Advanced medical imaging has revolutionised liver disease detection, diagnosis, and management, improving diagnostic accuracy and personalized therapeutic interventions.
The Essential Functions of the Liver in the Human Body
The liver, a vital organ in the human body, performs essential functions such as metabolism, detoxification, and synthesis of proteins. Therefore, detecting and diagnosing liver diseases is crucial for appropriate treatment and management. Advanced medical imaging techniques are pivotal in detecting, diagnosing, and monitoring liver diseases. This article introduces various advanced imaging techniques for liver assessment and their clinical applications.
Ultrasonography: A Non-Invasive Imaging Technique for Liver Evaluation
Ultrasonography is a non-invasive imaging method that uses high-frequency sound waves to produce images of internal organs and structures, such as the liver. This imaging modality has undergone numerous advancements, significantly improving its diagnostic capabilities. The ultrasound toolbox consists of Conventional ultrasonography, or B-mode ultrasound, commonly used as the first-line imaging modality for liver evaluation. It can identify morphological changes such as liver cirrhosis or tumours and assess the liver’s size, shape, and echogenicity. This non-invasive technique is cost-effective, widely available, and has no known harmful effects. Furthermore, it can be performed in real-time, allowing for a dynamic assessment of the liver and its vasculature.
However, conventional ultrasonography has its limitations. It is operator-dependent, which means that the accuracy of the examination heavily relies on the expertise of the sonographer. Moreover, its sensitivity in detecting small lesions, mainly those less than 1 cm in diameter, is limited. This may lead to missed or delayed diagnoses, especially in the early stages of liver diseases.
Throughout the years, numerous advancements in ultrasonography have emerged to address its limitations and augment its diagnostic prowess.
- Doppler Ultrasonography is used to assess blood flow within the liver’s vessels. It helps evaluate portal hypertension, liver vascular disorders, and the detection of vascular invasion by tumours. Doppler ultrasonography has become an essential tool in liver transplantation, where it is used to evaluate the patency and flow within hepatic vessels.
- Contrast-Enhanced Ultrasonography (CEUS) involves using microbubble contrast agents, which are injected intravenously to enhance the visualisation of blood vessels and tissues. This technique improves the detection and characterisation of liver lesions, including hepatocellular carcinoma, metastases, and focal nodular hyperplasia. CEUS can also monitor the treatment response in patients undergoing locoregional therapy for the liver.
Non-Invasive Assessment of Liver Fibrosis Using Strain and Shear Wave Elastography
Liver fibrosis and cirrhosis represent severe conditions that may result in liver failure, potentially necessitating a liver transplant. Therefore, early diagnosis and monitoring are crucial for managing these conditions and reducing complications. Elastography is a non-invasive imaging technique that measures the stiffness of liver tissue, which can indicate the presence of fibrosis or cirrhosis. Two main types of elastography are used for liver assessment:
Strain elastography, also known as compression elastography or static elastography, is the first generation of elastography techniques. It involves manually applying pressure to the tissue of interest with an ultrasound transducer, causing the tissue to deform. The deformation of the tissue is then measured by comparing the pre-compression and post-compression ultrasound images. The degree of deformation indicates tissue stiffness; less deformation means stiffer tissue, which can indicate liver fibrosis or cirrhosis.
However, strain elastography has limitations, such as being operator-dependent and highly susceptible to external factors like patient movement or breathing. Additionally, strain elastography does not provide absolute measurements of tissue stiffness, making it challenging to compare results across different examinations or patients.
Shear wave elastography, a more advanced form of elastography, overcomes many of the limitations of strain elastography. This technique uses specialised ultrasound transducers to generate acoustic radiation force impulses (ARFI) within the tissue.
These impulses create shear waves that propagate through the tissue, and the velocity of these waves is directly related to the tissue’s stiffness. The faster the shear waves travel, the stiffer the tissue. Shear wave elastography has several advantages over strain elastography.
First, it is less operator-dependent, as the ultrasound transducer generates the ARFI rather than relying on manual compression. Second, shear wave elastography provides quantitative measurements of tissue stiffness, which can be compared across different examinations or patients. Finally, this technique is less susceptible to external factors like patient movement or breathing, making it more reliable and accurate.
Elastography has various clinical applications, particularly in assessing and monitoring liver fibrosis and cirrhosis. In addition, it can be used to:
- Assess patients susceptible to liver fibrosis or cirrhosis, including individuals with chronic hepatitis B or C, non-alcoholic fatty liver disease (NAFLD), or alcohol-associated liver disease. Monitor disease progression in patients with established liver fibrosis or cirrhosis, providing valuable information to guide treatment decisions and adjust therapy as needed.
