Dosimetry in radionuclide therapy involves measuring and calculating the absorbed radiation dose delivered to tissues in the body. This field is crucial for effectively treating cancers and other diseases while minimising damage to healthy tissues. This article reviews the fundamental concepts of dosimetry, methods of dose calculation, advances in imaging and software tools, clinical applications, and future directions. Through a detailed examination, we aim to provide a comprehensive understanding of how dosimetry enhances the precision and effectiveness of radionuclide therapy.
Introduction to Radionuclide Therapy
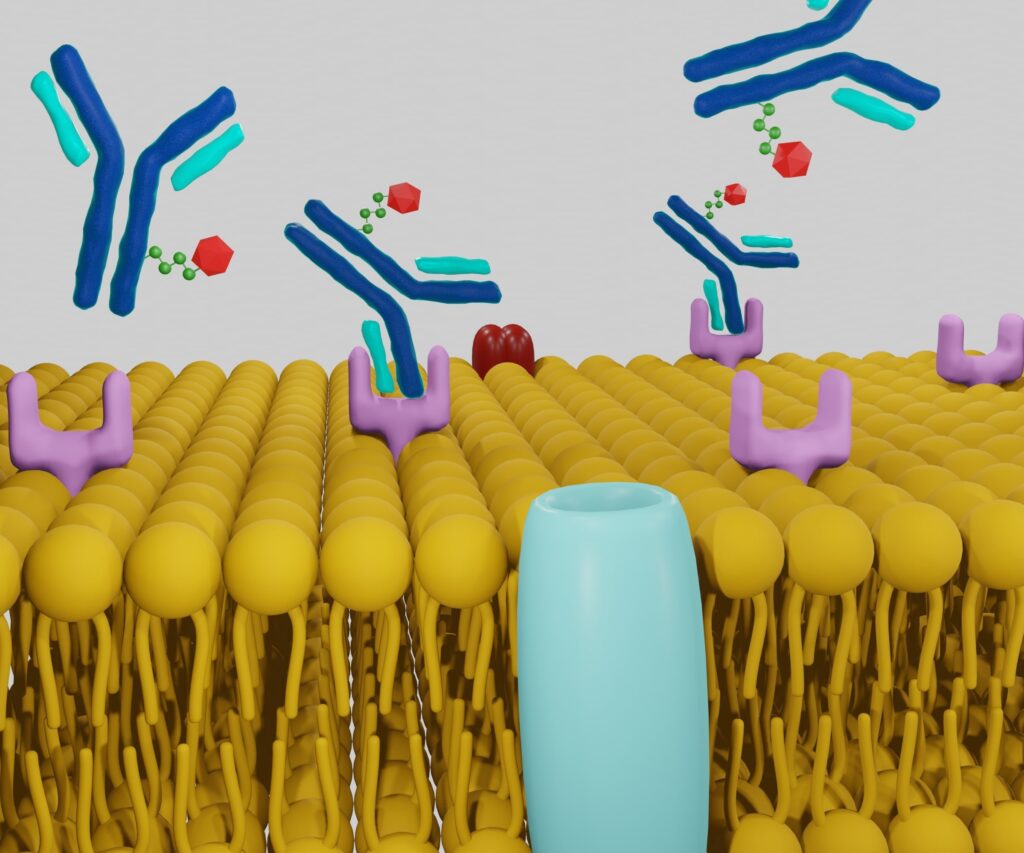
Radionuclide therapy is a form of targeted treatment that uses radioactive substances to treat various conditions, most notably cancer. The therapy involves the administration of radiopharmaceuticals, which are compounds containing radioactive isotopes. These compounds target specific cells or tissues, delivering a lethal dose of radiation to malignant cells while sparing surrounding healthy tissue as much as possible.
The Role of Dosimetry in Radionuclide Therapy
Dosimetry is the science of measuring and calculating the radiation dose the human body receives. In the context of radionuclide therapy, dosimetry plays a pivotal role in optimising treatment efficacy and safety. Accurate dosimetry ensures that the intended dose is delivered to the target tissues, enhancing therapeutic outcomes and reducing the risk of adverse effects.
Fundamental Concepts of Dosimetry
Absorbed Dose
The absorbed dose is the amount of radiation energy deposited per unit mass of tissue, measured in grays (Gy). This is a crucial parameter in assessing the biological impact of radiation on tissues.
Equivalent Dose
The equivalent dose takes into account the type of radiation used, providing a measure that reflects the biological effects of different radiations. It is measured in sieverts (Sv).
Effective Dose
The effective dose further adjusts the equivalent dose by considering the varying sensitivities of different tissues to radiation. This provides a holistic assessment of the potential biological harm from radiation exposure.
