Radiotheranostics, a revolutionary approach combining diagnostics and therapeutic radiology, is transforming the landscape of personalised medicine. This article looks into the various types of radiotheranostic treatments, outlining how these innovative techniques are being used for precise cancer diagnosis and treatment. From radionuclide-based therapies to advanced PET/CT diagnostics, we explore the mechanisms, applications, and future potential of radiotheranostics in the clinical setting.
Introduction to Radiotheranostics
Radiotheranostics is an emerging field that combines diagnostics with therapeutic applications in nuclear medicine. This dual-purpose approach enables doctors to not only diagnose cancer but also treat it using the same radiopharmaceutical agents. The term “theranostics” is derived from the combination of “therapy” and “diagnostics”, and it represents a personalised approach to treatment by targeting specific biological markers associated with disease.
Radiotheranostics primarily utilises radioactive isotopes attached to targeting molecules, such as antibodies or peptides, which can identify specific cancer cells. Once the diagnostic part confirms the tumour’s location, the therapeutic component delivers radiation directly to the tumour site, sparing healthy tissues. This strategy offers an effective and targeted treatment, minimising side effects compared to traditional chemotherapy or radiotherapy.
Types of Radiotheranostic Treatments
Radiotheranostics comprises various techniques and treatment modalities, each tailored to specific cancers and patient needs. Below are the main types of radiotheranostic treatments currently in clinical use or under research.
Peptide Receptor Radionuclide Therapy (PRRT)
Peptide Receptor Radionuclide Therapy (PRRT) is a type of molecular therapy used primarily for neuroendocrine tumours (NETs). This treatment relies on radiolabelled peptides, such as octreotide or octreotate, that bind to specific receptors expressed on tumour cells.
The peptides are conjugated with radioactive isotopes such as Lutetium-177 (177Lu) or Yttrium-90 (90Y). These isotopes emit beta radiation, which causes DNA damage in the tumour cells, leading to cell death. The radiolabelled peptides are administered intravenously and circulate in the bloodstream until they bind to their target receptors on cancer cells. Once attached, the radiation is delivered precisely to the tumour site.
PRRT has shown considerable success in improving progression-free survival in patients with NETs, making it a significant advancement in personalised cancer treatment.
Radioimmunotherapy (RIT)
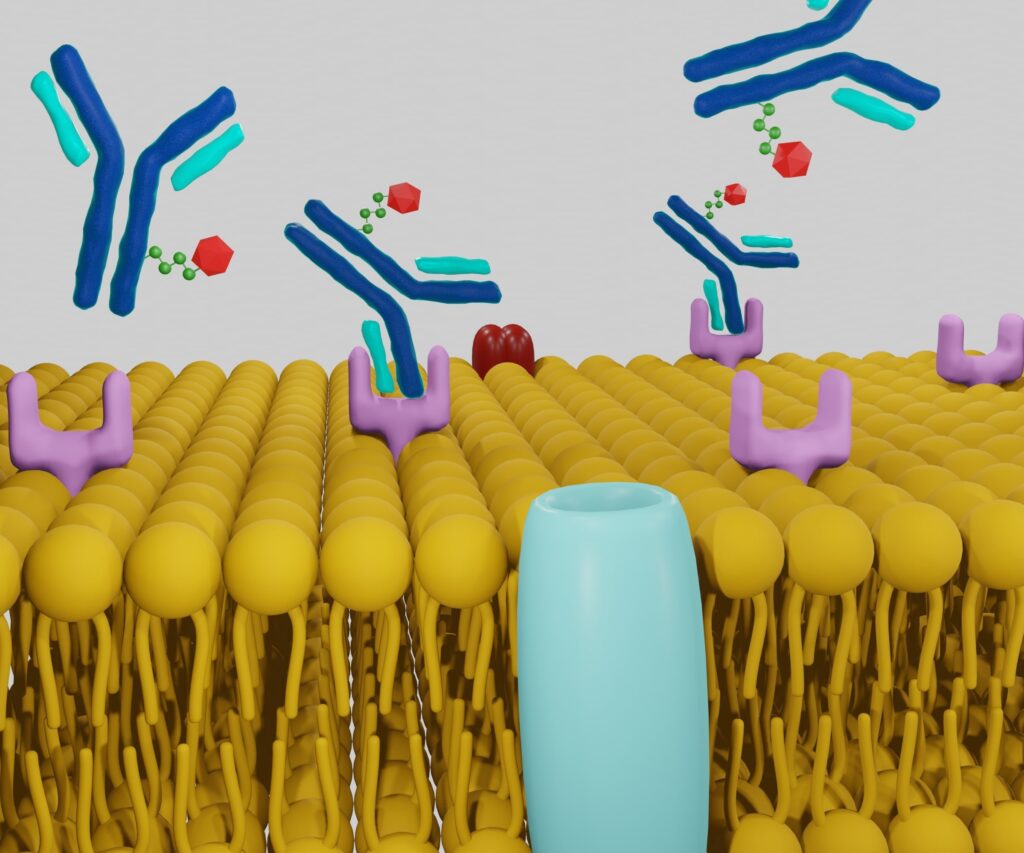
Radioimmunotherapy (RIT) combines the specificity of monoclonal antibodies with the cell-killing power of radiation. In this therapy, antibodies are designed to target specific antigens expressed on the surface of tumour cells. These antibodies are conjugated with a radioactive isotope, such as Iodine-131 (131I) or Yttrium-90 (90Y).
