Summary: Radiotheranostics, a rapidly advancing field in oncology, offers significant promise in treating prostate cancer through personalised diagnosis and therapy. Combining targeted radiotherapy with diagnostic imaging, radiotheranostics enables precise localisation, assessment, and treatment of prostate cancer lesions, including metastatic spread. This approach not only enhances the accuracy of treatment but also reduces the impact on surrounding healthy tissues. Recent advances, especially in prostate-specific membrane antigen (PSMA)-targeted radiopharmaceuticals, have demonstrated improved patient outcomes in advanced prostate cancer cases. This article explores the role of radiotheranostics in prostate cancer treatment, examining its mechanisms, benefits, challenges, and potential future developments.
Introduction to Prostate Cancer
Prostate cancer is one of the most prevalent cancers affecting men worldwide, with high morbidity and mortality rates in advanced stages. Traditional treatment options, such as surgery, chemotherapy, and external beam radiation therapy, have limitations in terms of efficacy, side effects, and patient-specific outcomes. Radiotheranostics, an emerging approach in nuclear medicine, holds transformative potential in treating prostate cancer. This method integrates diagnostic and therapeutic capabilities, allowing clinicians to precisely target cancerous cells and deliver treatment while monitoring progress.
Understanding Radiotheranostics
Radiotheranostics combines two core components: diagnostic imaging and targeted radionuclide therapy. This fusion of therapy and diagnostics enables the detection and treatment of cancer cells based on molecular characteristics rather than solely anatomical features.
Diagnostic Component: Imaging
The diagnostic aspect of radiotheranostics involves the use of imaging agents tagged with radioactive isotopes that emit positrons or gamma rays, detectable through positron emission tomography (PET) or single-photon emission computed tomography (SPECT). These radiopharmaceuticals target specific receptors or antigens on cancer cells, such as the prostate-specific membrane antigen (PSMA), which is highly expressed in prostate cancer. By visualising these molecular markers, clinicians can obtain a highly accurate map of cancerous tissue distribution, even in metastatic cases.
Therapeutic Component: Targeted Radionuclide Therapy
The therapeutic side of radiotheranostics involves administering a therapeutic radiopharmaceutical that targets cancer cells while emitting cytotoxic radiation. In prostate cancer, beta- or alpha-emitting isotopes attached to ligands specific for PSMA are common. When administered to the patient, these radiopharmaceuticals bind to the cancer cells, releasing radiation that damages cancerous tissue. This approach limits the damage to healthy tissues, as the radiation is delivered with high specificity to malignant cells.
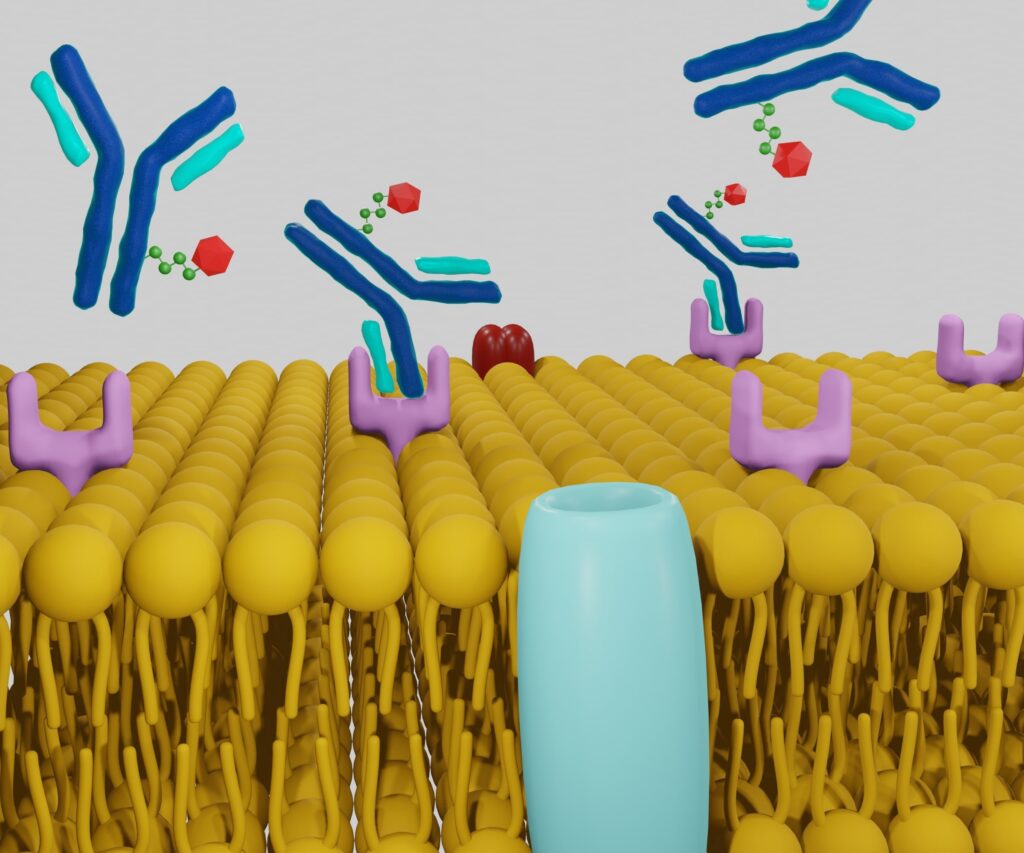
The Role of Prostate-Specific Membrane Antigen (PSMA) in Radiotheranostics
PSMA is a transmembrane protein found in high levels in prostate cancer cells, making it an ideal target for radiotheranostic applications. PSMA expression increases with the progression and metastatic spread of prostate cancer, further amplifying its potential for effective targeting in advanced cases.
PSMA-Based Imaging