Methods of Dose Calculation
Direct Measurement
Direct measurement of radiation dose can be performed using dosimeters, which are devices that measure the absorbed dose in real-time. Common types include thermoluminescent dosimeters (TLDs) and optically stimulated luminescent dosimeters (OSLDs).
Computational Modelling
Computational methods involve using mathematical models and simulations to estimate the dose distribution within the body. Monte Carlo simulations are widely used because they accurately model the complex interactions of radiation with matter.
Biokinetic Modelling
Biokinetic models describe the behaviour of radiopharmaceuticals within the body, predicting their distribution and clearance over time. These models are crucial for calculating the absorbed dose to various organs and tissues.
Advances in Imaging and Software Tools
Positron Emission Tomography (PET)
PET imaging is instrumental in visualising the distribution of radiopharmaceuticals within the body. This imaging modality provides high-resolution, three-dimensional images that are essential for accurate dose calculation.
Single Photon Emission Computed Tomography (SPECT)
SPECT imaging, similar to PET, provides detailed information on the spatial distribution of radiopharmaceuticals. It is particularly useful for dosimetry in radionuclide therapy involving gamma-emitting isotopes.
Hybrid Imaging Techniques
Hybrid imaging systems, such as PET/CT and SPECT/CT, combine functional and anatomical imaging, providing comprehensive data for precise dosimetry.
Dosimetry Software
Advanced software tools have been developed to facilitate dose calculation and planning. These programs integrate imaging data, biokinetic models, and computational algorithms to provide accurate and personalised dosimetry.
Clinical Applications of Dosimetry in Radionuclide Therapy
Thyroid Cancer
Dosimetry is critical in the treatment of thyroid cancer using radioactive iodine (I-131). Accurate dosimetry ensures the optimal dose is delivered to the thyroid tissue while minimising exposure to other organs.
Neuroendocrine Tumours
Radionuclide therapy with Lutetium-177 (Lu-177) and Yttrium-90 (Y-90) is commonly used for neuroendocrine tumours. Dosimetry helps tailor the treatment to maximise tumour control and minimise side effects.
Prostate Cancer
Radium-223 (Ra-223) therapy for metastatic prostate cancer relies on dosimetry to deliver effective treatment doses to bone metastases, improving patient outcomes.
Challenges in Dosimetry
Heterogeneous Dose Distribution
One of the significant challenges in dosimetry is accounting for the heterogeneous distribution of radiopharmaceuticals within the body. Tumours and normal tissues may receive varying doses, complicating dose calculations and optimisation.
Patient-Specific Variability
Individual differences in anatomy, physiology, and radiopharmaceutical uptake can lead to significant variability in dose distribution. Personalised dosimetry is essential to address these variations and ensure optimal treatment for each patient.
Technological Limitations
While advancements in imaging and software have improved dosimetry, technological limitations can still impact accuracy. Ensuring high-quality imaging and precise modelling is crucial for effective dosimetry.
Future Directions in Dosimetry
Personalised Medicine
The trend towards personalised medicine is driving advancements in dosimetry. By tailoring treatment plans to individual patient characteristics, personalised dosimetry aims to enhance the efficacy and safety of radionuclide therapy.
Artificial Intelligence and Machine Learning
Artificial intelligence (AI) and machine learning (ML) are increasingly being integrated into dosimetry. These technologies can analyse large datasets, improve predictive models, and optimise treatment planning.
Advanced Imaging Techniques
Ongoing developments in imaging technology are expected to enhance dosimetry further. Innovations such as high-resolution PET and SPECT and new imaging agents will provide more precise and detailed information for dose calculation.
Radiobiological Modelling
Incorporating radiobiological models into dosimetry can improve understanding of radiation effects at the cellular and molecular levels. This knowledge can be used to refine dose calculations and optimise treatment outcomes.
Conclusion
Dosimetry in radionuclide therapy is a dynamic and essential field that underpins treatment effectiveness and safety. By accurately measuring and calculating radiation doses; dosimetry ensures that therapeutic goals are achieved while minimising harm to healthy tissues. As technology and methodologies continue to advance, dosimetry will play an increasingly critical role in the personalised treatment of cancer and other diseases, ultimately improving patient outcomes.
Disclaimer
The content of this article is intended for informational and educational purposes only and does not constitute medical advice, diagnosis, or treatment recommendations. While every effort has been made to ensure the accuracy and currency of the information presented, Open Medscience does not guarantee its completeness or applicability to individual cases. Readers should consult a qualified healthcare professional before making decisions related to radionuclide therapy, dosimetry, or any medical treatment. The views expressed in this article are those of the author(s) and do not necessarily reflect the position of Open Medscience or its affiliates.