- Assess treatment response in patients receiving antiviral therapy or other treatments for liver disease, helping to determine the effectiveness of the intervention and inform ongoing management.
Computed Tomography: A Powerful Tool for Liver Imaging and Intervention
Computed tomography (CT) is an advanced medical imaging technique that uses X-ray technology to produce detailed, cross-sectional images of the body’s internal structures. One of the primary applications of CT is the imaging and evaluation of the liver, where it has become an indispensable tool for clinicians. Conventional CT assesses liver anatomy, detect and characterises liver lesions, and stage liver malignancies. Furthermore, it plays a significant role in planning and monitoring various interventions, such as ablations or transarterial chemoembolisation (TACE).
The liver is a complex organ with various anatomical structures and functional units. Therefore, an accurate assessment of liver anatomy is essential for diagnosing and managing liver diseases. CT provides a non-invasive method for visualising liver anatomy, including assessing the liver size, shape, and structural abnormalities. In addition, it allows for identifying liver lobes, segments, and vascular structures, such as the hepatic artery, portal vein, and hepatic veins. By providing detailed images of the liver, CT aids in evaluating underlying liver diseases and helps guide appropriate treatment plans.
Liver lesions refer to atypical growths or regions of tissue injury within the liver, which can be either benign or malignant. Characterisation is vital for establishing the proper course of treatment. CT is a powerful diagnostic tool for detecting and characterising liver lesions. It can identify various liver lesions, such as cysts, hemangiomas, focal nodular hyperplasia, and malignant tumours.
Using contrast-enhanced CT, radiologists can evaluate the enhancement patterns of liver lesions, essential for characterising the lesion and differentiating between benign and malignant growths. For example, hepatocellular carcinoma (HCC), the most common primary liver cancer, typically shows arterial enhancement and washout in the venous phase. These characteristic patterns help radiologists and clinicians establish a diagnosis and select the most suitable management approach.
Accurate staging of liver malignancies is vital for determining prognosis and guiding treatment decisions. CT is widely used for this purpose, as it can provide detailed information about the extent of the tumour. Also, its involvement in liver vasculature and the presence of extrahepatic metastases. The TNM (Tumour, Node, Metastasis) staging system is used for liver malignancies, and CT plays a significant role in determining each component of the staging system. By providing comprehensive information about tumour size, number, and location, as well as the involvement of lymph nodes and distant metastases, CT is an essential tool for liver cancer staging.
CT is valuable for diagnostic purposes and crucial for planning and monitoring liver interventions. Ablation therapy involves using heat or cold to destroy tumour cells and is a minimally invasive treatment option for patients with small liver tumours. CT guidance ensures precise tumour targeting and minimises damage to surrounding healthy tissue. Moreover, CT is used to monitor the effectiveness of the treatment and assess for any complications.
Transarterial chemoembolisation (TACE) is another liver-directed therapy primarily used to treat hepatocellular carcinoma. TACE involves the injection of chemotherapy drugs and embolic agents directly into the blood vessels supplying the tumour, leading to tumour ischemia and necrosis. CT is used to identify the appropriate blood vessels for catheter placement and to monitor the treatment response.
Dual-Energy Computed Tomography: A Game Changer Tumour Liver Imaging
Dual-Energy Computed Tomography (DECT) is an advanced medical imaging technique that acquires images at two different X-ray energy levels, enabling the differentiation of various tissue types and enhancing the detection of small liver lesions. DECT is beneficial for characterising liver tumours, assessing liver steatosis, and identifying liver inflammation. This technology has revolutionised liver imaging, offering several advantages over traditional single-energy computed tomography (SECT).
DECT leverages that different tissue types absorb and scatter X-ray photons differently at varying energy levels. By acquiring images at two different energy levels, DECT can generate material-specific images that enhance the differentiation of various tissue types. This ability to distinguish between tissues has proven advantageous in detecting small liver lesions, which may otherwise be missed or misdiagnosed on conventional imaging modalities.
DECT plays a crucial role in characterising liver tumours by offering a more precise and accurate evaluation of the tumour composition. This is particularly important for differentiating between benign and malignant liver tumours, which can significantly impact treatment planning and patient prognosis. DECT’s ability to generate iodine-specific images has also made it possible to identify and quantify iodine uptake within liver tumours. This quantitative information can provide valuable insights into tumour vascularity and response to therapy, further improving the clinical management of patients with liver cancer.
