Nuclear medicine stands as a revolutionary intersection between radiology and specialised medical fields, notably neurology, cardiology, and oncology. It employs radioactive substances to diagnose and treat various conditions, offering unique insights that conventional methods might miss. This article outlines the profound impact of nuclear medicine within these three critical areas, highlighting its diagnostic precision, therapeutic benefits, and the future direction of this cutting-edge domain.
Introduction to Nuclear Medicine
Nuclear medicine emerges as a cutting-edge field within the medical domain, offering a unique approach to diagnosing and treating various diseases. This speciality is distinguished by its use of radiopharmaceuticals—small amounts of radioactive substances—to explore the body’s internal processes in real-time. Unlike traditional diagnostic methods that focus solely on anatomical images, nuclear medicine techniques provide valuable functional and molecular insights. This capability allows clinicians to observe how the body is functioning, identify diseases at their onset, and enable more effective, tailored treatments.
At the core of nuclear medicine is the principle of radiopharmacy, which involves using radiopharmaceuticals specifically designed to target specific processes within the body. These substances emit gamma rays that can be detected by special types of cameras, such as the gamma camera, PET (Positron Emission Tomography) scanner, or SPECT (Single Photon Emission Computed Tomography) scanner. The images produced from these scans offer high-resolution details about the biological processes, including the presence and spread of diseases, blood flow to tissues, and the functioning of various organs.
The applications of nuclear medicine span a wide range of medical fields, with significant contributions to neurology, cardiology, and oncology. In neurology, nuclear medicine techniques such as PET scans are instrumental in diagnosing conditions like Alzheimer’s disease, Parkinson’s disease, and epilepsy. By highlighting changes in brain activity or the accumulation of specific proteins, these scans can detect neurological disorders much earlier than traditional methods, facilitating early intervention and management.
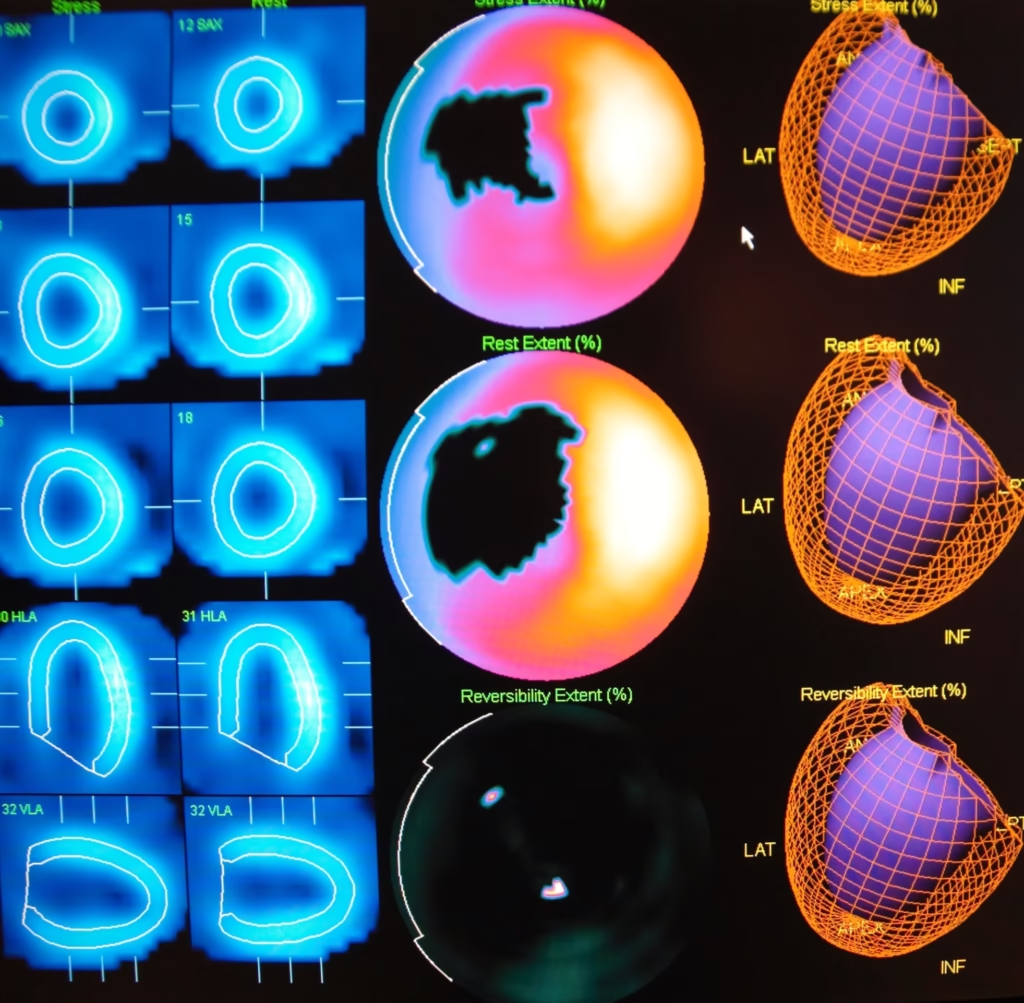
Nuclear medicine plays a pivotal role in diagnosing and assessing heart diseases in cardiology. Techniques like myocardial perfusion imaging help detect coronary artery disease by showing areas of the heart that may have reduced blood flow. Cardiac SPECT and PET scans can also evaluate the heart’s function, including its ability to pump blood effectively, providing crucial information for diagnosing conditions like heart failure.
Oncology is another area where nuclear medicine has made a profound impact. PET scans, often combined with CT or MRI scans, offer comprehensive insights into the presence, location, and spread of cancers throughout the body. This precision in imaging enables oncologists to tailor treatment plans specifically to the patient’s needs, improving outcomes. Moreover, nuclear medicine offers therapeutic applications, such as targeted radionuclide therapy, where radioactive substances are used to treat cancer, targeting malignant cells while sparing healthy tissue.
