Radiotheranostics is an emerging field at the intersection of diagnostics and therapeutics, offering a highly promising approach in precision medicine. By combining targeted diagnosis with personalised treatment, it addresses many limitations of traditional cancer care. As technology and molecular biology advance, radiotheranostics is expected to revolutionise how clinicians treat various malignancies, improving patient outcomes and minimising side effects. This article explores the key developments, challenges, and future directions of radiotheranostics. It highlights how advancements in imaging, radiopharmaceuticals, artificial intelligence, and regulatory frameworks are shaping this new frontier of medicine.
Advancements in Imaging Techniques
The concept of radiotheranostics represents a novel and transformative approach to medicine, particularly in cancer treatment. It merges two traditionally separate areas: radiotherapy, which involves the use of radiation to treat disease, and diagnostic imaging, which helps in identifying diseases. The idea behind radiotheranostics is simple yet revolutionary—using the same molecule for both diagnosis and treatment. This allows for precise targeting of cancer cells, reducing damage to healthy tissue and enhancing treatment efficacy. As we move forward, the future of radiotheranostics looks incredibly promising, with rapid advancements in technology, medicine, and bioengineering. However, challenges remain in terms of cost, regulation, and integration into mainstream healthcare systems.
Molecular Imaging
One of the most significant developments driving the future of radiotheranostics is molecular imaging. Traditional imaging modalities, such as CT and MRI, are limited in their ability to provide detailed information about the biological and molecular characteristics of a tumour. Molecular imaging goes beyond this by visualising cellular processes and pathways, enabling clinicians to identify tumour-specific biomarkers.
Positron emission tomography (PET) combined with computed tomography (CT), known as PET/CT, is a leading technology in radiotheranostics. This hybrid modality provides real-time data on both the structure and metabolic activity of tumours. Future imaging technologies will likely build upon PET/CT’s strengths, providing higher-resolution images and improved contrast agents to better detect early-stage cancers. Additionally, the advent of artificial intelligence (AI) in medical imaging could enhance diagnostic accuracy by automating image analysis and identifying patterns that might elude human observers.
Theranostic Imaging Agents
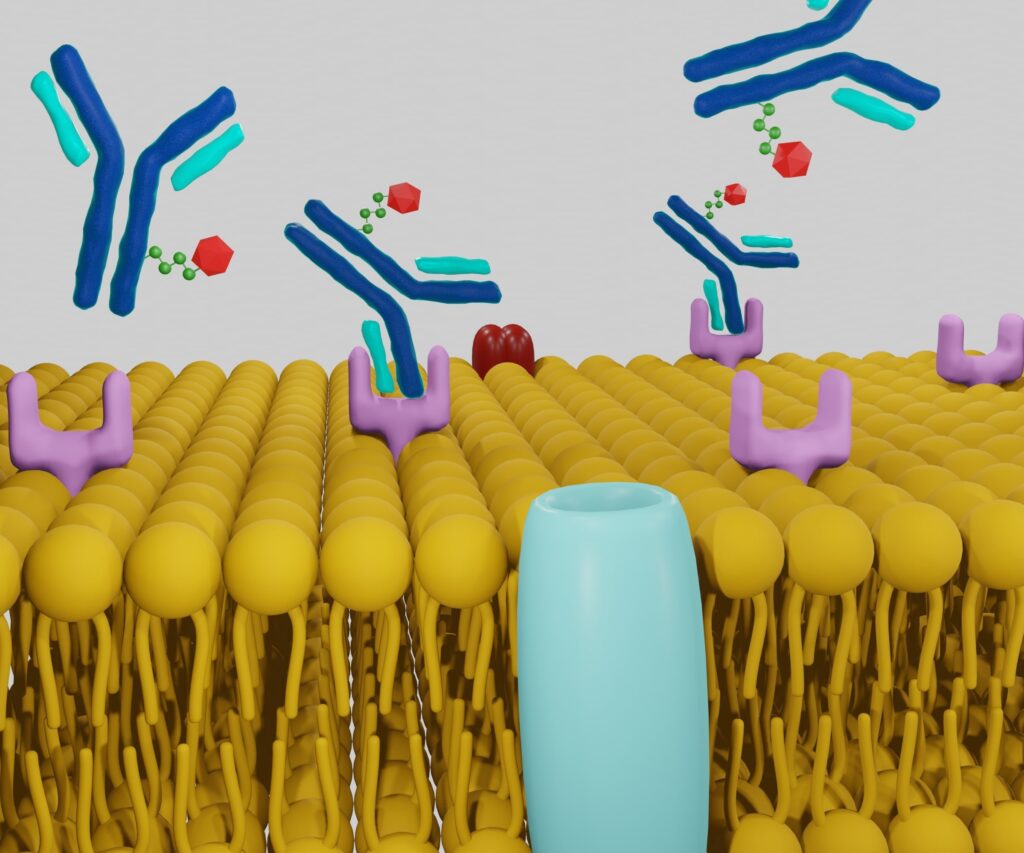
Another key advancement in the future of radiotheranostics is the development of theranostic imaging agents—molecules that combine both diagnostic and therapeutic functions. These agents are designed to selectively target cancer cells and are labelled with both diagnostic and therapeutic radioisotopes. For instance, gallium-68 (Ga-68) can be used for PET imaging, while lutetium-177 (Lu-177) can provide therapeutic radiation. These agents offer real-time monitoring of treatment response, allowing clinicians to adjust treatment plans dynamically.