Fatty liver, also referred to as liver steatosis, is a widespread condition characterised by excessive fat accumulation in the liver. Left untreated, it can progress to more severe liver diseases, such as non-alcoholic steatohepatitis (NASH), cirrhosis, and hepatocellular carcinoma. DECT has emerged as a powerful diagnostic tool for assessing liver steatosis, providing a non-invasive means to quantify the degree of fat infiltration. In addition, with the ability to differentiate between water and fat components in the liver, DECT can accurately measure the liver fat content and monitor the progression of steatosis over time.
Liver inflammation, frequently resulting from viral hepatitis, autoimmune disorders, or drug-induced liver injury, has the potential to cause substantial liver damage and may eventually lead to liver failure. Therefore, early identification and appropriate management of liver inflammation are crucial to prevent further deterioration of liver function. DECT has shown promise in detecting and quantifying liver inflammation by generating virtual non-contrast images highlighting inflammation-related tissue changes.
This technique enables clinicians to differentiate inflammatory changes from other causes of liver damage, such as fibrosis or steatosis, facilitating prompt and accurate diagnosis.
DECT offers several advantages over traditional SECT in liver imaging. These include:
- DECT’s ability to generate material-specific images results in improved image quality, with increased contrast resolution and reduced beam-hardening artefacts.
- By simultaneously acquiring images at two different energy levels, DECT can achieve comparable or even lower radiation doses than SECT while maintaining diagnostic accuracy.
- DECT allows for advanced post-processing techniques, such as virtual non-contrast imaging and material decomposition, enabling more accurate and detailed evaluations of liver diseases.
- The additional information DECT provides radiologists makes more confident diagnoses, reducing the need for invasive diagnostic procedures, such as liver biopsy.
The Versatility of Magnetic Resonance Imaging in Liver Assessment
Magnetic Resonance Imaging (MRI) is a non-invasive medical imaging technique that utilises powerful magnets and radiofrequency waves to generate detailed images of the liver without employing ionising radiation. Conventional MRI offers high spatial resolution for visualising liver anatomy and pathology, rendering it an invaluable resource for assessing the liver size, detecting focal liver lesions, and evaluating biliary structures.
Various MRI sequences, such as T1-weighted, T2-weighted, and fat-suppressed sequences, are used to obtain detailed liver images. In addition, advanced MRI techniques, such as Contrast-Enhanced MRI (CE-MRI) and Diffusion-Weighted Imaging (DWI), further improve the diagnostic capabilities of MRI in liver assessment.
Contrast-Enhanced MRI (CE-MRI) uses gadolinium-based contrast agents to improve the visualisation of liver lesions and blood vessels. By enhancing the contrast between healthy and abnormal liver tissue, contrast-enhanced MRI (CE-MRI) facilitates more accurate detection and characterisation of liver lesions.
Additionally, it is beneficial in identifying and characterising liver tumours, as the contrast agents assist in distinguishing between benign and malignant lesions according to their enhancement patterns. This information is crucial for determining the appropriate treatment strategies and predicting patient outcomes.
CE-MRI is also valuable in assessing liver fibrosis, a condition characterised by the excessive accumulation of fibrous tissue in the liver. Using contrast agents enables the visualisation of liver parenchymal changes and the degree of fibrosis, aiding in diagnosing and staging liver diseases, such as chronic hepatitis and cirrhosis.
Furthermore, CE-MRI can be used to evaluate the post-treatment response of liver tumours. By comparing the enhancement patterns before and after treatment, clinicians can assess the effectiveness of various therapies, such as chemotherapy, radiotherapy, and liver resection, in eradicating or reducing the tumour burden.
Diffusion-Weighted Imaging (DWI) is an advanced MRI technique that measures the diffusion of water molecules within tissues. By examining the movement of water molecules, DWI can provide valuable information on the microstructural properties of liver tissue, allowing for better differentiation between normal and abnormal tissue.
DWI is useful for detecting small liver lesions that conventional MRI sequences may miss, as these lesions often exhibit restricted diffusion due to their higher cellularity. The ability to detect small lesions is essential in the early diagnosis of liver cancer, as it enables timely treatment and improves patient prognosis.
In addition to lesion detection, DWI can characterise liver tumours. By analysing the apparent diffusion coefficient (ADC) values, representing the degree of water molecule diffusion within a given tissue, radiologists can differentiate between benign and malignant liver lesions. Lower ADC values are typically associated with malignant tumours, as they exhibit higher cellularity and restricted water diffusion.
