Radiotheranostics is an innovative approach to cancer treatment that integrates diagnostic imaging with targeted radiotherapy. This dual functionality allows for more precise cancer diagnosis, personalised treatment, and improved therapeutic outcomes. By using molecular agents that specifically target cancer cells, radiotheranostics promises to revolutionise oncology, improving patient outcomes and minimising side effects. This article explores the science behind cancer radiotheranostics, its applications, and its future potential in precision medicine.
Introduction to Radiotheranostics
Cancer remains one of the leading causes of mortality worldwide, with millions of new cases diagnosed each year. Traditional treatment methods such as surgery, chemotherapy, and radiotherapy have shown significant success in managing cancer, yet these treatments come with their own set of limitations. Among the most pressing challenges is the ability to target cancer cells specifically without damaging healthy tissues. This is where radiotheranostics comes into play—a field that offers a new frontier in precision cancer treatment.
Radiotheranostics combines diagnostic imaging and therapeutic radiotherapy into a single platform, enabling clinicians to diagnose, treat, and monitor cancer in a more personalised and effective manner. As a result, radiotheranostics holds the potential to transform oncology by offering a more patient-specific approach to cancer care, reducing toxicity, and enhancing therapeutic outcomes.
The Science Behind Radiotheranostics
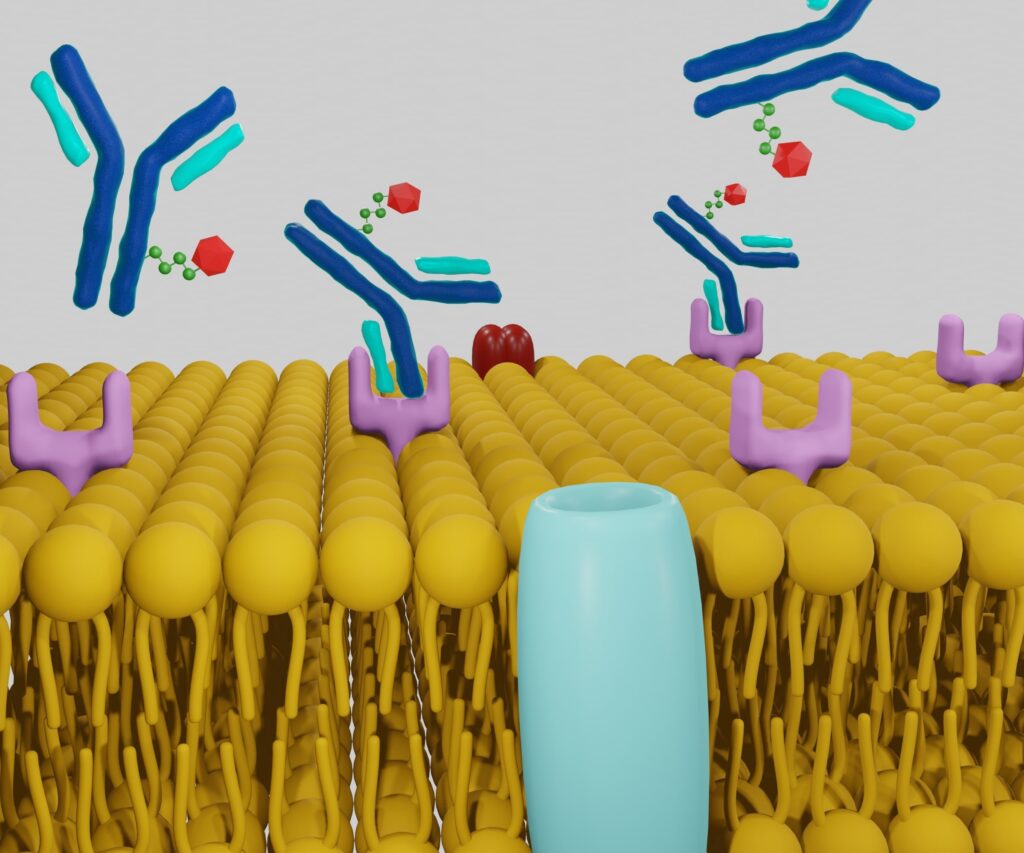
Radiotheranostics relies on the concept of targeting cancer cells at the molecular level using radiopharmaceuticals. These agents are composed of two main components: a targeting molecule that seeks out cancer cells and a radionuclide that emits radiation. Depending on the radionuclide’s properties, the radiopharmaceutical can either be used for diagnostic imaging or therapy.
