Summary: Radiotheranostics is a rapidly evolving area of precision medicine that integrates molecular imaging and targeted radionuclide therapy using the same or similar radiopharmaceutical compounds. By confirming the presence of disease-specific molecular targets through diagnostic scans before delivering a therapeutic dose, radiotheranostics allows clinicians to visualise and treat disease with remarkable accuracy. This approach is already transforming the management of advanced prostate cancer and neuroendocrine tumours and is being actively explored for other malignancies and non-oncological conditions. Despite challenges in isotope supply, infrastructure, and cost, research and global collaboration are driving the expansion of radiotheranostics into mainstream clinical practice.
Keywords: Radiotheranostics, Molecular Imaging, Radionuclide Therapy, Personalised Medicine, Prostate Cancer, Neuroendocrine Tumours.
How Radiotheranostics Works
Radiotheranostics has emerged as one of the most critical developments in precision medicine, offering a method of diagnosis and therapy that is closely intertwined. The approach relies on using a single molecular targeting agent, or two closely related agents, labelled with either an imaging isotope or a therapeutic isotope. This allows clinicians to first map the distribution of disease and then deliver radiation precisely to those areas. By linking nuclear medicine imaging with targeted therapy, radiotheranostics has brought new levels of accuracy, safety, and personalisation to patient care.
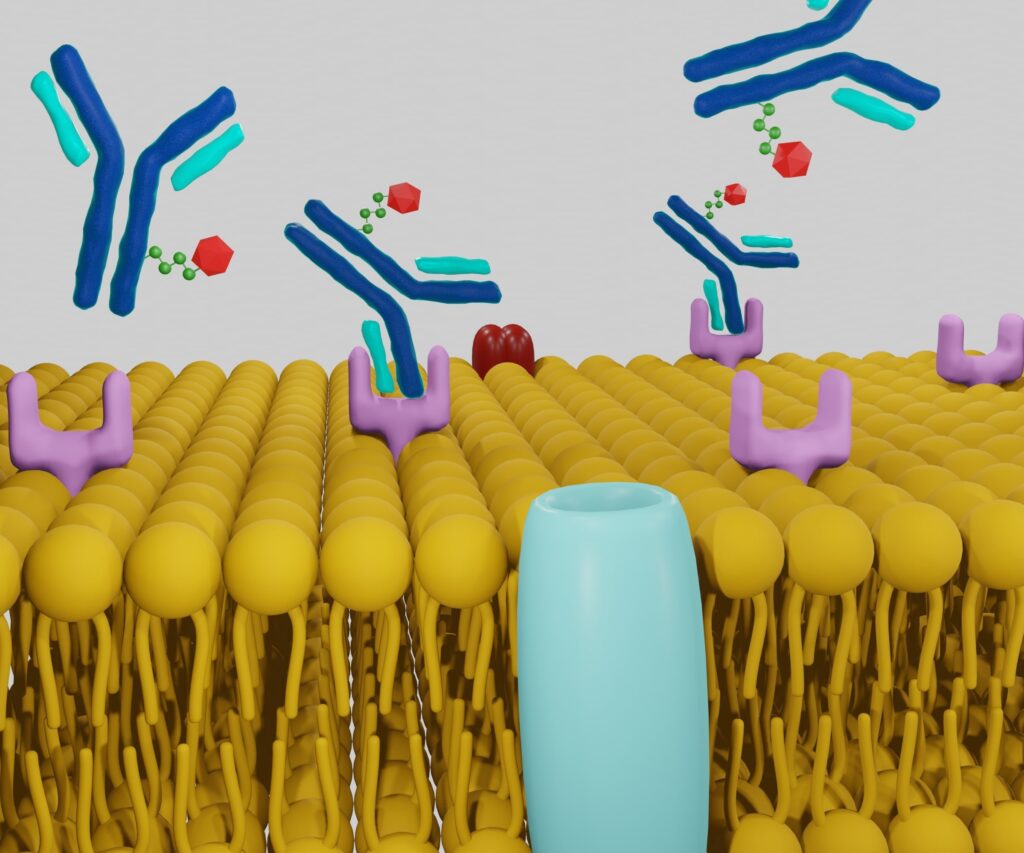
The process begins with the development of a radiopharmaceutical that can bind to a specific molecular marker present on diseased cells. These markers are often proteins or receptors expressed at high levels on cancer cells but not on normal cells. A targeting molecule, such as a peptide or antibody fragment, is linked to a chelating agent that can hold a radioactive isotope. For diagnostic imaging, isotopes like gallium-68 or technetium-99m are used, enabling PET or SPECT scans. For therapy, isotopes such as lutetium-177 or actinium-225 are employed, delivering cytotoxic radiation directly to the tumour.
In practice, the patient undergoes a diagnostic scan with the targeting agent labelled with an imaging isotope. This confirms whether the target is sufficiently expressed and accessible. If the scan shows positive uptake, the therapeutic stage follows, using the same or a similar compound labelled with a therapeutic isotope. This ensures that the treatment is delivered exactly where it is needed, while sparing most surrounding healthy tissue. The predictability of treatment distribution is one of the core strengths of radiotheranostics.
Established Clinical Applications
Radiotheranostics has already become a valuable part of clinical care for specific cancers. In prostate cancer, prostate-specific membrane antigen (PSMA) is a well-characterised target that is overexpressed in many advanced cases. Gallium-68 PSMA PET/CT provides sensitive imaging of metastatic lesions. If these lesions demonstrate uptake, lutetium-177 PSMA therapy can be administered to selectively irradiate cancer cells throughout the body. This approach has been shown to improve disease control and alleviate symptoms in patients with advanced, treatment-resistant disease.