Looking forward, more innovative theranostic agents are expected to be developed, which will provide greater specificity for a wider range of cancers. The integration of nanotechnology is also on the horizon, allowing for the design of multifunctional nanoparticles capable of delivering both imaging and therapeutic payloads with remarkable precision.
Radiopharmaceuticals and Targeted Therapy
At the core of radiotheranostics are radiopharmaceuticals—radioactive compounds used for diagnosis or treatment. The future of radiopharmaceuticals is closely linked to advances in chemistry and molecular biology, enabling more sophisticated methods of targeting cancer cells. Radiopharmaceuticals can bind to specific proteins or receptors found only on cancer cells, thereby sparing healthy tissue and reducing side effects.
Therapeutic radiopharmaceuticals emit beta or alpha particles that destroy cancer cells from within. With advances in radiochemistry, newer and more effective radiopharmaceuticals are being developed, which can be more easily targeted to specific tumour types. Innovations in this area, including novel ligands and peptides, are likely to broaden the application of radiotheranostics across various types of cancer and other diseases.
Alpha Emitters and Beta Emitters
The future of radiotheranostics will see significant advancements in the types of emitters used in therapy. Traditionally, beta emitters like lutetium-177 (Lu-177) have been employed due to their ability to travel a certain distance, which allows them to target larger areas within a tumour. However, alpha emitters such as actinium-225 (Ac-225) are gaining traction because they deliver high-energy radiation over very short distances, thereby offering highly localised treatment with minimal damage to surrounding tissues.
The increased use of alpha emitters in radiotheranostics presents exciting possibilities, particularly in treating cancers that are difficult to target with conventional therapies. As research progresses, alpha emitters are expected to become more widely available and applicable across a broader range of tumours.
Combination Therapies
As the field of radiotheranostics continues to evolve, combination therapies are expected to become a standard approach to treatment. This involves using radiopharmaceuticals in conjunction with other treatment modalities, such as immunotherapy or chemotherapy. The combination of different therapies could enhance the overall effectiveness of treatment, targeting multiple pathways simultaneously and reducing the likelihood of resistance.
For example, combining immune checkpoint inhibitors with radiotheranostics could help to boost the immune system’s response to cancer cells. Ongoing clinical trials are already exploring these synergies, and future research will undoubtedly expand the range of combination strategies available to clinicians.
Artificial Intelligence and Machine Learning in Radiotheranostics
Artificial intelligence (AI) and machine learning (ML) are poised to play an increasingly important role in the future of radiotheranostics. AI-powered algorithms can process vast amounts of imaging and clinical data, identifying patterns that can help predict how a patient’s disease will progress and how they might respond to treatment.