- Diagnostic Imaging: For imaging purposes, a radionuclide that emits gamma rays, such as technetium-99m or iodine-123, is often used. These gamma rays can be detected by imaging technologies such as positron emission tomography (PET) or single-photon emission computed tomography (SPECT), enabling clinicians to locate tumours, assess the extent of disease, and evaluate treatment response.
- Targeted Radiotherapy: For therapeutic purposes, radionuclides that emit beta or alpha particles, such as lutetium-177 or actinium-225, are utilised. These particles deliver high-energy radiation directly to the cancer cells, causing DNA damage and cell death while sparing the surrounding healthy tissue.
In essence, radiotheranostics merges the diagnostic and therapeutic potential of radiopharmaceuticals into a single, seamless process, allowing for more accurate tumour localisation, tailored treatment, and real-time monitoring of therapeutic efficacy.
Applications in Cancer Treatment
Radiotheranostics has found its most significant application in treating neuroendocrine tumours (NETs) and prostate cancer, although ongoing research is expanding its potential to other cancer types.
- Neuroendocrine Tumours (NETs): One of the most successful applications of radiotheranostics is in the treatment of neuroendocrine tumours using peptide receptor radionuclide therapy (PRRT). NETs are rare cancers that arise from cells of the neuroendocrine system, and they frequently express high levels of somatostatin receptors. Radiolabelled somatostatin analogues, such as lutetium-177-DOTATATE, can specifically bind to these receptors, delivering targeted radiation to the tumour cells. PRRT has shown excellent results in improving progression-free survival and overall survival in patients with NETs.
- Prostate Cancer: Another important application is in prostate cancer, where prostate-specific membrane antigen (PSMA) is commonly overexpressed. Radiolabelled PSMA inhibitors, such as lutetium-177-PSMA, have been developed to target prostate cancer cells. These agents enable both imaging of metastatic prostate cancer and targeted radiotherapy, leading to improved outcomes in patients with advanced disease who have exhausted other treatment options.
- Other Cancers: Beyond NETs and prostate cancer, radiotheranostics is being investigated for use in a range of other malignancies. Research is ongoing to explore its potential in treating breast cancer, thyroid cancer, lymphoma, and glioblastoma, among others. With advancements in molecular biology and imaging technologies, the development of novel radiopharmaceuticals continues to expand the horizon for radiotheranostic applications.
Benefits of Radiotheranostics
The integration of diagnostics and therapeutics within a single platform offers numerous advantages over traditional cancer treatment approaches.
- Personalised Treatment: Radiotheranostics allows for a personalised approach to cancer care. By using molecular markers specific to each patient’s tumour, clinicians can tailor treatment strategies that are unique to the individual. This improves the efficacy of the treatment and reduces unnecessary exposure to harmful radiation.
- Targeted Therapy: Unlike conventional radiotherapy, which may affect surrounding healthy tissues, radiotheranostics delivers radiation directly to the cancer cells. This minimises damage to normal tissues and reduces the side effects commonly associated with cancer treatment, such as nausea, fatigue, and hair loss.
- Real-Time Monitoring: One of the most significant advantages of radiotheranostics is the ability to monitor the effectiveness of the treatment in real-time. By using diagnostic imaging to track the uptake of the radiopharmaceutical in the tumour, clinicians can assess how well the treatment is working and make adjustments if necessary.
- Improved Outcomes: Studies have shown that radiotheranostic treatments can improve overall survival and progression-free survival in patients with certain types of cancer. This is particularly true for NETs and prostate cancer, where targeted radiotherapy has been shown to significantly extend patient survival.
Challenges and Limitations
Despite the promising future of radiotheranostics, the field faces several challenges that must be addressed to realise its full potential.