Once injected into the patient, the radiolabelled antibody binds to its target antigen, delivering radiation directly to the cancer cells. This localised approach reduces damage to surrounding healthy tissues and increases the effectiveness of the therapy.
RIT has been successfully used to treat certain types of non-Hodgkin lymphoma, especially in cases where traditional chemotherapy and radiation therapy have failed. For example, the radiopharmaceutical agent Zevalin (Ibritumomab tiuxetan) is approved for treating relapsed or refractory lymphoma.
Radionuclide Therapy
Radionuclide therapy involves the use of radioactive isotopes that are introduced into the body to target specific tumours. These isotopes either circulate systemically or are injected directly into a tumour, depending on the type of cancer.
- Iodine-131 Therapy: One of the most well-known forms of radionuclide therapy is Iodine-131 (131I) treatment for thyroid cancer and hyperthyroidism. Iodine-131 is selectively taken up by thyroid cells, and its beta radiation destroys cancerous thyroid tissue with minimal impact on the rest of the body.
- Radium-223 Therapy: Another example is Radium-223 (223Ra) therapy, which is used for treating bone metastases, especially in prostate cancer. Radium-223 mimics calcium and is absorbed into bone tissue, where it emits alpha radiation that kills cancer cells without causing significant damage to surrounding healthy tissue.
Radionuclide therapy is an effective treatment for cancers that have metastasised, particularly those that spread to bones or specific organs, and it often leads to improved survival rates and quality of life for patients.
Prostate-Specific Membrane Antigen (PSMA) Radiotherapy
Prostate-specific membrane antigen (PSMA) is a protein found on the surface of prostate cancer cells, making it an ideal target for radiotheranostic applications. PSMA radiotherapy is designed for advanced prostate cancer patients who no longer respond to standard therapies.
The treatment involves using a PSMA-targeted molecule that is labelled with a radioactive isotope, such as Lutetium-177 (177Lu) or Actinium-225 (225Ac). The radiopharmaceutical binds specifically to the PSMA-expressing tumour cells, allowing for highly targeted radiation therapy.
PSMA radiotherapy has shown great promise in treating castration-resistant prostate cancer, often reducing tumour size and improving patient outcomes. Its diagnostic counterpart, PSMA PET/CT imaging, is also used to accurately locate and stage prostate cancer before initiating treatment.
Theranostic Nanoparticles
The development of nanoparticles as radiotheranostic agents is a growing area of research. Nanoparticles can be engineered to carry both diagnostic and therapeutic agents, offering a multimodal platform for cancer treatment.
These nanoparticles are typically loaded with a radionuclide for imaging purposes (e.g., technetium-99m for SPECT or fluorine-18 for PET scans) and a therapeutic payload (e.g., Lutetium-177 or Yttrium-90). The small size of the nanoparticles allows them to penetrate deep into tumour tissues and deliver their payload with high precision.
Theranostic nanoparticles hold promise for treating a wide range of cancers, including those that are difficult to treat with conventional methods. Ongoing research aims to improve the targeting specificity, imaging clarity, and therapeutic effectiveness of these nanoparticles.
SPECT and PET Imaging-Guided Therapy
Single Photon Emission Computed Tomography (SPECT) and Positron Emission Tomography (PET) are essential imaging tools used in radiotheranostics. These imaging modalities help identify the location and extent of cancer before, during, and after treatment.
- PET Imaging: PET imaging uses radioactive tracers, such as fluorine-18 (18F), to visualise cancerous tissues in the body. The information from a PET scan helps oncologists decide whether the patient is a candidate for a specific type of radionuclide therapy. For instance, in PSMA radiotherapy, PSMA PET imaging is often performed first to determine the extent of the tumour burden.