DWI is also beneficial in evaluating liver fibrosis, as the diffusion of water molecules is affected by the presence of fibrous tissue. In addition, studies have demonstrated a correlation between decreased ADC values and increased liver fibrosis stages, suggesting that DWI can be used as a non-invasive tool for fibrosis assessment and staging.
Liver Malignancy Diagnosis: The Power of PET/CT and PET/MRI Imaging in Assessing Metabolic Activity and Anatomical Details
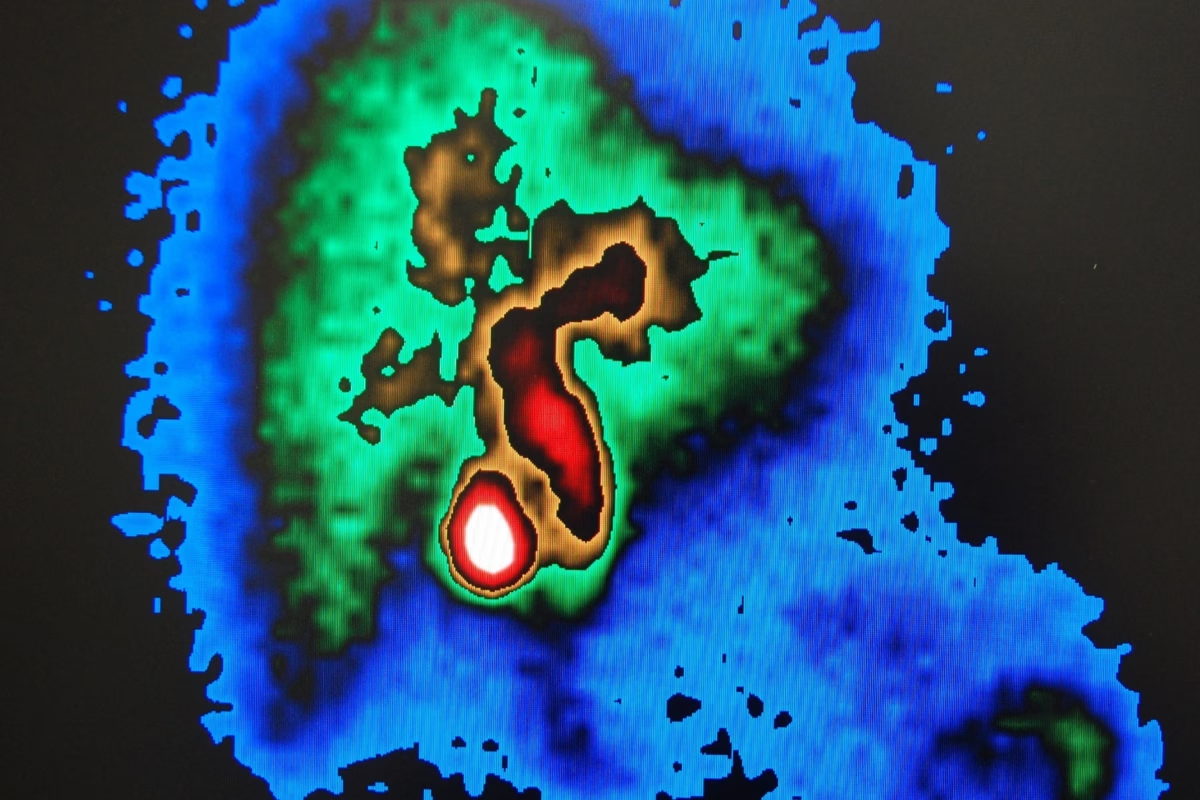
Positron Emission Tomography (PET) is a nuclear medicine imaging technique that has revolutionised the field of medical diagnostics by providing vital insights into cellular metabolic activity. This is achieved by tracking a radiotracer, usually fluorodeoxyglucose (FDG), which allows for visualising physiological processes that cannot be observed through conventional imaging modalities. PET/CT and PET/MRI are hybrid imaging techniques that amalgamate the functional information derived from PET with the anatomical details obtained from CT or MRI scans. These advanced imaging modalities have proven exceptionally useful in diagnosing, staging, and restaging liver malignancies, assessing treatment response, and detecting recurrent disease.
