Medical imaging plays a vital role in the early detection of breast cancer including those with BRCA1 or BRCA2 mutations.
Overview of imaging techniques in breast cancer
In 2016-17, a breast cancer screening programme was carried out in England and the following facts were reported: 2.2 million over the age of 45 were screened (34% increase from the previous decade); 71.1% of women took up the breast imaging invitation; 18,402 women aged over 45 had cancer and correlated to 8.4 cases per 1,000 women screened.
In about 5 to 10% of patients, the origin of their breast cancer was the result of gene mutations. In some cases, the mutant forms of the breast cancer gene 1 (BRCA1) and breast cancer gene 2 (BRCA2) have shown to play a role in the initiation of about 10% of all breast cancers. Therefore, women who possess faulty BRCA1 or BRCA2 allele (a variant form of a gene) are at higher risk of developing breast cancer within their lifetime.
It is worth noting that several studies have implicated mutated BRCA1/2 genes in the role of prostate, pancreatic and stomach cancers.
Both BRCA1 and BRCA2 genes are present in all humans and BRCA1 is involved in the repair of DNA breaks that could lead to the formation of a tumour. Also, the BRCA genes in themselves do not cause breast cancer as they have a role in its prevention. Consequently, these genes are known as tumour suppressor genes. The reason that these genes do not work correctly and are involved in breast cancer is because of mutations within them.
Incidentally, about 0.25% of the human population carry mutated BRCA1 or BRCA2 genes. One of the most common cancer-related mutations found in BRCA1 is the 5382insC. This mutation originated from a common European ancestor about 400-500 years ago and is associated with a higher incidence of ovarian cancer (9.4%).
These damaged BRCA genes can no longer be effective at repairing broken DNA and helping to prevent breast cancer. Therefore, people with a BRCA gene mutation are more likely to develop breast cancer and pass a gene mutation down to the next generation.
Women with a BRCA1 or BRCA2 mutation who have overcome breast cancer through a treatment plan may develop secondary cancer known as a recurrence. Cancers involving BRCA1 mutations are more probable, forming aggressive triple-negative breast cancer which is challenging to treat. Triple-negative breast cancer tests negative for oestrogen receptors, progesterone receptors and excess HER2 protein. About 10-20% of breast cancers are triple-negative breast cancers.
Today, medical imaging plays a vital role in the early detection of breast cancer including those with BRCA1 or BRCA2 mutations. The most commonly used breast imaging techniques are positron emission tomography/computed tomography (PET/CT) imaging, ultrasound, magnetic resonance imaging (MRI), thermography and electrical impedance tomography. The objective of these medical imaging modalities is to detect breast cancer at the earliest stage.
Medical imaging modalities
Mammography
This technique is used in the detection of breast cancer and utilises low-dose amplitude X-rays. Screen-film mammography has proved to be the gold standard in breast screening due to its cost-effectiveness and reduction in breast cancer mortality. During mammography screening, two standard views are used and these include the mediolateral oblique (MLO) view and the craniocaudal (CC) view. The MLO view compresses the breast along a plane of approximately 45 degrees extending from the upper inner quadrant to the lower outer quadrant. In this configuration, the X-ray tube is rotated parallel to the pectoralis muscle fibres and allows for maximum breast tissue in the MLO view. The CC view positions the breast directly on top of the X-ray cassette holder with the X-ray tube positioned for superior and inferior imaging.
The cancerous masses and calcium deposits appear bright in the mammogram and this technique has the ability to detect ductal carcinoma in situ (DCIS). It is vital to detect breast cancer at the earliest stage to prevent the formation of lesions from becoming evident. The generation of a 3-D mammogram will have more significant screening potential in spotting breast lesions. A study of 7300 women from the ages of 48 to 71 received a standard mammogram including both a combination of standard and 3-D imaging. It was found that a total of 59 breast cancers were detected. However, 39 were found by both standard mammogram alone and the standard plus 3-D compared to combination mammography which found an additional 20 cancers. In September 2017, the Tomosynthesis Mammographic Imaging Screening Trial (TMIST) was opened to healthy women in order to compare and contrast the tomosynthesis (3-D mammogram) and the conventional 2-D mammogram.
