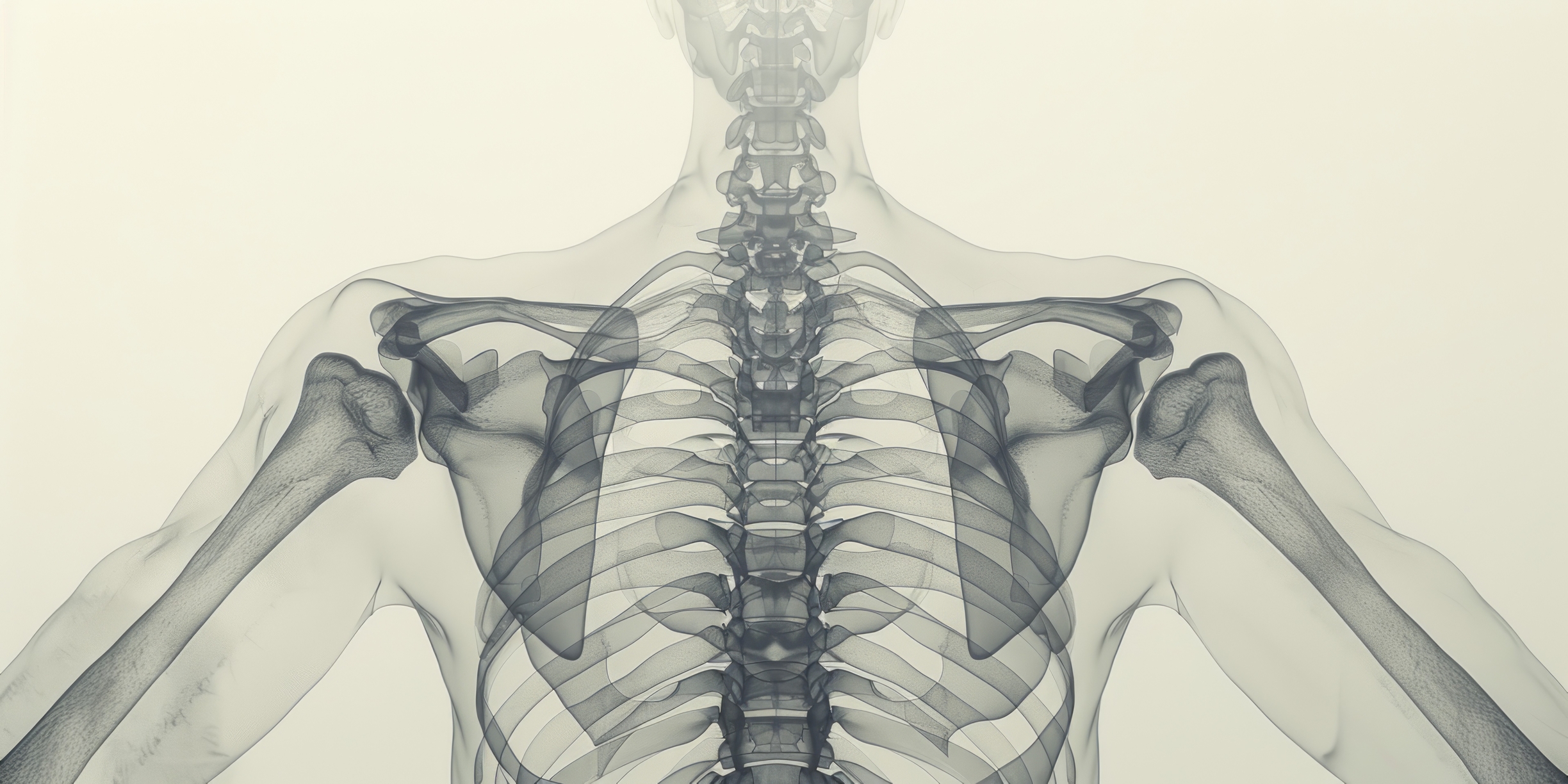
Medical imaging revolutionises healthcare by offering profound insight into human anatomy, with skeletal imaging specifically aiding diagnosis, treatment, and understanding structural intricacies and functions.
Skeletal Imaging
Medical imaging is essential to modern healthcare, providing valuable information about the human body’s structure, function, and health. Among the various tissues and systems of the body, the human skeleton plays a critical role in supporting and protecting our organs, enabling movement, and serving as a reservoir for minerals such as calcium and phosphorus. This article will discuss the various medical imaging techniques for visualising the human skeleton, their applications, advantages, limitations, and future prospects.