The future of nuclear medicine is bright, with ongoing advancements in technology and the development of new radiopharmaceuticals enhancing its potential. The field is moving towards more personalised medicine approaches, where treatments are customised based on the individual’s specific disease characteristics and responses. Research into novel imaging agents and therapeutic radiopharmaceuticals continues to expand the scope of nuclear medicine, promising to improve diagnostic accuracy, treatment efficacy, and patient outcomes.
Nuclear medicine represents a significant advancement in medical diagnostics and treatment, offering a deeper understanding of disease processes. By providing detailed functional and molecular information, it enables early detection, accurate diagnosis, and personalised treatment strategies, particularly in the areas of neurology, cardiology, and oncology. As this field continues to evolve, it holds the promise of revolutionising patient care and advancing the frontiers of medical science.
Nuclear Neurology: Mapping the Mind
Nuclear neurology represents a transformative approach to the understanding and management of neurological disorders, leveraging the power of radiopharmaceuticals to illuminate the complexities of brain function. This specialised branch of medicine has become indispensable in the early detection and treatment of conditions such as Alzheimer’s disease, Parkinson’s disease, and epilepsy, offering insights into the brain’s workings that were previously inaccessible.
At the heart of nuclear neurology are PET (Positron Emission Tomography) and SPECT (Single Photon Emission Computed Tomography) scans, sophisticated imaging techniques that enable clinicians to observe cerebral functions and detect abnormalities at a molecular level. These methods rely on the administration of radiopharmaceuticals, substances that emit radiation. When introduced into the body, these substances accumulate in specific brain areas, allowing for detailed neural activity and pathology imaging.
Alzheimer’s Disease
Alzheimer’s disease, a leading cause of dementia, poses significant diagnostic challenges, particularly in its early stages. Nuclear neurology, through the use of PET scans, offers a revolutionary diagnostic tool. PET imaging can identify the buildup of amyloid plaques, a key pathological feature of Alzheimer’s, well before clinical symptoms manifest. This early detection is crucial, as it opens the door to interventions that may delay the progression of the disease, offering patients a better quality of life for a more extended period. Furthermore, ongoing research into tau protein imaging promises even greater specificity in diagnosing various stages of Alzheimer’s, potentially leading to more tailored and effective treatment strategies.