- SPECT Imaging: SPECT imaging provides 3D images of how radiopharmaceuticals distribute throughout the body. It is particularly useful in planning radiotheranostic treatments by showing how effectively a radiopharmaceutical targets the tumour. SPECT is frequently used alongside radionuclide therapies like Iodine-131 and Lutetium-177.
Both imaging techniques allow for real-time monitoring of treatment progress, making adjustments to the therapy as needed to improve patient outcomes.
Benefits of Radiotheranostic Treatments
The advantages of radiotheranostic treatments are numerous and align with the growing emphasis on personalised medicine. By combining diagnosis and treatment in a single procedure, radiotheranostics offers several benefits:
Personalised and Targeted Therapy
Radiotheranostic treatments are highly specific to individual patients, targeting unique biomarkers expressed by their cancer cells. This level of precision minimises damage to healthy tissue and maximises the therapeutic effect on tumours.
Minimised Side Effects
Traditional cancer treatments, such as chemotherapy and external beam radiation therapy, can cause widespread damage to healthy tissues, leading to severe side effects. Radiotheranostics significantly reduces these side effects by delivering radiation directly to the tumour site.
Improved Treatment Monitoring
With the use of SPECT and PET imaging, oncologists can closely monitor the effectiveness of the treatment. This allows for timely adjustments, ensuring that the treatment is as effective as possible while minimising unnecessary exposure to radiation.
Potential for Early Diagnosis
In some cases, radiotheranostic techniques can detect cancer at earlier stages than other imaging modalities. Early diagnosis often leads to better treatment outcomes and higher survival rates.
Combination with Other Therapies
Radiotheranostics can be combined with other treatment modalities, such as surgery, chemotherapy, and immunotherapy, to create a comprehensive treatment plan tailored to the patient’s specific needs.
Limitations and Challenges
While radiotheranostic treatments offer many advantages, there are also several limitations and challenges that need to be addressed:
Limited Availability
Radiotheranostic treatments are not widely available in all regions, primarily due to the high cost of radiopharmaceuticals and the need for specialised equipment and facilities.
Radiopharmaceutical Supply Chain
The production and distribution of radiopharmaceuticals are complex, and ensuring a consistent supply can be challenging. Radioisotopes often have short half-lives, necessitating timely production and delivery.
Patient Selection
Not all patients are candidates for radiotheranostic treatments. The success of these therapies depends on the expression of specific biomarkers, and in some cases, cancer cells may not express the necessary targets for the therapy to be effective.
Future Directions in Radiotheranostics
As research into radiotheranostic treatments continues, several promising developments are on the horizon:
New Radiopharmaceuticals
The discovery of new radioisotopes and targeting molecules is expanding the range of cancers that can be treated with radiotheranostics. For instance, alpha-emitting isotopes like Actinium-225 are being explored for their ability to cause more localised and potent damage to cancer cells.
Immunotheranostics
Combining radiotheranostics with immunotherapy is a promising area of research. This approach could enhance the immune system’s ability to recognise and attack cancer cells, improving the overall effectiveness of treatment.
AI and Machine Learning
The integration of artificial intelligence and machine learning in radiotheranostics could lead to more accurate treatment planning and monitoring. AI algorithms may help identify patterns in imaging data that can predict patient outcomes and guide personalised treatment decisions.
Conclusion
Radiotheranostics represents a cutting-edge approach to cancer treatment, offering a personalised and targeted therapy option for many patients. By combining diagnostic imaging with radiopharmaceutical therapy, radiotheranostics provides a powerful tool for the diagnosis and treatment of cancer. While challenges remain, ongoing advancements in this field hold the promise of even more effective and widely available treatments in the future. Radiotheranostics is likely to play an increasingly important role in personalised medicine, improving outcomes for patients across a broad spectrum of cancers.
Disclaimer
The content provided in this article, “Radiotheranostic Treatments: A Guide to Types and Their Clinical Applications,” is intended for informational and educational purposes only. It does not constitute medical advice, diagnosis, or treatment, and should not be relied upon as a substitute for professional medical guidance.
While every effort has been made to ensure the accuracy of the information at the time of publication, Open Medscience makes no warranties or representations regarding its completeness or suitability for any particular purpose. Radiotheranostic treatments are complex medical procedures that should only be considered and administered under the supervision of qualified healthcare professionals.
Readers are strongly advised to consult their doctor, oncologist, or a qualified specialist before making any decisions related to diagnosis or treatment based on the content of this article. The mention of specific products, therapies, or medical devices does not imply endorsement or recommendation by Open Medscience.
Open Medscience disclaims any liability for any loss, injury, or damage incurred as a consequence, directly or indirectly, of the use or application of any information contained in this article.
home » blog » radiotheranostics »