Summary: Radiology is increasingly being used in the treatment of drug addiction to support diagnosis, personalise therapies, and monitor recovery. Techniques such as MRI and PET scans provide valuable insight into how addiction affects the brain, allowing therapists to design more targeted interventions. Imaging can also motivate patients by showing visible progress and supporting the scientific understanding that addiction is a medical condition, not a moral failing.
Keywords: radiology; drug addiction; brain imaging; therapy; MRI; PET scan
Introduction
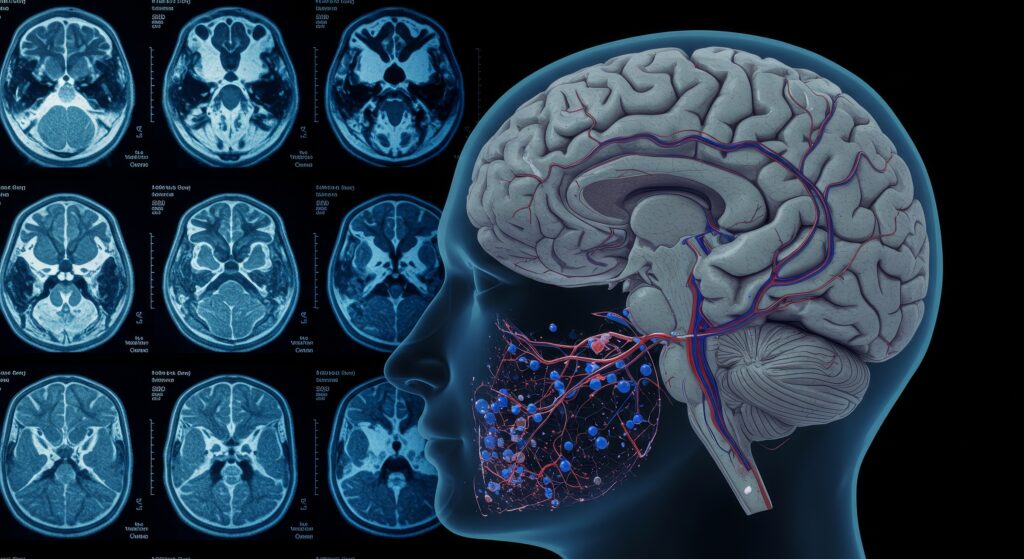
The treatment of drug addiction is evolving rapidly, with advances in medical imaging offering new tools to understand and manage the condition. Radiology, once confined to diagnostics in physical illnesses, is now being applied in therapeutic contexts for substance use disorders. Imaging technologies such as Magnetic Resonance Imaging (MRI) and Positron Emission Tomography (PET) are helping therapists develop more effective, personalised treatment plans and understand the neurological basis of addiction.
Addiction as a Neurological Disorder
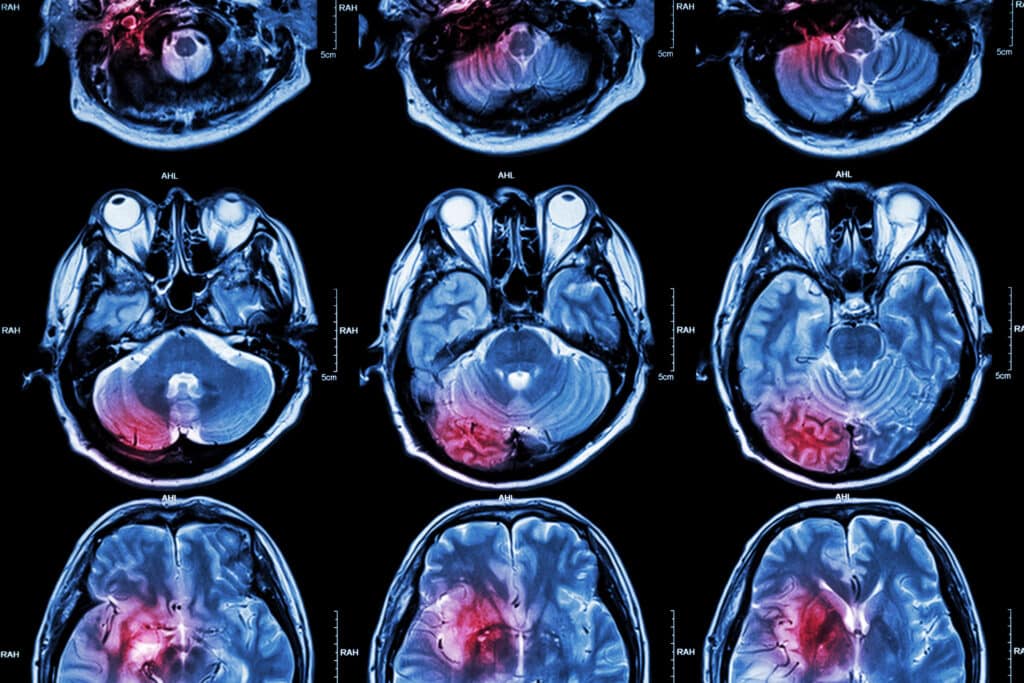
Addiction is no longer seen solely as a behavioural or social issue. Brain imaging has revealed that substance use alters key areas of the brain, particularly those involved in reward, motivation, memory, and decision-making. These findings, captured through radiological methods, have helped shift public and professional perceptions of addiction as a chronic neurological disorder. This scientific framework also helps reduce stigma, encouraging more individuals to seek treatment and commit to long-term recovery.