Liver malignancies represent a significant challenge in medical diagnostics due to their complexity and heterogeneity. The liver, a crucial organ with numerous metabolic and detoxification roles, is vulnerable to various diseases, including cancer. Primary liver cancers, including hepatocellular carcinoma (HCC), cholangiocarcinoma, and metastatic liver lesions stemming from colorectal, breast, or lung cancer, represent the most prevalent liver malignancies. Therefore, accurate diagnosis and staging of liver malignancies are essential for determining the appropriate treatment strategy and predicting the disease’s prognosis.
PET/CT and PET/MRI have emerged as powerful imaging tools that provide complementary information to traditional imaging techniques, such as ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI). Combining the metabolic data from PET with the anatomical precision of CT or MRI, these hybrid imaging modalities offer a more comprehensive and accurate assessment of liver malignancies.
The key to PET imaging lies in its ability to detect the metabolic activity of cells by tracking the uptake of radiotracers. In the case of liver malignancies, FDG is the most commonly used radiotracer. FDG is a glucose analogue that accumulates in cells with high metabolic activity, such as tumour cells. This differential uptake of FDG allows for identifying malignant lesions, as they display increased metabolic activity compared to healthy liver tissue. In addition, PET imaging can provide valuable information regarding tumour aggressiveness, as highly aggressive tumours tend to exhibit higher FDG uptake.
PET/CT and PET/MRI offer several advantages for staging and restaging liver malignancies. They provide a comprehensive assessment of the tumour burden in the liver, as well as identify extrahepatic metastases that may impact treatment planning. Furthermore, these hybrid imaging modalities can evaluate the response to various treatment modalities, including surgery, chemotherapy, and targeted therapies. By comparing pre- and post-treatment PET scans, clinicians can determine the effectiveness of the treatment and make informed decisions regarding the need for further intervention or the modification of the treatment plan.
A major obstacle in managing liver malignancies is identifying instances of recurring disease. Patients who undergo surgical resection or other curative treatments risk developing recurrent tumours within the liver or other organs. PET/CT and PET/MRI have proven to be highly sensitive in detecting recurrent liver malignancies, enabling early intervention and improving patient outcomes.
Despite the numerous advantages of PET/CT and PET/MRI in managing liver malignancies, these imaging techniques also have some limitations. The high cost of these modalities and limited availability in some regions may restrict their widespread use. Furthermore, PET imaging relies on the differential uptake of radiotracers, which may not always accurately reflect the metabolic activity of all tumour types.
Hepatobiliary-Specific PET Radiotracers
In recent years, nuclear medicine has witnessed significant advancements in developing new and improved radiotracers for positron emission tomography (PET) imaging. These advances have shown great potential in detecting and characterising liver lesions, particularly in the context of hepatocellular carcinoma (HCC). Two notable hepatobiliary-specific PET radiotracers that have garnered significant attention are 18F-fluorocholine and 11C-acetate. These novel radiotracers have improved sensitivity and specificity for liver lesion detection, offering promising alternatives to conventional imaging modalities.
Hepatocellular carcinoma (HCC) is the most common primary liver malignancy, with its worldwide incidence continually increasing. Thus, early and precise detection of HCC is essential for optimal patient care and enhanced prognosis. Traditional imaging techniques, like computed tomography (CT) and magnetic resonance imaging (MRI), are extensively employed to detect and characterise liver lesions. However, these approaches may be limited, particularly when lesions are small, indeterminate, or masked by preexisting liver disease.
18F-fluorocholine, a radiolabelled choline analogue, is a newer hepatobiliary-specific PET radiotracer promising in detecting liver lesions. Choline is a precursor of phosphatidylcholine, a major component of cell membranes. Malignant cells, including HCC, exhibit increased choline uptake and metabolism, which can be exploited for imaging. Early studies of 18F-fluorocholine PET imaging have demonstrated improved sensitivity and specificity for detecting HCC compared to traditional imaging techniques. Furthermore, this radiotracer has shown potential for differentiating between benign and malignant liver lesions and assessing treatment response in HCC patients.
Another emerging radiotracer, 11C-acetate, has demonstrated potential for detecting and characterising liver lesions. Acetate is involved in lipid synthesis and is preferentially taken up by HCC cells due to their enhanced lipogenesis. 11C-acetate PET imaging has shown promising results in detecting HCC, especially in cases where traditional imaging modalities have yielded inconclusive results. Moreover, 11C-acetate PET has helped identify extrahepatic metastases, which can significantly impact patient management and treatment planning.
Ablation Techniques for Liver Tumours
Ablation techniques have revolutionised the treatment of liver tumours, providing a minimally invasive and highly effective alternative to traditional surgery. These cutting-edge procedures, including radiofrequency ablation (RFA), microwave ablation (MWA), and cryoablation, utilise imaging guidance to precisely target and destroy tumour tissue while preserving healthy liver tissue. This approach is particularly advantageous for patients with unresectable liver tumours or those who are not suitable candidates for liver transplantation.
