Summary: Magnets have fascinated humanity for centuries, not just for their mysterious attraction but for their profound impact on various technologies. In the area of medicine, magnets have emerged as indispensable tools, transforming diagnostics, therapeutics, and research methodologies. This article investigates the multifaceted uses of magnets in modern medicine, exploring their applications, benefits, and the innovations that continue to shape healthcare.
Introduction
The allure of magnets extends beyond their ability to attract metals; they have become pivotal in advancing medical science. From the non-invasive imaging techniques that peer inside the human body to innovative therapies that target diseases at the cellular level, magnets are at the forefront of medical innovation.
Before exploring their medical applications, it is essential to understand the basics of magnetism. Magnets produce magnetic fields, invisible forces that can attract ferromagnetic materials like iron, nickel, and cobalt. In medicine, both permanent magnets and electromagnets (which generate a magnetic field when electric current flows through them) are used.
Types of Magnets Used
- Permanent Magnets: Made from materials like neodymium or samarium-cobalt, these magnets retain their magnetism without the need for electricity.
- Electromagnets: Created by passing an electric current through a coil of wire, their magnetic field can be controlled by adjusting the current.
- Superconducting Magnets: Utilised in devices like MRI machines, they require extremely low temperatures to function and produce very strong magnetic fields.
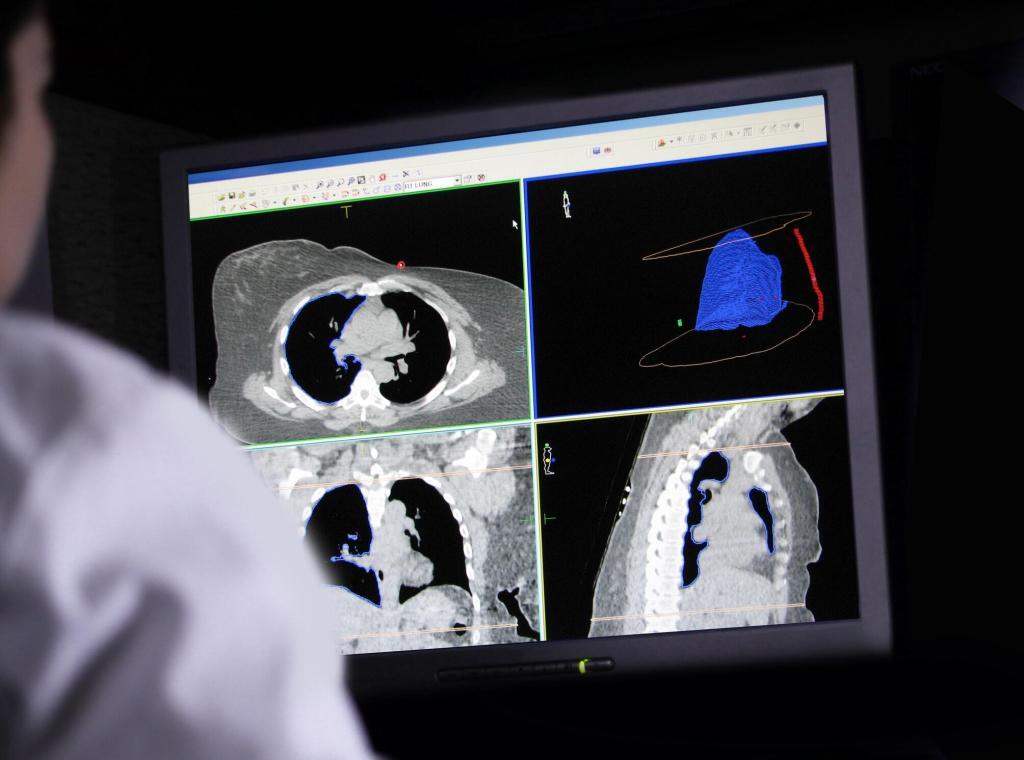
Magnetic Resonance Imaging (MRI)
Perhaps the most well-known medical application of magnets is Magnetic Resonance Imaging (MRI). This non-invasive diagnostic tool has transformed medical imaging, allowing clinicians to obtain detailed images of internal body structures.
How MRI Works
MRI machines use powerful superconducting magnets to generate a strong magnetic field. When a patient is placed inside this field, the hydrogen nuclei in their body align with it. Radiofrequency pulses are then applied, temporarily disrupting this alignment. As the nuclei return to their original state, they emit signals that are detected and converted into detailed images by a computer.
Advantages Over Other Imaging Techniques
- Non-Ionising Radiation: Unlike X-rays or CT scans, MRIs do not use ionising radiation, reducing the risk of harmful exposure.
- High Contrast Images: MRIs provide excellent contrast between different soft tissues, making them ideal for imaging the brain, muscles, and connective tissues.
- Functional Imaging: Techniques like functional MRI (fMRI) can assess brain activity by detecting changes in blood flow.
Magnetic Therapy
The use of magnets for therapeutic purposes dates back centuries. Today, magnetic therapy encompasses various practices, some of which are integrated into mainstream medicine, while others remain alternative treatments.
Historical Context
Ancient civilisations, including the Greeks and Chinese, explored the healing properties of magnets. They believed magnets could influence the body’s energy flow and alleviate ailments.
Contemporary Magnetic Therapies
- Transcranial Magnetic Stimulation (TMS): A non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain, often used to treat depression.