Conventional Radiography: The Enduring Relevance of X-ray Imaging in Modern Skeletal Assessment and Medical Diagnostics
Conventional radiography, commonly known as X-ray imaging, has been the cornerstone of medical imaging since its inception in 1895 by Wilhelm Conrad Röntgen. This revolutionary technique has transformed how healthcare professionals visualise the internal structures of the human body, particularly the skeletal system. As the oldest and most widely utilised imaging modality, X-ray imaging has continued to play a vital role in diagnosing and monitoring a broad range of medical conditions.
The principle of X-ray imaging relies on the differential absorption of X-rays by various tissues within the body. When X-ray beams pass through a body part, they are absorbed by tissues to varying degrees, depending on the density and composition of the tissues. For example, denser structures, such as bones, absorb more X-rays and appear lighter on the radiographic image, while less dense tissues like muscles and fat absorb fewer X-rays and appear darker. This contrast in absorption allows for the creation of detailed images of the internal structures, enabling healthcare providers to identify and assess potential abnormalities.
Since X-rays are the oldest imaging modality, conventional radiography has maintained its relevance in modern medicine due to its numerous advantages. It is a quick, non-invasive, and cost-effective diagnostic tool, making it accessible to a vast population worldwide. In addition, the technology has evolved significantly, with digital radiography systems replacing traditional film-based systems, enhancing image quality and reducing radiation exposure.
However, X-ray imaging has limitations, such as being less sensitive in detecting soft tissue abnormalities than other advanced imaging modalities compared to computed tomography (CT) or magnetic resonance imaging (MRI). Despite these limitations, conventional radiography remains an indispensable tool in modern medicine for assessing the human skeleton, providing valuable information for clinical decision-making and treatment planning.
Computed Tomography: Diagnostic Imaging with Advanced Visualisation and Expanding Applications
Computed tomography (CT) is a sophisticated X-ray-based imaging modality that has revolutionised diagnostic imaging since its invention in the 1970s. By applying computer algorithms, CT scans generate detailed cross-sectional images of the body, offering superior contrast and resolution compared to conventional radiography. The enhanced image quality provided by CT scans has expanded the scope of medical imaging, enabling healthcare professionals to visualise intricate structures and diagnose a broader range of conditions with increased accuracy.
In a CT scan, an X-ray source and detector rotate around the patient, capturing numerous projections from various angles. These projections are subsequently reconstructed into a series of two-dimensional cross-sectional images, which can be combined to generate a comprehensive three-dimensional representation of the body. This advanced imaging technology allows for improved visualisation of complex fractures, spinal injuries, joint disorders, and other skeletal abnormalities.
Beyond its application in musculoskeletal imaging, CT scans have proven invaluable in assessing bone tumours, infections, and degenerative conditions such as osteoporosis. In addition, the ability to visualise soft tissues in addition to bone has further broadened the utility of CT scans, making them essential tools for detecting and evaluating a wide array of pathologies, including those affecting the lungs, abdomen, and pelvis.
CT scans have also gained traction in interventional radiology, frequently employed to guide procedures such as biopsies, drainages, and ablations. By providing real-time, high-resolution images, CT scans facilitate precise targeting and positioning, which can significantly improve the safety and efficacy of these minimally invasive procedures.
Despite the numerous advantages of CT scans, some drawbacks exist. CT scans generally involve higher radiation doses than conventional radiography, which may raise concerns about long-term radiation exposure, especially in pediatric patients and individuals who require frequent imaging. Additionally, CT scans are more expensive, which can limit their accessibility and availability, particularly in resource-constrained healthcare settings.
Magnetic Resonance Imaging: Unveiling Soft Tissues and Skeletal Insights with Non-Ionising Diagnostic Precision
Magnetic Resonance Imaging (MRI) is a groundbreaking non-ionising imaging modality that revolutionised the field of diagnostic medicine. Developed in the 1970s, MRI uses a combination of powerful magnetic fields, radiofrequency pulses, and sophisticated computer algorithms to generate detailed images of the body’s internal structures. The technique is particularly effective for visualising soft tissues, providing valuable insights into various medical conditions and enabling accurate diagnoses.
In an MRI procedure, hydrogen nuclei present in the body are aligned within a strong magnetic field. Then, radiofrequency pulses are applied, causing these nuclei to absorb energy and change their alignment. As the nuclei gradually return to their original state, they release energy, which is detected and subsequently used to create images of the body’s internal structures.
Although MRI is not primarily used for skeletal imaging, it can offer valuable information about bone marrow and surrounding soft tissues. This modality evaluates bone tumours, infections, and metabolic bone diseases. Additionally, MRI effectively visualises cartilage, tendons, and ligaments, making it a powerful tool for diagnosing and monitoring joint disorders such as osteoarthritis, rheumatoid arthritis, and sports injuries.
