour-coded maps that show areas of the brain affected by reduced blood flow. This enables faster decision-making and can save crucial minutes in treatment.
Parkinson’s disease diagnosis has also been enhanced through AI-driven analysis of brain imaging and motion data. Machine learning models can identify specific patterns of dopaminergic degeneration in PET or SPECT scans, supporting earlier and more reliable detection of the disease.
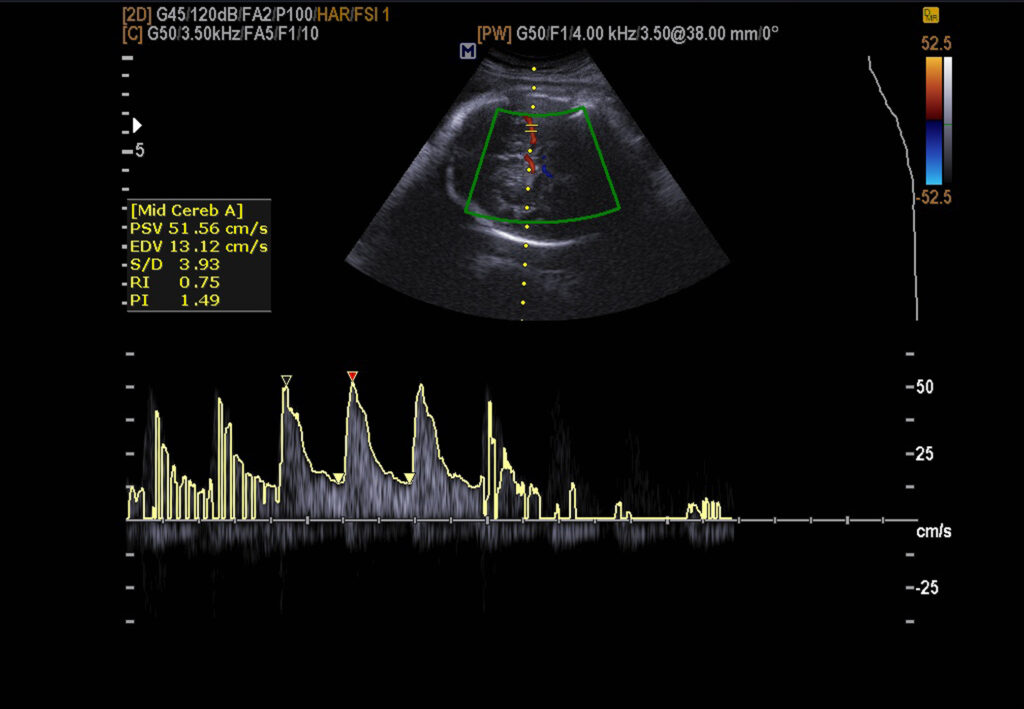
Cardiovascular Disease and Predictive Imaging
Cardiovascular conditions remain the leading cause of death globally, but many can be prevented or mitigated through early detection. AI-powered radiology has become instrumental in this area, particularly in analysing cardiac CT and MRI scans.
For instance, AI can automatically quantify coronary artery calcium scores, assess plaque composition, and evaluate blood flow dynamics. This enables clinicians to identify patients at risk of heart attack or stroke even before symptoms occur. Algorithms can also detect subtle changes in heart structure and function, such as early signs of left ventricular dysfunction, which might indicate the onset of heart failure.
In echocardiography, AI assists by automating measurements that would otherwise require manual tracing, such as ejection fraction or chamber volume. This reduces operator variability and improves consistency between examinations. By providing real-time feedback during scans, AI systems ensure high-quality images are acquired, reducing the need for repeat procedures.
Beyond Detection: AI as a Decision-Support Tool
While much focus is placed on AI’s ability to detect disease, its role extends far beyond diagnosis. Once abnormalities are identified, AI can support clinical decision-making by suggesting next steps, predicting disease progression, and even tailoring treatment strategies.
Radiomics—a field that extracts quantitative data from medical images—has enabled the development of predictive models that correlate imaging features with genetic, molecular, and clinical information. This combination of imaging and data science underpins precision medicine, in which treatment is tailored to an individual’s unique characteristics.
AI tools are also being integrated into multidisciplinary workflows. For example, during cancer treatment planning, AI can help oncologists and radiologists assess tumour response to therapy by comparing serial imaging scans. It can automatically measure tumour shrinkage or progression, ensuring that treatment adjustments are based on objective evidence.