The introduction of PSMA-targeted PET imaging has revolutionised prostate cancer diagnostics. PSMA-targeted imaging agents, such as 68Ga-PSMA and 18F-PSMA, provide a clear and accurate depiction of cancerous lesions by binding to PSMA receptors in prostate cancer cells. This enables the identification of metastatic disease that may not be visible through conventional imaging methods, such as MRI or CT scans.
PSMA-Directed Radiotherapy
Therapeutic PSMA-targeting radiopharmaceuticals, such as Lutetium-177-PSMA (177Lu-PSMA), have shown promising results in treating advanced prostate cancer. 177Lu-PSMA binds selectively to PSMA receptors, delivering beta radiation directly to cancer cells, which leads to DNA damage and cell death. The high specificity of PSMA-targeted radiotherapy minimises collateral damage to surrounding healthy tissues, reducing side effects compared to systemic chemotherapy.
Benefits of Radiotheranostics in Prostate Cancer Treatment
Radiotheranostics offers several unique advantages for prostate cancer patients, particularly those with advanced or metastatic disease. These benefits include precision, personalised treatment, reduced side effects, and potential for repeat therapy.
Precision and Accuracy
One of the most notable advantages of radiotheranostics is its precision in detecting and treating prostate cancer cells. The ability to visualise PSMA expression levels across different tissues allows clinicians to customise the treatment approach for individual patients. Furthermore, precise targeting reduces the impact on surrounding organs, such as the bladder and rectum, thereby preserving their function and enhancing the patient’s quality of life.
Personalised Therapy
Radiotheranostics allows for a personalised approach, as the therapy is based on the molecular characteristics of the tumour. By evaluating PSMA expression levels, clinicians can identify patients who are likely to respond favourably to radiotheranostic treatment, optimising therapeutic outcomes.
Reduced Side Effects
Traditional treatments for advanced prostate cancer, such as chemotherapy, are associated with significant side effects, including fatigue, nausea, and a weakened immune system. Radiotheranostics, in contrast, delivers radiation directly to cancer cells, minimising exposure to healthy tissue and thus reducing these adverse effects.
Feasibility of Repeat Therapy
Radiotheranostics treatments, particularly PSMA-targeted therapies, may be administered multiple times if cancer recurs or progresses. This flexibility is beneficial in advanced prostate cancer, where continuous management is often required.
Radiotheranostics in Advanced Prostate Cancer: Clinical Evidence
Numerous studies have demonstrated the efficacy of radiotheranostics in managing advanced prostate cancer. Clinical trials involving 177Lu-PSMA have shown notable improvements in progression-free survival and overall survival rates. A landmark trial, the VISION study, evaluated the efficacy of 177Lu-PSMA-617 in metastatic castration-resistant prostate cancer patients. Results indicated that patients receiving 177Lu-PSMA-617 alongside standard care experienced significant delays in disease progression and extended overall survival compared to those receiving standard care alone.
The success of these trials has spurred regulatory approvals in several countries, making 177Lu-PSMA a valuable therapeutic option for advanced prostate cancer patients who have exhausted other treatment lines.