In neuroendocrine tumours, overexpression of somatostatin receptors is common. Gallium-68 DOTATATE PET/CT imaging can detect these receptors with high sensitivity, while lutetium-177 DOTATATE therapy targets them directly. The NETTER-1 trial demonstrated that this therapy significantly improved progression-free survival compared to high-dose somatostatin analogue therapy alone, marking a milestone in the treatment of this rare cancer type.
Expanding Therapeutic Horizons
Beyond its established indications, radiotheranostics is now being investigated in a wide range of malignancies. In breast cancer, HER2-targeted radiopharmaceuticals are being developed to image and treat HER2-positive tumours, potentially providing a new option for patients with resistant disease. Glioblastoma, one of the most aggressive brain cancers, is also under study for targeted radionuclide therapy. Haematological cancers, including certain lymphomas, may benefit from radiolabelled antibodies targeting cell-surface antigens.
Interest is also growing in applying radiotheranostics to non-cancerous conditions. Inflammatory diseases, cardiovascular disorders such as atherosclerosis, and some infectious diseases could theoretically be targeted if suitable molecular markers are identified. This would represent a major expansion of the field beyond oncology.
Benefits for Patients and Clinicians
The primary advantage of radiotheranostics lies in its ability to personalise treatment. Diagnostic imaging ensures that only patients with confirmed target expression receive therapy, avoiding unnecessary radiation exposure. This selectivity reduces systemic side effects and improves the likelihood of treatment success.
For patients, the precision of radiotheranostics means that tumours can be targeted even in locations that are challenging for surgery or external beam radiotherapy. Many report improved quality of life compared to traditional chemotherapy, with fewer and less severe side effects. For clinicians, the combination of visual confirmation and targeted treatment enables better patient selection, more accurate dosing, and the potential to adapt therapy based on imaging feedback.
Current Challenges
Despite its promise, radiotheranostics faces several obstacles to widespread adoption. The production of therapeutic isotopes, such as lutetium-177, requires specialised nuclear reactors, while alpha emitters like actinium-225 are even more challenging to produce at scale. Supply chain limitations create disparities in access between countries and even within regions.
Infrastructure is another challenge. Radiotheranostics requires advanced imaging facilities, licensed radiopharmacies, and highly trained multidisciplinary teams. Establishing and maintaining this capability demands substantial investment. Financial considerations also play a role, as the cost of isotope production, imaging, and therapy delivery can be high. Reimbursement policies in some healthcare systems are inconsistent, which may deter the adoption of new practices.
Safety remains a focus of research. While the short- and medium-term safety profiles of most radiotheranostic therapies are favourable, long-term monitoring is essential, particularly for alpha-emitting therapies that deliver high-energy radiation over very short distances.
Advances in Research and Development
Research is actively addressing these challenges. New isotope production facilities are being commissioned to expand supply. Alpha emitters are being investigated for their potential to kill cancer cells more efficiently while sparing surrounding tissue. Novel molecular targets are being identified through advances in proteomics and genomics, potentially allowing radiotheranostics to be applied to a broader range of diseases.
In parallel, improvements in dosimetry and treatment planning are enhancing patient-specific care. Artificial intelligence is being used to predict therapy response, optimise dosing, and assist in treatment decision-making. There is also growing interest in combining radiotheranostics with immunotherapies, targeted drugs, and external beam radiotherapy to create synergistic effects.
The Global Outlook
The pace of adoption varies internationally. In the United Kingdom, the NHS has integrated lutetium-177 DOTATATE into clinical practice for neuroendocrine tumours, setting a precedent for other radiotheranostic therapies. Prostate cancer applications are following suit, supported by regulatory approvals and clinical evidence. In Europe and Australia, access is expanding through coordinated isotope production and distribution networks. The United States has approved certain radiotheranostic agents, though access may depend on institutional capacity and funding.
International collaboration is likely to be essential for long-term success, not only in ensuring isotope supply but also in standardising protocols, sharing clinical data, and training the next generation of specialists.
Conclusion
Radiotheranostics represents a paradigm shift in how disease is diagnosed and treated. Uniting imaging and therapy in a single patient-specific pathway offers a level of precision that conventional treatments cannot match. For cancers such as advanced prostate cancer and neuroendocrine tumours, it is already delivering measurable improvements in outcomes and quality of life. As research expands its applications, radiotheranostics may well become a cornerstone of personalised medicine in oncology and beyond.
Take-Home Message
Radiotheranostics combines targeted molecular imaging and radionuclide therapy to diagnose and treat disease with exceptional precision. Already transforming the management of prostate cancer and neuroendocrine tumours, it is poised for broader application across oncology and potentially other medical fields. While challenges in isotope supply, infrastructure, and cost remain, advances in research and international collaboration are steadily moving radiotheranostics towards becoming a standard of care.
Disclaimer
The content provided in Radiotheranostics: The Dual Power of Diagnosis and Therapy in Modern Medicine by Open MedScience is intended for informational and educational purposes only. It does not constitute medical advice, diagnosis, or treatment and should not be used as a substitute for professional medical guidance. Readers should consult a qualified healthcare professional before making decisions about diagnosis, treatment, or the use of any medical technologies described. While every effort has been made to ensure the accuracy and currency of the information at the time of publication, Open MedScience makes no warranties or representations regarding completeness, reliability, or applicability to individual circumstances. References to specific medical procedures, technologies, or products do not imply endorsement. The views expressed are those of the authors and do not necessarily reflect those of any affiliated institutions or organisations.