For instance, AI can be integrated into PET/CT imaging systems to analyse tumour characteristics with greater precision. These technologies will improve diagnostic accuracy, reduce the time it takes to interpret imaging results, and aid in personalising treatment plans for each patient. In the future, AI could even be used to develop virtual models of tumours, which would allow doctors to simulate the effects of different treatment options and select the most effective one for each patient.
Machine Learning for Predicting Treatment Outcomes
Machine learning (ML) is another area of AI that holds significant promise for the future of radiotheranostics. ML algorithms can analyse large datasets from previous radiotheranostic treatments, learning from past successes and failures to predict the likely outcomes of new cases. This capability could be particularly useful in complex cases where traditional treatment protocols may not provide the best outcomes.
For example, ML could help to identify biomarkers that predict a patient’s likelihood of responding to a specific radiopharmaceutical. This would allow for even more personalised treatment plans, ensuring that patients receive the therapy most likely to succeed in their unique situation.
Clinical Trials and Regulatory Challenges
Radiotheranostics is still an emerging field, and many of its technologies are currently undergoing rigorous testing in clinical trials. These trials are essential for ensuring the safety and efficacy of new radiopharmaceuticals and imaging agents. Some promising areas of investigation include prostate cancer, neuroendocrine tumours, and haematological malignancies, where radiotheranostics has shown early success.
The future of clinical trials in this field will likely focus on expanding the applications of radiotheranostics beyond cancer, exploring its potential in treating autoimmune diseases, cardiovascular conditions, and other chronic illnesses. Additionally, trials will seek to refine dosage and administration protocols to further reduce side effects and enhance patient outcomes.
Regulatory Considerations and Safety Concerns
As with any new medical technology, radiotheranostics faces several regulatory hurdles. The use of radioactive materials in treatment requires stringent safety protocols to protect both patients and healthcare providers. Regulatory bodies such as the European Medicines Agency (EMA) and the US Food and Drug Administration (FDA) will need to develop new frameworks that balance innovation with safety.
One of the challenges facing radiotheranostics is the standardisation of treatment protocols. Due to the personalised nature of these therapies, it can be difficult to create one-size-fits-all guidelines. Additionally, the long-term effects of some radiopharmaceuticals remain unclear, necessitating ongoing monitoring and research. Future regulatory efforts will need to address these challenges, ensuring that radiotheranostics can be safely integrated into mainstream clinical practice.
Cost and Accessibility
While the future of radiotheranostics holds great promise, one significant barrier to widespread adoption is cost. The development and production of radiopharmaceuticals, as well as the sophisticated imaging equipment required for diagnosis and treatment, can be prohibitively expensive. Additionally, the personalised nature of radiotheranostics means that each patient’s treatment plan may need to be custom-tailored, further increasing costs.
To make radiotheranostics more accessible, it will be essential to develop cost-effective methods of production and distribution. Governments and healthcare providers will also need to consider how to fund these therapies, ensuring that patients from all economic backgrounds can benefit from these cutting-edge treatments.
Improving Accessibility in Low-Resource Settings
A key challenge for the future of radiotheranostics will be ensuring that it is accessible to patients in low-resource settings. Many countries lack the infrastructure necessary to support advanced imaging technologies and radiopharmaceutical production. Addressing these disparities will require international cooperation, with wealthier nations and global organisations working together to expand access to these life-saving treatments.
One potential solution lies in the development of portable and affordable imaging devices, as well as radiopharmaceuticals that are easier and cheaper to produce. Additionally, telemedicine and AI-powered diagnostic tools could help to bring radiotheranostics to remote or underserved areas.
Ethical Considerations
The personalised nature of radiotheranostics raises important ethical questions, particularly regarding informed consent and patient autonomy. Because these therapies are highly experimental and involve the use of radioactive materials, it is essential that patients fully understand the risks and benefits before agreeing to treatment.
In the future, ensuring that patients have access to clear and comprehensive information will be crucial. Healthcare providers will need to engage in transparent discussions with patients, explaining not only the potential outcomes but also the long-term risks and uncertainties associated with radiotheranostic treatments.