- Limited Availability: One of the primary challenges is the limited availability of radiopharmaceuticals and specialised equipment. Radiotheranostic treatments are currently only available in a few specialised centres around the world, limiting access for many patients.
- High Costs: The cost of radiotheranostic agents and the associated imaging equipment is high, which may restrict widespread adoption. Additionally, the production of radionuclides requires specialised facilities, adding further to the cost.
- Toxicity: Although radiotheranostics offers more targeted therapy, it is not without potential side effects. Some patients may experience toxicity from the radiation, particularly to organs that express the same molecular markers as the tumour. For example, the kidneys and salivary glands are common sites of toxicity in patients undergoing PSMA-targeted therapy for prostate cancer.
- Regulatory Hurdles: The development and approval of new radiopharmaceuticals face stringent regulatory requirements. Given the radioactive nature of these agents, ensuring their safety and efficacy requires extensive clinical trials and oversight, which can slow down the process of bringing new therapies to market.
Future Directions and Innovations
The future of radiotheranostics looks promising, with ongoing research poised to overcome the current limitations and expand its applications.
- Development of Novel Radiopharmaceuticals: Researchers are actively working on developing new radiopharmaceuticals that can target a broader range of cancer types. Advances in molecular biology, bioengineering, and nanotechnology are expected to accelerate the discovery of novel targeting molecules and radionuclides, further enhancing the effectiveness of radiotheranostic treatments.
- Combination Therapies: There is growing interest in combining radiotheranostics with other cancer therapies, such as immunotherapy or chemotherapy. By using radiotheranostics to precisely target the tumour, clinicians may be able to enhance the effectiveness of other treatments and improve patient outcomes.
- Artificial Intelligence and Machine Learning: The integration of artificial intelligence (AI) and machine learning into radiotheranostics holds immense potential. AI can help optimise the selection of radiopharmaceuticals, improve image interpretation, and predict treatment responses, leading to more personalised and effective therapies.
- Theranostic Nanoparticles: Nanotechnology is also being explored for its potential in radiotheranostics. Theranostic nanoparticles can be engineered to carry both imaging and therapeutic agents, offering a highly precise platform for cancer diagnosis and treatment. These nanoparticles can be designed to enhance tumour targeting, reduce toxicity, and provide better imaging resolution.
Conclusion
Radiotheranostics represents a groundbreaking approach to cancer treatment, offering the possibility of more personalised, targeted, and effective therapies. By combining diagnostic imaging with targeted radiotherapy, radiotheranostics has already shown remarkable success in treating neuroendocrine tumours and prostate cancer. As research continues to advance, the potential applications of radiotheranostics in other cancers and the development of novel radiopharmaceuticals will further solidify its place as a key player in the future of oncology.
The benefits of radiotheranostics, including personalised treatment, targeted therapy, real-time monitoring, and improved outcomes, make it a promising tool in the fight against cancer. Although there are challenges to overcome—such as limited availability, high costs, and regulatory hurdles—the future of this field could revolutionise cancer treatment for years to come.
Radiotheranostics has the potential to provide patients with more effective, less toxic treatment options, ultimately improving their quality of life and long-term survival. As the field continues to evolve, it is likely to become an integral part of precision medicine, offering hope to cancer patients around the world.
Disclaimer
The information provided in this article, “Cancer Radiotheranostics: The Future of Targeted Cancer Therapy”, is intended for educational and informational purposes only. It is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Readers should not rely solely on the content presented here for making decisions related to healthcare or treatment options.
While every effort has been made to ensure the accuracy of the content at the time of publication, Open Medscience makes no representations or warranties regarding the completeness, accuracy, or reliability of any information contained in this article. The field of cancer research and radiotheranostics is rapidly evolving, and new developments may supersede some of the information presented.
Always consult with a qualified healthcare professional or medical specialist before making any decisions based on information found in this publication. Open Medscience, its authors, and contributors accept no liability for any loss, injury, or damage incurred as a result of the use or reliance on the content provided.
Any mention of specific products, treatments, or technologies does not constitute endorsement or recommendation by Open Medscience.
You are here: home » diagnostic medical imaging blog »