Digital mammography
This technology uses a single or multiple detector system. The electronic image of the X-rays transmitted through the breast can be displayed, stored and communicated. Digital mammography is now a standard tool for breast cancer imaging and is replacing screen-film mammography as the preferred tool for screening.
Digital breast tomosynthesis – DBT
Breast tomosynthesis is an advanced form of mammography. This breast imaging uses low-dose X-rays to detect cancer early when it is at its most treatable. The technique DBT continues to expand in the clinical setting and produces a more effective mammogram based on observed increases in specificity and breast cancer detection compared with digital mammography (DM) alone. DBT will help to address the limitation caused by overlapping structures by acquiring a series of low-dose projection images. Computer reconstruction allows the radiologist to examine 1 mm single-section images for a particular volumetric set. This technique has shown improved sensitivity and specificity compared with digital mammography, especially in cases of noncalcified breast cancer with an overall improvement of cancer visibility.
Ultrasound imaging
This modality works by directing high-frequency sound waves via a transducer into the breast tissues. This results in the detection of the reflected sound waves and produces 2-D images in real-time. The ultrasound approach is used to detect the location of the breast lesions.
Automated breast ultrasonography – ABUS
The first line of examination in the detection of breast lesions is the application of breast ultrasonography. The use of handheld ultrasonography devices is very dependent on the healthcare professional and require a significant amount of time for the radiologist to examine the whole breast. However, the ABUS device provides improvements in higher reproducibility and less operator dependence compared to handheld ultrasonography. The ABUS system provides both coronal and a large field of view. Several studies have indicated that ABUS is a useful screening tool for breast cancer in women with dense breast tissue.
Elastography
This test can be carried out in conjunction with an ultrasound examination. Elastography works using the concept that breast cancers appear to be more solid compared to the surrounding breast tissues. During the elastography process, the breast is slightly compressed, and ultrasound is targeted to a particular area to see how firm it is. This test will help to decide if the solid is likely to be cancer or a benign tumour.
Breast thermography
The concept behind this imaging technique makes use of the fact that cancerous tissues have a higher metabolic rate which can lead to the formation of new blood vessels to supply vital nutrients in order to grow the cancerous mass. This results in an increase in the localised temperature of the cancerous breast tissue compared to the temperature of the surrounding healthy tissues. Furthermore, breast thermograms can detect breast cancer accurately and can be used as a screening tool to diagnose breast cancer at least ten years in advance.
Magnetic resonance imaging – MRI
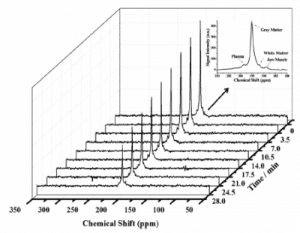
The Indomitable was the first MRI full-body scanner invented by Raymond Damadian for human body imaging in 1977. This non-invasive technique makes use of the physical properties of the hydrogen nucleus (a single proton) to produce images. The human body is abundant in water and fat and enables the magnetic ‘spin’ property of the hydrogen nucleus to generate internal images. This procedure involves placing the patient on a horizontal moveable bed followed by transportation into the magnetic field. Once inside the tunnel, a radio frequency wave is applied to create high contrast images of the breast. Several techniques stem from MRI and include the injection of a contrast agent into the patient to produce dynamic contrast enhanced-MRI (DCE-MRI) images. The advantage of this technique is that it is more sensitive than mammography and is used to investigate the vascular changes associated with neoangiogenesis. Also, MRI is used to assess tumour response to treatment plans and in the early detection of breast cancer. In addition, advanced MRI scanners using 3 Tesla magnets have demonstrated that MRI can achieve a higher spatial and temporal resolution to produce an improved signal to noise ratio and consequently improve survival rates.