- Pulsed Electromagnetic Field Therapy (PEMF): Uses electromagnetic fields to promote bone healing and reduce pain.
- Static Magnetic Field Therapy: Involves placing static magnets near the body, though scientific evidence supporting its efficacy is limited.
Evidence and Controversies
While treatments like TMS have robust scientific backing, the effectiveness of static magnetic field therapy remains controversial. The placebo effect and lack of rigorous clinical trials contribute to the debate.
Magnetically Controlled Drug Delivery
Advancements in nanotechnology have enabled the development of magnetically controlled drug delivery systems, offering targeted therapy with reduced side effects.
Mechanism
Magnetic nanoparticles are bound to therapeutic agents and injected into the bloodstream. External magnets are then used to guide these particles to specific sites within the body, concentrating the treatment where it is needed most.
Benefits
- Targeted Delivery: Reduces systemic exposure and side effects.
- Controlled Release: Magnetic fields can modulate the release rate of the drug.
- Enhanced Efficacy: Higher local concentrations improve therapeutic outcomes.
Challenges
- Biocompatibility: Ensuring magnetic particles are safe and do not elicit immune responses.
- Controlled Navigation: Precisely guiding particles through complex vascular systems.
Magnetic Surgery and Robotics
Magnets are increasingly used in surgical procedures, enhancing precision and reducing invasiveness.
Magnetic Anchoring and Guidance Systems (MAGS)
MAGS utilise external magnets to control internal surgical instruments without the need for additional incisions. This approach minimises trauma and speeds up recovery.
Robotic Applications
Magnetic fields guide miniature robotic devices inside the body, performing tasks such as biopsies or delivering therapies to hard-to-reach areas.
Future Prospects
Research continues into improving the dexterity and control of magnetically guided surgical tools, potentially revolutionising minimally invasive surgery.
Magnetic Stimulation Therapies
Beyond TMS, other magnetic stimulation therapies are emerging as potential treatments for various conditions.
Repetitive Transcranial Magnetic Stimulation (rTMS)
An extension of TMS, rTMS involves repeated magnetic pulses and is investigated for treating neurological conditions like Parkinson’s disease and stroke rehabilitation.
Deep Brain Stimulation (DBS)
Although DBS primarily uses electrical stimulation via implanted electrodes, research explores the use of magnetic fields to achieve similar effects non-invasively.
Magnetic Materials in Medical Devices
Magnets play a crucial role in the functionality of various medical devices.
Implantable Devices
- Pacemakers and Defibrillators: Use magnets for programming and safety features.
- Magnetic Sphincters: Devices like the LINX system treat gastro-oesophageal reflux disease by reinforcing the lower oesophageal sphincter with magnetic beads.
Biocompatible Materials
Developing magnetic materials that are biocompatible and durable is essential for implantable devices. Innovations focus on materials that minimise corrosion and tissue reaction.
Risks and Safety Considerations
While magnets offer significant benefits, they also pose risks if not properly managed.
Potential Hazards
- Interference with Medical Devices: Strong magnetic fields can disrupt the functioning of pacemakers or insulin pumps.
- Projectile Risk: In MRI environments, ferromagnetic objects can become dangerous projectiles.
- Heating Effects: Magnetic fields can induce currents in conductive materials, causing heating.
Safety Protocols
- Screening: Patients are thoroughly screened for metal implants or devices before MRI scans.
- Training: Medical staff receive training on handling magnets and magnetic equipment safely.
- Regulations: Standards govern the manufacturing and use of magnetic medical devices to ensure safety.
The Future of Magnets in Medicine
The potential applications of magnets in medicine continue to expand, driven by ongoing research and technological advancements.
Nanotechnology and Magnetism
The integration of nanotechnology with magnetism promises breakthroughs in diagnostics and therapeutics, such as:
- Magnetic Hyperthermia: Using magnetic nanoparticles to generate heat and destroy cancer cells.
- Advanced Imaging Techniques: Enhancing contrast agents for more precise imaging.
Personalised Medicine
Magnetically guided therapies could enable personalised treatment plans, targeting diseases at the molecular level.
Challenges Ahead
- Ethical Considerations: Balancing innovation with patient safety and consent.
- Regulatory Hurdles: Ensuring new technologies meet stringent safety standards.
- Interdisciplinary Collaboration: Fostering cooperation between engineers, clinicians, and researchers.
Conclusion
Magnets have transcended their traditional roles, becoming integral to modern medicine’s fabric. From enabling life-saving diagnostics to pioneering new therapeutic avenues, their impact is profound and far-reaching. As technology advances, magnets will undoubtedly continue to play a critical role in shaping the future of healthcare, offering hope for more effective treatments and improved patient outcomes.
Disclaimer
The content of this article is intended for informational and educational purposes only. It does not constitute medical advice, diagnosis, or treatment, and should not be relied upon as such. Readers are advised to consult qualified healthcare professionals regarding any medical conditions or treatments discussed herein. Open Medscience makes no representations or warranties about the accuracy, completeness, or current relevance of the information presented. While efforts have been made to ensure the content is evidence-based, some practices and technologies mentioned may still be under investigation or considered experimental. Open Medscience disclaims any liability for any loss or damage arising directly or indirectly from the use of or reliance on the information contained in this article.