Parkinson’s Disease
Parkinson’s disease is characterised by the degeneration of dopamine-producing neurons in the brain, leading to tremors, stiffness, and a host of movement-related issues. Diagnosing Parkinson’s can be challenging, given the overlap of its symptoms with other neurodegenerative disorders. DAT scans, a form of SPECT imaging, have emerged as a critical tool in distinguishing Parkinson’s from similar conditions. By measuring the concentration of dopamine transporters, these scans provide conclusive evidence of dopamine deficiency, allowing for a more accurate diagnosis and the implementation of targeted therapies that can significantly improve patient outcomes.
Epilepsy
Epilepsy, a disorder marked by recurrent seizures, can be particularly resistant to drug treatment. For patients with drug-resistant epilepsy, surgical intervention may offer relief, but pinpointing the exact origin of seizures within the brain is essential for successful surgery. SPECT scans, used in conjunction with video EEG monitoring, can accurately localise seizure foci, guiding surgeons in removing the precise area of the brain responsible for seizure activity. This targeted approach has profoundly improved surgical outcomes, reducing seizure frequency and, in some cases, achieving complete seizure freedom for patients.
Nuclear neurology has contributed to understanding and treating neurological disorders, representing a significant leap forward in medicine. Providing a window into the brain’s molecular processes enables the early detection of disease, facilitates precise diagnoses, and guides targeted treatment strategies. As research advances and new radiopharmaceuticals are developed, the potential of nuclear neurology to unveil the intricacies of the brain and combat neurological diseases will only continue to grow. This evolving field offers hope to those affected by debilitating neurological conditions and underscores the importance of innovative approaches in unravelling the mysteries of the human mind.
Nuclear Cardiology: A Heartfelt Revolution
Nuclear cardiology stands at the forefront of a revolution in diagnosing and managing heart disease, offering a deeper understanding of heart function, blood flow, and the detection of diseased tissue. This specialised field utilises radiopharmaceuticals to non-invasively assess myocardial perfusion, ventricular function, and the integrity of the heart’s electrical conduction system. Through techniques such as myocardial perfusion imaging (MPI), cardiac function assessment, and nuclear stress tests, nuclear cardiology provides critical insights that guide patient care, from diagnosis through to treatment and follow-up.
Coronary Artery Disease (CAD)
Coronary artery disease, the leading cause of death globally, involves the narrowing or blockage of coronary arteries, leading to a reduction in blood flow to the heart muscle. Myocardial perfusion imaging (MPI) has become an essential tool in nuclear cardiology for diagnosing CAD. MPI assesses blood flow to the heart muscle at rest and during stress, identifying areas with inadequate perfusion. This technique relies on the administration of radiopharmaceuticals, which highlight blood flow discrepancies in the heart tissue. MPI not only aids in diagnosing CAD but also provides valuable information on the severity and extent of the disease, guiding treatment decisions such as the need for angioplasty, stenting, or coronary artery bypass surgery.
Heart Failure
Heart failure, a condition where the heart cannot pump adequately to meet the body’s needs, affects millions worldwide. Nuclear medicine plays a pivotal role in diagnosing heart failure by evaluating cardiac function, particularly ejection fraction (EF) and ventricular dynamics. EF, the percentage of blood ejected from the heart during each beat, is a critical parameter measured using radionuclide ventriculography or gated SPECT imaging. These techniques offer precise, reproducible assessments of heart function, enabling clinicians to classify heart failure, monitor disease progression, and adjust treatments accordingly. By accurately measuring cardiac function, nuclear cardiology helps in tailoring therapies, including medications, device implantation, or surgical interventions, improving patient outcomes.