Magnetic resonance elastography – MRE
This non-invasive medical imaging technique is based on imaging the propagation of transmission of shear waves. During this process, measurements are taken regarding the stiffness of soft tissue. Consequently, the stiffness of diseased tissue is more than that of healthy tissue in the surrounding area. MRE works by applying acoustic waves with a frequency of 100 Hz to 1 kHz and adjusting motion-sensitive phase-contrast MRI sequences. Furthermore, this gives rise to the propagation of shear waves as a function of the shear modulus of the tissue. The images are the result of shear wave propagation with variable wavelengths and are being used in the detection of breast cancer. Several studies have found that breast cancer tissue is much harder than healthy fibroglandular tissue.
Magnetic resonance mammography – MRM
This technique is capable of distinguishing the physiologic changes of the scar from tumour tissue due to its high sensitivity, specificity and accuracy. For example, the clinical and X-ray mammographic assessment of response to neoadjuvant chemotherapy may be inaccurate because of the replacement of the tumour with scar tissue. Also, MRM is useful in patients with recurrent disease and for the assessment of breast implants because it is more accurate than X-ray mammography and ultrasound. MRM is becoming a valuable tool in the diagnostic uncertainty of breast cancer and will become more prevalent in the clinical setting.
Positron emission tomography – PET
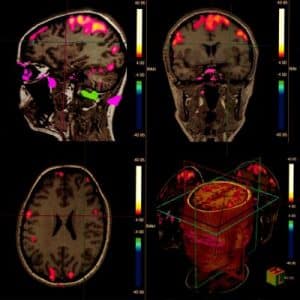
Nuclear medicine procedures and can measure the metabolic activity of cells within the human body to generate 3-D images. The patient receives a radioactive tracer via injection into the bloodstream: the emitted radiation produces a pair of gamma rays which are detected. Malignant tumours will rapidly uptake glucose and provide a contrast between cancerous and healthy cells in PET images. This technique can be used in the investigation of brain and heart function and also in planning cancer treatment.
Single-photon emission computed tomography – SPECT
This imaging technique utilises computed tomography (CT) in conjunction with an injected radioactive tracer into the bloodstream of a patient. When the radioactive tracer is taken up by the cells, the X-rays produced are then detected by gamma cameras and provide an image. SPECT can be used to investigate blood flow to tissues and metabolism in the body. Both SPECT and PET are used to study animal models of breast cancer with direct application to human imaging. Also, MRI and PET can be used to monitor the response of medical treatment – during breast cancer assessment and pre-surgery -known as neoadjuvant chemotherapy.
PET/MR imaging in breast cancer
This is a combination of positron emission tomography (PET) and magnetic resonance imaging. The hybrid scanner combines the metabolic information obtained from PET imaging with the high resolution of MRI to contrast the soft tissue into a single examination of the patient. Furthermore, dynamic contrast-enhanced MRI of the breast provides higher sensitivity in the evaluation of primary breast cancers. However, PET/CT has shown to provide information regarding loco-regional staging in women: especially with locally advanced breast cancer and the response to neoadjuvant chemotherapy. Moreover, PET/MRI has shown to perform just as well as PET/CT imaging in patients with breast cancer, especially during the assessment of metastatic cancer.
Scintimammography, SPECT and PET imaging
These imaging tools are useful in the early detection and staging of breast cancer. A disadvantage of these imaging modalities is the insufficient sensitivity to detect small (less than 1 cm) tumours. Therefore, these imaging techniques cannot replace invasive procedures. However, SMM is a useful technique in the assessment of palpable breast masses in women and PET imaging for the detection and staging of recurrent breast cancer facilitated with the radiotracer [18F]fluorodeoxyglucose. Also, PET imaging can assess the patient’s response to chemotherapy.