Equity and Fairness
As with any new medical technology, there is a risk that radiotheranostics could exacerbate existing inequalities in healthcare. Wealthier patients or those living in well-resourced regions may have access to the latest treatments, while others are left behind. It will be important for policymakers to develop frameworks that ensure equitable access to radiotheranostics, regardless of a patient’s socioeconomic status or geographical location.
Conclusion
The future of radiotheranostics is promising, offering unprecedented opportunities for the precise diagnosis and treatment of a range of diseases, particularly cancer. Technological advancements in imaging, radiopharmaceutical development, and artificial intelligence are driving this field forward, promising to revolutionise precision medicine. However, challenges remain in terms of cost, regulatory hurdles, and ensuring equitable access to these cutting-edge therapies. As we look to the future, ongoing research and collaboration between clinicians, researchers, and policymakers will be essential in unlocking the full potential of radiotheranostics.
Q&A: The Future of Radiotheranostics
Q1: What is radiotheranostics?
A: Radiotheranostics is an innovative field that combines diagnostics and therapy, particularly for cancer treatment. It involves using the same molecule for both diagnosing and treating a disease, allowing clinicians to deliver highly targeted treatments while simultaneously monitoring the effectiveness of those treatments. The process typically involves using a radioactive substance to both detect cancer cells and treat them, improving precision and reducing side effects.
Q2: How does radiotheranostics differ from traditional cancer treatments?
A: Traditional cancer treatments like chemotherapy and external beam radiation often target both cancerous and healthy cells, leading to significant side effects. In contrast, radiotheranostics is far more targeted. It uses radiopharmaceuticals that bind specifically to cancer cells, delivering therapy directly to the tumour while minimising damage to surrounding healthy tissue. This approach offers a personalised treatment plan, reducing unnecessary harm and improving outcomes for patients.
Q3: What are some recent advancements in imaging techniques used in radiotheranostics?
A: Advances in molecular imaging, such as PET/CT, allow clinicians to visualise not just the structure of tumours but also their metabolic activity. Theranostic imaging agents, which combine diagnostic and therapeutic functions, are another breakthrough. These agents help detect cancer cells while simultaneously delivering treatment. Additionally, the use of artificial intelligence (AI) in imaging is improving diagnostic accuracy by automating image analysis and identifying patterns that human observers might miss.
Q4: What are radiopharmaceuticals, and why are they important in radiotheranostics?
A: Radiopharmaceuticals are compounds that carry radioactive isotopes used either for diagnostic imaging or treatment. In radiotheranostics, these substances are crucial because they allow for the targeting of cancer cells with great precision. Diagnostic radiopharmaceuticals help in visualising tumours, while therapeutic radiopharmaceuticals emit radiation that destroys cancer cells. Innovations in radiopharmaceuticals are expanding their applications to different types of cancers, offering more effective treatment options.
Q5: What types of emitters are used in radiotheranostics, and how do they work?
A: Radiotheranostics typically uses two types of radioactive emitters: beta emitters and alpha emitters. Beta emitters, such as lutetium-177 (Lu-177), deliver radiation over a certain distance, allowing them to target larger tumour areas. Alpha emitters, like actinium-225 (Ac-225), provide highly localised, high-energy radiation that is more precise, making them suitable for treating difficult-to-reach cancers while sparing healthy tissues. The future of radiotheranostics is likely to see increased use of alpha emitters for more precise treatments.
Q6: How is artificial intelligence (AI) contributing to the development of radiotheranostics?
A: AI plays a significant role in radiotheranostics by enhancing diagnostic accuracy and personalising treatment. AI algorithms can process large datasets of imaging and clinical data, identifying patterns that can predict disease progression and treatment response. AI is also helping to automate image analysis, reducing interpretation time and increasing precision. In the future, AI may allow doctors to simulate different treatment options, selecting the most effective one for each patient.
Q7: What are some of the regulatory and clinical challenges facing radiotheranostics?
A: One of the primary challenges is the regulation of radiopharmaceuticals, as they involve the use of radioactive materials that require strict safety protocols. Regulatory bodies must ensure these treatments are both safe and effective, which can slow down their approval process. Additionally, clinical trials are essential for establishing the efficacy of new radiopharmaceuticals, and these trials can take years. Standardising treatment protocols across different healthcare systems also poses a significant challenge due to the personalised nature of radiotheranostics.