The primary advantage of MRI is its ability to visualise soft tissues in detail without exposing patients to ionising radiation, which can pose health risks with prolonged exposure. Moreover, MRI images can be acquired in multiple planes, allowing for enhanced visualisation of complex anatomical structures that might otherwise be challenging to observe using other imaging techniques.
Notwithstanding its numerous advantages, MRI also has certain limitations; for example, the procedure is generally more expensive and time-consuming than other imaging modalities, such as X-rays and CT scans. Furthermore, MRI is contraindicated for patients with specific implanted devices, like pacemakers and certain metallic implants, as the strong magnetic fields could interfere with their function or cause harm to the patient.
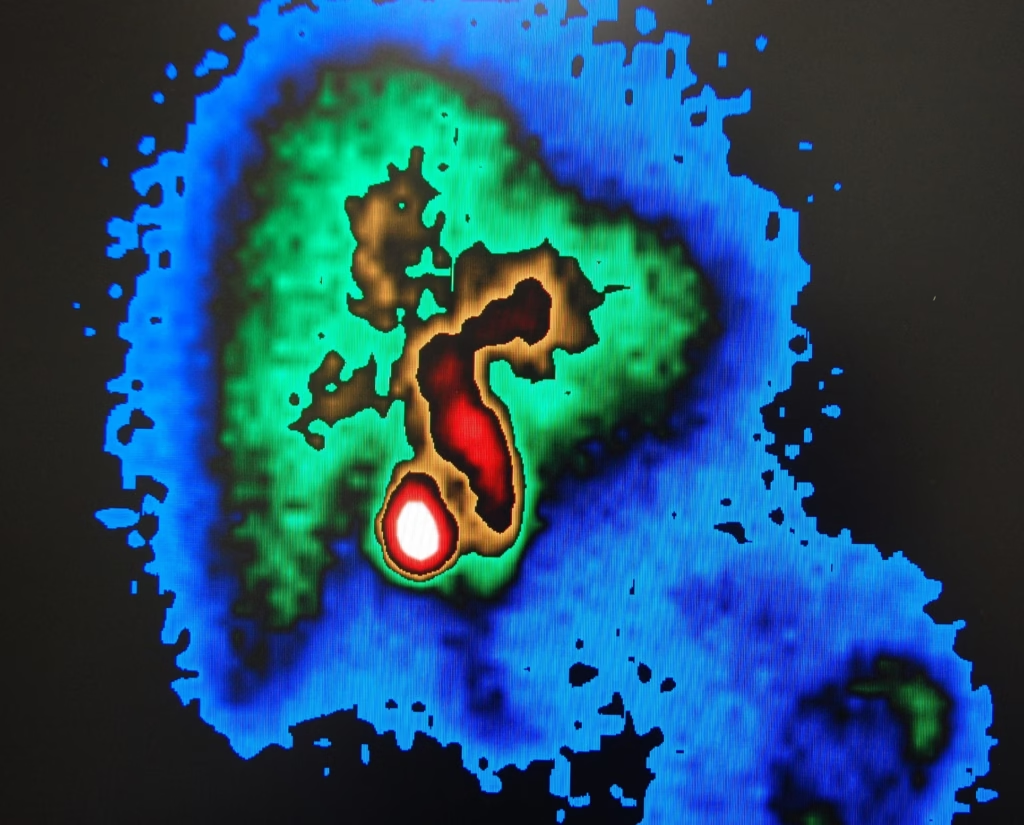
Bone Scintigraphy: Harnessing Nuclear Medicine for Early Detection and Monitoring of Skeletal Disorders
Nuclear medicine imaging, or bone scintigraphy, is a functional imaging technique that has revolutionised how physicians diagnose and treat various bone-related disorders. Pioneered in the 1950s, employed small amounts of radioactive substances to visualise the metabolic activity within the skeleton, allowing for the detection of changes in bone metabolism before they are discernible through other imaging techniques.
Bone scintigraphy begins with injecting a radiopharmaceutical, typically technetium-99m-labelled diphosphonate, into the patient’s bloodstream. This compound exhibits a predilection for areas of high bone turnover, such as sites of injury, infection, or tumour growth. A gamma camera subsequently captures the emitted radiation, generating images depicting the radiopharmaceutical distribution within the skeletal system.
This imaging modality is instrumental in detecting and monitoring metastatic bone disease, primary bone tumours, and infections. Furthermore, evaluating treatment response and identifying the source of unexplained bone pain is crucial. With its ability to provide whole-body imaging and high sensitivity for detecting early changes in bone metabolism, bone scintigraphy has become an indispensable tool in the medical field.
Despite its numerous advantages, bone scintigraphy does possess certain limitations. Its specificity is somewhat restricted, as various conditions can produce similar uptake patterns, potentially leading to misinterpretation. Moreover, this imaging technique involves exposure to ionising radiation, raising concerns about the cumulative effects of radiation exposure, especially in patients requiring multiple scans. Additionally, bone scintigraphy offers limited anatomical detail compared to other imaging modalities, such as CT and MRI.