Cardiac Stress Tests
Stress testing is fundamental to diagnosing coronary artery disease and assessing how the heart functions under physical exertion. Nuclear stress tests enhance the accuracy of these evaluations by combining exercise or pharmacological stress with radiopharmaceutical imaging. This approach allows for the direct visualisation of blood flow to the heart muscle during stress, identifying areas at risk of ischemia (reduced blood flow). Unlike conventional stress tests, nuclear stress tests can detect subtle abnormalities, offering a more sensitive and specific assessment of coronary artery disease. The information garnered from these tests is crucial for guiding treatment strategies, such as recommending lifestyle changes, prescribing medications, or proceeding with interventional procedures.
Nuclear cardiology represents a significant advancement in the field of cardiovascular medicine, providing clinicians with powerful tools to diagnose and manage heart disease with unprecedented precision. The ability to visualise heart function and blood flow at the molecular level has revolutionised patient care, enabling earlier detection, more accurate diagnosis, and personalised treatment plans. As technology evolves and new radiopharmaceuticals are developed, nuclear cardiology will continue to play a vital role in combating heart disease and improving the quality of life for patients around the world. This heartfelt revolution signifies progress in medical science and offers hope to those affected by cardiovascular diseases, marking a new era in heart health management.
Nuclear Oncology: Lighting the Way in Cancer Care
Nuclear oncology represents a pioneering field within cancer care, employing radiopharmaceuticals to diagnose, treat, and palliate cancer with unprecedented precision. This innovative approach combines the diagnostic clarity of nuclear imaging with the therapeutic potential of targeted radiation, offering hope to patients and reshaping oncological practice. Nuclear oncology is lighting the way towards more effective, personalised cancer care through techniques such as PET/CT scans, targeted radionuclide therapy, and radiopharmaceuticals for pain palliation.
Cancer Diagnosis and Staging
The accurate diagnosis and staging of cancer are pivotal for effective treatment planning. PET scans, particularly when combined with CT (PET/CT), have revolutionised oncological diagnostics. These scans allow for the detailed visualisation of metabolic activity within the body, enabling the detection of cancerous cells that other imaging techniques might miss. PET/CT is invaluable in determining the precise location and extent of cancer, providing essential information for staging. This level of detail is crucial for developing an effective treatment strategy, as it helps in understanding the aggressiveness of the cancer, predicting patient outcomes, and planning surgical interventions or radiation therapy with greater accuracy.
Targeted Radionuclide Therapy
One of the most exciting advances in nuclear oncology is the development of targeted radionuclide therapy, such as Peptide Receptor Radionuclide Therapy (PRRT). This treatment involves attaching a radioactive isotope to a molecule that specifically targets cancer cells, sparing surrounding healthy tissue. PRRT is particularly effective for treating certain types of neuroendocrine tumours, delivering high doses of radiation directly to the cancer cells and significantly reducing the tumour burden. The specificity of this approach minimises side effects compared to traditional chemotherapy, representing a significant leap forward in cancer treatment. Targeted radionuclide therapy exemplifies the move towards more personalised, precision medicine in oncology, offering patients therapies tailored to their specific disease profile.
Pain Palliation
For many patients with advanced cancer, particularly those with bone metastases, pain management is a critical concern. Radiopharmaceuticals provide significant relief in such cases, targeting the areas of bone affected by metastatic cancer cells and delivering localised radiation therapy. This method can significantly reduce pain and improve the quality of life for patients with advanced cancer, often when other pain management strategies have failed. The ability to alleviate suffering in this way is one of the most compassionate applications of nuclear oncology, demonstrating the field’s broader benefits beyond diagnosis and treatment.
Nuclear oncology is at the forefront of the fight against cancer, offering tools that improve the precision of diagnosis, the effectiveness of treatment, and the management of cancer-related pain. As research progresses and new radiopharmaceuticals and targeted therapies are developed, the potential for even more personalised and effective treatment strategies grows. This progress promises to extend life and improve the quality of life for cancer patients, showcasing the profound impact of nuclear oncology in transforming cancer care. With each advancement, nuclear oncology continues to illuminate the path towards a future where cancer treatment is more targeted, less invasive, and more attuned to the needs and conditions of individual patients.