Radiofrequency ablation (RFA) is the most commonly utilised ablation method for treating liver tumours. It employs high-frequency electrical currents to generate heat, which causes coagulative necrosis of the targeted tissue. This method is generally safe, with minimal complications, and can be performed using local anaesthesia or conscious sedation. RFA is effective for treating small to medium-sized tumours, and several sessions may be required for larger tumours.
Microwave ablation (MWA) is another heat-based ablation technique that uses electromagnetic waves to create friction within the tumour cells, generating heat and leading to cellular death. MWA is known for its rapid heating and larger ablation zones, making it suitable for treating more extensive tumours. It also has a reduced risk of heat-sink effect compared to RFA, which can improve treatment outcomes.
Cryoablation, on the other hand, employs extremely cold temperatures to destroy tumour cells. This technique uses argon gas to create an ice ball around the tumour, freezing and ultimately destroying the cells. Cryoablation is advantageous in some instances, as it preserves the extracellular matrix and reduces the risk of haemorrhage, which can be crucial for patients with compromised liver function.
In summary, ablation techniques have emerged as an effective and minimally invasive option for treating liver tumours. These methods, including RFA, MWA, and cryoablation, offer hope to patients who may not be candidates for traditional surgical interventions while minimising complications and improving recovery times.
Transarterial Therapies for Liver Malignancies
Transarterial therapies, including transarterial chemoembolisation (TACE) and transarterial radioembolisation (TARE), have revolutionised the treatment of liver malignancies by providing minimally invasive, targeted therapy to patients suffering from unresectable hepatocellular carcinoma (HCC) or liver metastases. These advanced techniques have emerged as a viable alternative to traditional surgical resection, offering several advantages, such as reduced morbidity and faster recovery time.
TACE is a procedure that combines the administration of chemotherapy drugs with embolisation, a process that obstructs blood flow to the tumour. The chemotherapy agent is injected directly into the hepatic artery, delivering a high drug concentration to the tumour while minimising systemic side effects. Simultaneously, embolic agents are introduced to block the blood supply, starving the tumour of essential nutrients and oxygen. This dual approach maximises the therapeutic effect while minimising damage to healthy liver tissue.
TARE, on the other hand, involves the delivery of radioactive microspheres, commonly known as Yttrium-90 (Y-90), into the hepatic artery. These microspheres emit beta radiation, selectively targeting and destroying cancer cells in the liver. By delivering radiation directly to the tumour, TARE spares healthy tissue and has been associated with fewer side effects compared to conventional external beam radiation therapy.
Both TACE and TARE offer significant benefits in controlling tumour growth and alleviating symptoms for patients with unresectable HCC or liver metastases. While they are not curative, these therapies can prolong survival and improve quality of life, making them a valuable addition to the treatment arsenal for liver cancer patients.
Conclusion
Advanced medical imaging techniques have profoundly transformed the liver disease detection, diagnosis, and management landscape. Technologies such as ultrasonography, CT, MRI, PET, and interventional radiology have provided clinicians with a comprehensive toolkit to evaluate liver function, characterise lesions, assess fibrosis, and monitor treatment response. These innovations have enhanced diagnostic accuracy and facilitated more personalised and targeted therapeutic interventions, ultimately improving patient outcomes. As research and technological advancements progress, we can anticipate even more sophisticated liver imaging capabilities, paving the way for further breakthroughs in preventing, diagnosing, and treating liver diseases. The future of liver imaging is bright, and with it comes the promise of better, more efficient healthcare for patients worldwide.
Disclaimer
The content provided in this article, Medical Imaging of the Liver: Techniques and Applications, is for informational and educational purposes only. It is not intended to serve as a substitute for professional medical advice, diagnosis, or treatment.
Open Medscience does not offer medical advice or clinical services. Any medical decisions should be made in consultation with qualified healthcare professionals. While every effort has been made to ensure the accuracy and reliability of the information presented, Open Medscience makes no warranties or guarantees regarding its completeness, timeliness, or applicability to individual cases.
Readers should not disregard or delay seeking professional medical advice based on the information contained in this article. The inclusion of imaging techniques and technologies does not imply endorsement or suitability for all patients or clinical scenarios.
Use of this article and reliance on any information provided is solely at the reader’s own risk.
home » blog » human anatomy »