The scintimammography imaging technique can visualise lesions of the breast by utilising in vivo injections of radiotracers. The advantage of SMM over mammography is its ability to detect breast cancer in dense breast tissue. Also, mammography can result in a high number of false positives. The radiopharmaceutical technetium-99m tetrofosmin allows improved precision in the diagnosis of women with dense breasts through this scintimammography approach. This technique demonstrated that high-resolution scintimammography of the breasts was able to detect small (<1 cm) nonpalpable lesions. Also, the application of mammography with the scintimammography imaging agent 99mTc-MIBI was able to decrease the number of biopsies by 34% in patients with potential breast cancer.
Positron emission mammography – PEM
Mammography using positron emitters was first proposed in 1994 and has demonstrated to have a higher resolution as PET-CT. The PEM set up uses a pair of gamma radiation detectors placed above and below the breast under slight compression. The radiotracer [18F]fluorodeoxyglucose is injected into the bloodstream of the patient and the resultant coincident of two 511 keV gamma rays, which are emitted 180 degrees from opposite directions and detected by a gamma camera. This high-resolution tomographic technique is a complementary imaging resource in patients with a history of breast cancer with apparent abnormalities in their mammogram.
Optical imaging
This technique makes use of the physical property of near-infrared (NIR) wavelength light which is capable of detecting lesions inside the breast. Diffuse optical imaging is the progression from near-infrared spectroscopy and uses image reconstruction techniques to generate pictures from multiple NIRS measurements. It is primarily used in functional brain imaging and imaging for breast cancer. Diffuse optical imaging uses NIR light to penetrate the breast at wavelengths of 700 to 1000 nm. However, optical mammography uses various wavelengths of light to detect breast lesions. The advantage of diffuse optical imaging is that it is non-invasive and can be used to characterise the properties of dense tissue.
Electrical impedance tomography and electrical impedance scanning
These non-invasive mobile breast screening techniques do not use ionising radiation and work by the body tissues offering resistance to the flow of electric current. Several studies have shown that breast cancer tissue has a lower impedance compared to healthy tissues. The 2-D or 3-D images are reconstructed from a range of impedance values obtained by placing electrodes around the breast surface.
Microwave imaging
Several research groups have studied microwave breast imaging systems that are non-invasive for the early detection of breast cancer. The advantage of this technique is that the breast does not have to be compressed during the imaging process. Also, a microwave breast imaging system will help patients who have dense breast tissue to receive regular breast cancer screening safely and comfortably. Laser infrared thermography assisted by microwaves provides a source of heating the biological tissues in the breast to provide active dynamic thermography (ADT) in mammography.
Radio waves
Imaging systems are being developed that use radio-waves to detect breast cancer. The advantage of this technique is that it does not involve breast compression.
Computed tomography
This imaging technique was introduced in 1972 and made use of X-rays to generate 2-D images (slices) of the human body. A different algorithm is applied to produce more advanced 3D anatomical images, especially in the location of lesions. The disadvantage of CT is the low contrast images and consequently, iodinated agents can be injected into the bloodstream to produce more pronounced images of the tumours. Also, shown that CT perfusion in breast cancer patients can identify and locate enlarged axillary lymph nodes.
Hybrid imaging
This technique involves combining PET and CT imaging and is especially useful in the staging of metastatic cancers. The benefits of this hybrid scanner are that CT can better define the location of the tumour while PET can indicate the metabolic activity of the cancer cells uptake of glucose. Also, automated ultrasound systems can be combined with CT or breast MRI and would be able to assist surgeons in obtaining more accurate biopsies. Furthermore, the combination of digital breast tomosynthesis (DBT) and scintimammography, including 18FDG-PET-MRI where anatomical and functional techniques together have the potential to provide a more accurate assessment of the breast cancer patient.