Reducing Human Error and Workload
Fatigue and workload pressures are well-recognised factors contributing to diagnostic errors in radiology. With the increasing volume of scans and complexity of imaging studies, maintaining accuracy and efficiency is challenging. AI provides a solution by acting as a second reader, flagging potential abnormalities and ensuring no subtle details are overlooked.
AI-powered triage systems are already in use in some hospitals. They automatically prioritise urgent cases—for instance, flagging CT scans that may show signs of intracranial haemorrhage or pneumothorax—so radiologists can review them immediately. This improves workflow efficiency and ensures that patients with critical conditions receive timely attention.
Moreover, AI can automate repetitive administrative tasks such as report generation, lesion measurements, and comparison with previous scans. By streamlining these processes, radiologists can dedicate more time to interpreting complex cases and communicating with patients and clinical teams.
Overcoming Challenges and Limitations
Despite its potential, the adoption of AI in radiology is not without challenges. Data quality, algorithm transparency, and clinical validation remain central concerns. AI systems are only as good as the data used to train them. If training datasets lack diversity or contain biases, the resulting models may perform poorly across different patient populations.
Another issue is interpretability. Deep learning algorithms are often considered “black boxes” because their internal decision-making processes are challenging to understand. This lack of transparency can create uncertainty for clinicians who must rely on AI outputs when making decisions that affect patient care. Researchers are addressing this by developing explainable AI models that highlight which image features contributed to a particular result.
Integration into clinical practice also requires robust regulatory approval, interoperability with existing hospital systems, and ongoing training for healthcare professionals. Radiologists must be confident in understanding the strengths and limitations of AI tools to use them effectively. Rather than replacing radiologists, AI is best viewed as an enhancement that augments their expertise.
Ethical Considerations and Data Governance
The use of AI in radiology also raises ethical questions related to patient privacy, consent, and data security. Medical imaging data often contains identifiable information, so its use in algorithm training must comply with data protection regulations such as the UK GDPR. Secure anonymisation and encryption are essential to ensure patient confidentiality.
There is also a need for transparency in how AI systems are developed and validated. Patients should be informed when AI tools are used in their care, and clinicians should understand the limits of algorithmic recommendations. Maintaining trust among patients, healthcare providers, and technology developers is critical to the widespread acceptance of AI in medicine.
The Future of AI-Powered Radiology
As technology continues to evolve, the role of AI in radiology will expand further. The combination of imaging data with genomic, clinical, and lifestyle information will lead to truly personalised health insights. Cloud-based AI platforms are already enabling remote analysis, allowing hospitals with limited radiology expertise to access high-quality diagnostic support.
Future AI systems are expected to operate in real time, integrating data from multiple imaging modalities and providing instant feedback to clinicians. For example, during surgery or interventional procedures, AI could guide instrument placement using live imaging data, enhancing precision and safety.
In research, AI will continue to accelerate discoveries by identifying imaging biomarkers associated with disease mechanisms or therapeutic response. These advances will not only improve diagnostics but also drive innovation in drug development and clinical trials.
Conclusion
AI-powered radiology represents a transformative shift in medical imaging and early disease detection. By combining computational intelligence with human expertise, healthcare is moving towards a model that is proactive rather than reactive, precise rather than generalised, and preventive rather than purely diagnostic.
From identifying microscopic cancerous changes to predicting cardiovascular risk and monitoring neurological disorders, AI is redefining the boundaries of what radiology can achieve. While challenges remain in data quality, ethics, and implementation, the progress made so far demonstrates the immense promise of this technology.
Ultimately, AI will not replace radiologists but empower them—enhancing their accuracy, reducing workload, and enabling earlier, more effective interventions that can save lives. In the coming years, as AI continues to mature, its integration into clinical radiology will no longer be an option but an essential part of delivering high-quality, patient-centred care.
Disclaimer
The information presented in this article, AI-Powered Radiology to Detect Early Disease, is provided for educational and informational purposes only. It does not constitute medical advice, diagnosis, or treatment and should not be used as a substitute for consultation with qualified healthcare professionals. Readers are advised to seek medical guidance regarding any specific health concerns or conditions.
While every effort has been made to ensure the accuracy and reliability of the content at the time of publication, Open MedScience makes no representations or warranties, express or implied, regarding the completeness, accuracy, or applicability of the information contained herein. The use of artificial intelligence in radiology and healthcare remains an evolving field, and research findings, technologies, and regulatory standards may change over time.
Open MedScience accepts no responsibility or liability for any loss, injury, or damages arising directly or indirectly from the use or reliance upon the material provided in this article. The opinions expressed are those of the author and do not necessarily reflect the views of Open MedScience or its affiliates.
home » blog » radiology »