The Future of Nuclear Medicine
The future of nuclear medicine is on the brink of a transformative era fueled by rapid advancements in radiopharmaceuticals and imaging technologies. This field bridges the gap between advanced imaging and therapeutic intervention and is poised to redefine personalised medicine. By harnessing the power of novel tracers and therapeutic agents, nuclear medicine is evolving to offer more precise, tailored treatments that align closely with individual patient profiles and the unique characteristics of their diseases.
Advancements in Radiopharmaceuticals
The development of new radiopharmaceuticals is at the heart of the future of nuclear medicine. These compounds, labelled with radioactive isotopes, are designed to target specific cellular processes or disease markers. Innovations in radiopharmaceuticals are improving the sensitivity and specificity of diagnostic imaging and expanding the therapeutic applications of nuclear medicine. For example, targeted radionuclide therapy (TRT) represents a significant advancement, promising to treat cancer with unprecedented precision. These therapies reduce side effects and improve patient outcomes by targeting cancer cells while sparing surrounding healthy tissues. As researchers continue to discover and refine these targeted agents, the potential for treating a wider range of conditions grows, including neurodegenerative diseases, cardiovascular conditions, and various forms of cancer.
Enhancements in Imaging Technologies
Parallel to the advancements in radiopharmaceuticals are the innovations in imaging technologies. Modern PET, SPECT, and hybrid imaging systems, such as PET/MRI, are pushing the boundaries of resolution, sensitivity, and speed. These technologies allow for earlier disease detection, more accurate staging, and better monitoring of treatment response. Furthermore, the integration of artificial intelligence and machine learning algorithms is revolutionising image analysis, enabling more precise interpretation and quantification of nuclear medicine images. This evolution in imaging technology improves diagnostic accuracy and facilitates the development of more effective, individualised treatment plans.
The Growth of Personalised Medicine
Perhaps the most significant impact of these advancements is the acceleration of personalised medicine. Nuclear medicine is at the forefront of developing personalised treatment strategies by combining detailed molecular and functional insights with genetic information. This approach ensures that treatments are specifically tailored to the genetic makeup of the patient’s disease, maximising efficacy while minimising adverse effects. Personalised medicine represents a shift from a ‘one size fits all’ approach to a more nuanced, patient-centred model of care, promising better outcomes and improved quality of life for patients.
Conclusion
Nuclear medicine stands at the intersection of innovation and personalised care, playing a pivotal role in the fields of neurology, cardiology, and oncology. The advancements in radiopharmaceuticals and imaging technologies are not only enhancing the precision and efficacy of this field but are also paving the way for a new era of medical diagnostics and therapy. As these technologies continue to evolve, the scope and impact of nuclear medicine will expand, offering more detailed insights into disease mechanisms and progression. This evolution heralds a future where early diagnosis, informed decision-making, and targeted treatment strategies become the norm, transforming patient care and opening new horizons in the fight against disease. With its promise of personalised medicine, nuclear medicine is poised to revolutionise healthcare, offering hope and improved outcomes for patients worldwide.
Disclaimer
The information provided in this article is intended for general informational and educational purposes only. Open Medscience does not provide medical, diagnostic, or therapeutic advice or services. The content herein is not a substitute for professional medical advice, diagnosis, or treatment. Readers should always seek the guidance of qualified healthcare professionals with any questions regarding a medical condition or treatment plan.
While every effort has been made to ensure the accuracy and reliability of the information at the time of publication, Open Medscience makes no representations or warranties, express or implied, about the completeness, accuracy, suitability, or applicability of any content contained in this article. Use of the information is at the reader’s own risk.
References to specific technologies, medical procedures, or treatments do not constitute an endorsement or recommendation by Open Medscience. The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of any affiliated institutions or organisations.
By reading this article, you agree to hold Open Medscience, its authors, and its affiliates harmless from any liability arising from the use or misuse of the content provided.
You are here: home » diagnostic medical imaging blog »