Challenges in Radiotheranostics for Prostate Cancer
Despite the promising outcomes, the implementation of radiotheranostics in prostate cancer treatment presents certain challenges.
Limited Access and Infrastructure
Radiotheranostics requires access to advanced nuclear medicine facilities, including PET scanners, cyclotrons for producing radionuclides, and specialised radiation safety measures. In regions with limited nuclear medicine infrastructure, access to radiotheranostic treatments may be challenging, affecting patient outcomes and limiting the widespread adoption of this approach.
Potential Side Effects and Toxicity
Although radiotheranostics reduce systemic side effects compared to chemotherapy, it is not entirely without risk. Some patients may experience haematologic toxicity, kidney damage, or mild radiation-induced side effects. Continuous monitoring is essential to ensure that the therapeutic benefits outweigh these potential risks.
Patient Selection and PSMA Expression
PSMA expression levels vary among prostate cancer patients, and some tumours may lack sufficient PSMA expression to benefit from PSMA-targeted radiotherapy. Accurate assessment of PSMA expression through PET imaging is crucial in selecting patients who are likely to respond to treatment, but not all patients will be eligible.
Future Directions in Radiotheranostics for Prostate Cancer
Research into radiotheranostics is progressing rapidly, with several potential developments on the horizon that could improve outcomes for prostate cancer patients further.
Development of Alpha-Emitting Radiopharmaceuticals
While beta-emitting radiopharmaceuticals like 177Lu-PSMA have shown efficacy, alpha-emitting isotopes such as Actinium-225 (225Ac) offer even greater cell-killing potential due to their high-energy emission. Alpha particles have a shorter path length, which may further reduce damage to nearby healthy tissues. Early studies involving 225Ac-PSMA have shown promising results, particularly in patients who have not responded to beta-emitting therapies.
Combination Therapies
Combining radiotheranostics with other treatment modalities, such as immunotherapy or hormone therapy, is an area of active research. By pairing radiotheranostic treatment with drugs that stimulate the immune response, researchers aim to enhance the body’s natural ability to fight prostate cancer, potentially leading to more durable responses.
Broadening Target Molecules
While PSMA is a well-validated target, additional targets are under investigation to expand the patient population that could benefit from radiotheranostics. Other molecular targets, such as gastrin-releasing peptide receptors (GRPRs), are being explored to develop new imaging agents and therapies for prostate cancer.
Enhancing Imaging Techniques
Advances in imaging technology, such as digital PET and hybrid PET/MRI, are improving the sensitivity and accuracy of tumour detection. Enhanced imaging techniques will enable clinicians to identify smaller metastatic lesions, facilitating earlier intervention and more tailored treatment planning.
Conclusion
Radiotheranostics represents a paradigm shift in prostate cancer treatment, offering a personalised approach that combines targeted imaging and therapy. By focusing on molecular targets such as PSMA, radiotheranostics provides accurate localisation and selective eradication of cancerous cells while minimising side effects. Recent studies and clinical trials have validated its efficacy in advanced prostate cancer, with ongoing research poised to expand its applications and enhance its effectiveness further.
As radiotheranostics continues to evolve, challenges such as accessibility, toxicity, and patient selection must be addressed to ensure the broadest possible benefit. The future of radiotheranostics in prostate cancer is promising, with potential breakthroughs in alpha-emitting therapies, combination treatments, and new molecular targets on the horizon. For prostate cancer patients, particularly those with advanced or metastatic disease, radiotheranostics offers hope for improved survival rates, enhanced quality of life, and a new level of precision in treatment.
Disclaimer
The information provided in this article, Radiotheranostics in Prostate Cancer: A New Frontier in Precision Treatment, is intended for educational and informational purposes only and does not constitute medical advice, diagnosis, or treatment. While every effort has been made to ensure the accuracy of the content, Open Medscience does not guarantee that the information is current, complete, or applicable to individual medical cases.
Readers should not rely solely on this article to make decisions about medical care or treatment options. Always consult a qualified healthcare professional or specialist for personalised advice and to discuss any medical concerns or conditions. The inclusion of specific radiopharmaceuticals or treatment protocols does not imply endorsement or recommendation by Open Medscience or its contributors.
Open Medscience and the authors accept no responsibility for any loss, injury, or harm incurred as a result of using the information presented in this article.
home » blog » radiotheranostics »