Ultrasound in Skeletal Imaging: Applications, Advantages, and Limitations of a Non-Invasive Diagnostic Approach
Ultrasound, or sonography, is a non-invasive imaging technique that employs high-frequency sound waves to generate images of the body’s internal organs and structures. This technology was developed in the 1940s; ultrasound has become an essential diagnostic tool in modern medicine. However, primarily used for imaging soft tissues, such as organs, muscles, and blood vessels, ultrasound has limited applications for skeletal imaging due to its inability to penetrate dense bone structures effectively.
The ultrasound imaging process involves placing a transducer on the skin, which emits sound waves that penetrate the body and reflect off internal structures. The returning echoes are detected by the transducer and used to create real-time images that can be viewed on a monitor. This real-time visualisation allows healthcare professionals to observe the function and movement of internal structures, making ultrasound particularly useful for guiding procedures such as needle biopsies and catheter insertions.
While not as effective for imaging dense bones as other modalities like X-ray or CT, ultrasound can evaluate superficial bones such as the ribs and certain joints like the shoulder and knee. It is also useful for assessing bone healing, particularly in infants and children whose bones are less dense and more sonolucent. Furthermore, ultrasound can be employed to diagnose soft tissue injuries, such as tendon or ligament tears, and to monitor the progress of bone fractures during the healing process.
Ultrasound provides multiple benefits compared to other imaging methods. As a non-ionising technique, it avoids subjecting patients to the potentially harmful ionising radiation found in X-rays and CT scans. Additionally, ultrasound is portable and economical, making it an appealing choice for imaging in specific circumstances, especially in rural or isolated regions with restricted access to more sophisticated imaging technology.
However, ultrasound does have some limitations. For example, its penetration depth is limited, and it cannot effectively visualise deeper bones or the internal structure of bone. Additionally, the quality of the images depends on the operator’s skill, and certain factors, such as the presence of gas or obesity, can impede the transmission of sound waves and reduce image quality.
Navigating the Evolution of Skeletal Imaging: Advancements, Modalities, and Their Impact on Modern Patient Care
In summary, medical imaging of the human skeleton has undergone a remarkable transformation over the years, with numerous modalities available to diagnose and monitor skeletal disorders. The evolution of these imaging techniques has significantly enhanced our ability to detect and manage a wide range of bone and joint conditions. However, each imaging modality has unique advantages and limitations, and the choice of the most appropriate technique depends on the clinical scenario, patient factors, and available resources.
Radiography, or X-ray imaging, has been the cornerstone of skeletal imaging since its discovery in 1895. It is a simple, cost-effective, and widely available method for detecting fractures, dislocations, and other bone abnormalities. However, its limited sensitivity for soft tissue structures and the potential risks associated with ionising radiation are important considerations.
CT scans provide high-resolution, cross-sectional images of the skeletal system, making it ideal for detecting subtle fractures, assessing complex anatomical structures, and planning surgical interventions. Despite its higher radiation dose than conventional X-rays, CT scans offer more detailed information on bone and joint pathologies.
MRI has revolutionised skeletal imaging by providing exceptional detail of bone and soft tissue structures without ionising radiation. MRI is particularly valuable for evaluating bone marrow disorders, infections, tumours, and joint conditions. However, the major limitations of MRI include its high cost, longer scanning times, and contraindications in patients with certain implanted devices.
Besides these traditional imaging methods, promising modalities like Positron Emission Tomography (PET) and Optical Imaging are emerging, offering the potential for even greater accuracy and specificity in diagnostic capabilities. As technology advances, we can anticipate further improvements in the quality, safety, and accessibility of skeletal imaging. These advancements will inevitably enhance our capacity to diagnose and treat many bone and joint conditions, ultimately improving patient care and outcomes.
Disclaimer
The information presented in this article, Medical Imaging of the Human Skeleton, is intended for general informational and educational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. The content reflects current knowledge and understanding as of the publication date (13 April 2023) and may not represent the most up-to-date developments in the field of medical imaging.
Open Medscience does not guarantee the accuracy, completeness, or reliability of the information contained in this article. Readers should not rely solely on this content for making health-related decisions. Always consult a qualified healthcare provider or medical professional for advice regarding any medical condition or imaging procedure.
Any mention of specific imaging technologies, techniques, or manufacturers is for illustrative purposes and does not imply endorsement. The views expressed are those of the authors and do not necessarily reflect the views of Open Medscience or its affiliates.
Open Medscience shall not be held liable for any direct or indirect damages resulting from the use or misuse of the information contained in this article.
home » blog » human anatomy »