Q8: What are the cost and accessibility concerns related to radiotheranostics?
A: Radiotheranostics is expensive, both in terms of developing and producing radiopharmaceuticals and acquiring the advanced imaging equipment required for diagnosis and treatment. The personalised nature of these therapies can further increase costs, potentially limiting accessibility for patients from lower-income backgrounds. Improving accessibility will require innovations in cost-effective production methods and potentially government-funded healthcare programmes to subsidise these treatments.
Q9: How can radiotheranostics be made more accessible in low-resource settings?
A: To improve accessibility in low-resource settings, it is essential to develop more affordable radiopharmaceuticals and imaging devices. Portable and less expensive imaging equipment could make it easier for clinicians in underserved areas to adopt radiotheranostic technologies. International collaboration and telemedicine can also help bridge the gap by enabling remote consultations and diagnoses. Governments and global health organisations will need to prioritise expanding access to these advanced treatments in economically disadvantaged regions.
Q10: What ethical considerations are associated with radiotheranostics?
A: One of the primary ethical concerns in radiotheranostics is ensuring informed consent, given the experimental nature of many of these treatments and their use of radioactive materials. Patients must fully understand the risks, benefits, and uncertainties involved before agreeing to treatment. Another concern is the potential for inequalities in access, where wealthier patients may benefit from these cutting-edge therapies while those in poorer regions or with fewer resources might not have the same opportunities.
Q11: What diseases beyond cancer might benefit from radiotheranostics in the future?
A: While radiotheranostics is currently focused primarily on cancer, there is potential for its application in other diseases. Research is exploring its use in treating autoimmune conditions, cardiovascular diseases, and certain neurological disorders. As the technology and understanding of disease-specific biomarkers improve, radiotheranostics could be used to deliver targeted treatments for a broader range of chronic illnesses.
Q12: What role does combination therapy play in the future of radiotheranostics?
A: Combination therapies, where radiopharmaceuticals are used alongside other treatments like immunotherapy or chemotherapy, are expected to become more common. By targeting multiple pathways simultaneously, combination therapies can improve treatment efficacy and reduce the likelihood of cancer cells developing resistance. Current clinical trials are exploring various combinations, and future research is likely to expand these strategies, offering more personalised and effective treatment options.
Q13: How might the use of machine learning improve treatment outcomes in radiotheranostics?
A: Machine learning (ML) can analyse large datasets from previous radiotheranostic treatments to predict treatment outcomes for new patients. This ability to learn from past successes and failures can help clinicians select the most effective treatments for each patient. For example, ML can identify biomarkers that indicate how likely a patient is to respond to a particular radiopharmaceutical, allowing for more personalised and precise treatment plans.
Q14: What does the future hold for radiotheranostics?
A: The future of radiotheranostics is full of promise. Technological advances in imaging, AI, radiopharmaceutical development, and personalised medicine are likely to revolutionise the field. More cancers and other diseases will be treatable using radiotheranostic methods, and treatments will become increasingly precise. However, challenges related to cost, regulation, and accessibility must be addressed to ensure these cutting-edge therapies are available to all patients who need them. Collaborative efforts between researchers, clinicians, and policymakers will be essential in unlocking the full potential of radiotheranostics.
Disclaimer
The content provided in this article is intended for informational and educational purposes only. Open Medscience does not offer medical advice, diagnosis, or treatment. Any opinions or views expressed are those of the author(s) and do not necessarily reflect those of Open Medscience or its affiliates.
While every effort has been made to ensure the accuracy and reliability of the information presented, radiotheranostics is an evolving area of research and clinical application. As such, some of the developments, treatments, or technologies discussed may still be under investigation or not yet widely available or approved for clinical use.
Readers should not use the information in this article as a substitute for professional medical advice or consultation with qualified healthcare providers. Always seek the guidance of a medical professional with any questions you may have regarding a medical condition or treatment options.
Open Medscience does not accept any responsibility for any loss, injury, or damage suffered by any individual as a result of reliance on the information provided in this article.
home » blog » radiotheranostics »