Photoacoustic computed tomography
The concept behind this new scanner developed by Caltech is to locate tumours within 15 seconds by shining pulses of light into the breast. This scanning technique is called photoacoustic computed tomography (PACT) and primarily works by shining a near-infrared laser pulse into the breast tissue. The mode of action of detection is as the laser light diffuses through the breast the haemoglobin molecules in the red blood cells cause ultrasonic vibrations. These vibrations pass through the tissue and are detected by an array of 512 tiny ultrasonic sensors around the skin of the breast. The data generated from these sensors can create an image of the breast’s internal structures. The advantage of PACT is that it can view structures as tiny as 0.25 mm of a depth of 4 cm. Also, mammograms are unable to provide soft-tissue contrast compared to higher details from PACT images.
Molecular breast imaging -MBI
The two types of MBI include breast-specific gamma imaging (BSGI) which tracks the blood flow during the uptake of the radiotracer sestamibi. The process involves a single 1-D image captured per view and is similar to mammography as it uses a small-field-of-view gamma camera. The second technique involves high-resolution positron emission mammography (PEM), which uses the PET tracer 18F-FDG to track glucose activity. MBI is applied when the mammogram results are questionable. The primary objective of mammography is to obtain information regarding the anatomical nature of the breast, which is in contrast to MBI, which detects cancers via metabolic activity in the breast.
In some cases, BSGI is used to assist mammography by distinguishing between scar tissue and cancer recurrence. In addition, BSGI is used to complement MRI investigations regarding the type of breast cancer involved. Moreover, PEM can be applied in pre-surgical staging and planning, including neoadjuvant chemotherapy response monitoring. The reported study of MBI in its effectiveness in detecting breast cancers is concluded in a group of 1,696 women. These patients had dense breasts and gave negative mammography results when screened using MBI. The study concluded that a total of 13 cancers were detected and 11 were invasive. The cancers ranged in size from 0.6 to 2.4 cm.
Artificial intelligence (AI) systems
The patient’s diagnosis is dependent on who interprets the imaging scans relating to breast cancer. These scans can be very complicated and time-consuming for radiologists. However, to speed up the diagnostic outcome of these scans, AI companies like Google Health and DeepMind have developed AI systems to analyse radiological scans which detect breast cancer. The AI system was able to decrease false positives by 5.7% in women by analysing mammograms for breast cancer. To teach the AI system about reading mammograms, the data was collected from 76,000 scans involving UK and USA women. The collective data was used to evaluate X-rays from 25,000 UK women and 3,000 US women. The scans which indicated that the women had cancer required verification by obtaining a biopsy. This AI system demonstrated that it was more superior to a single radiologist reading the mammograms and did not require any other medical data to base its outcome. Also, AI reduced the false negatives by 9.4% and patients were able to undergo a suitable breast cancer treatment plan.
Conclusion
At present, there is a shortage of senior radiologists in the UK and this is having an adverse effect on cancer patients. Furthermore, the radiologist’s workload of reading and interpreting scans has increased by 30% between 2012 and 2017. Consequently, artificial intelligence (AI) systems in the future will be able to assist in the rapid diagnosis of breast cancer with patients able to receive the correct treatment plan.
Screening programmes involving mammography aim to identify breast cancer before symptoms appear. Hence, facilitating earlier therapy increases a more favourable treatment outcome. The problem of screening programmes is how to interpret the vast data generated from the images. Radiologists must be careful not to give false positives or false negatives regarding the conclusions drawn from the images.
The Google Health AI system was able to show it was better at reading scans than an individual radiologist to locate breast cancer. Clinical data derived from reading mammograms from the US and UK was used to analyse scans. It found that the AI system reduced false positives by 5.7% (US) and 1.2% (UK) compared to false positives being 9.4% (US) and 2.7% (UK).
To further demonstrate the power of the AI system, researchers showed that the AI system was able to outperform six radiologists. These early assessments of the AI system initiated future clinical trials to improve the accuracy and efficiency of breast cancer screening programmes.
However, in the UK, it is a requirement that two radiologists review X-rays, and it was concluded that the AI system did not perform better than the two radiologists combined. AI systems will revolutionise diagnostic medicine by reducing the waiting times increasing patient output leading to improved patient treatment plans.
You are here: home » medical imaging blog »