The Role of Imaging in Early Detection
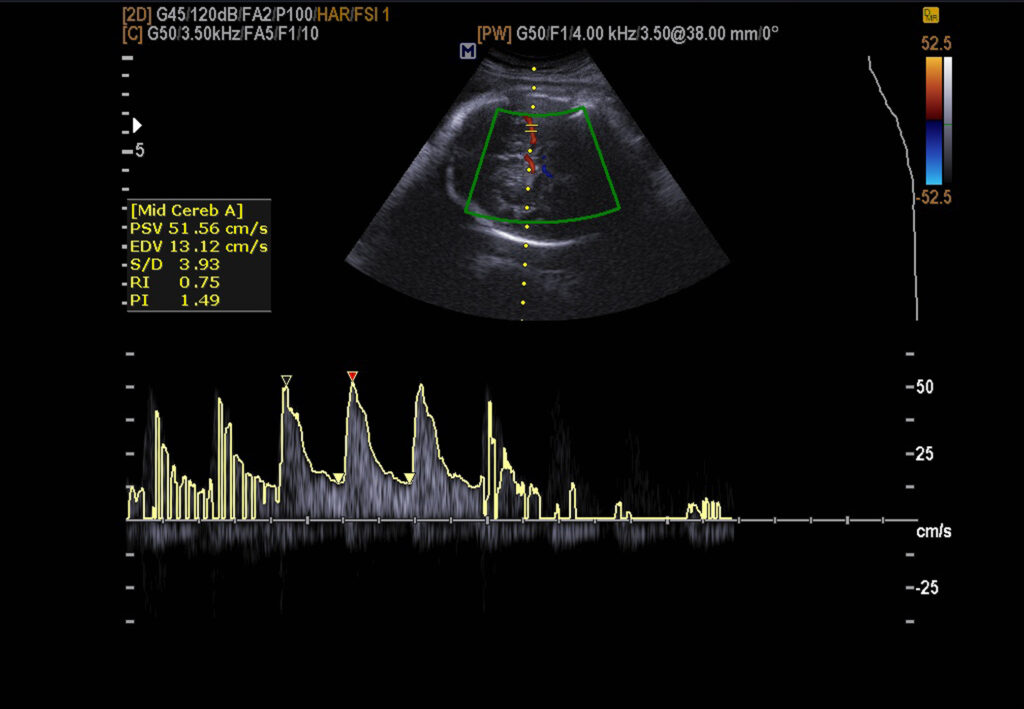
Radiological tools can detect early changes in brain activity linked to addiction, often before behavioural symptoms become evident. For example, PET scans can reveal fluctuations in dopamine transmission—one of the key chemical systems disrupted by addictive substances. Identifying these changes early enables timely interventions, which can lead to improved treatment outcomes. In high-risk individuals, this can also serve as a preventive strategy, supporting early-stage support before full-blown addiction develops.
Tailoring Treatment Using Brain Imaging
Radiology allows therapists to customise treatment according to the specific brain regions affected by substance use. For instance, if imaging reveals reduced activity in areas responsible for impulse control or emotional regulation, therapy can be directed towards addressing those functions more directly. This personalised approach increases the likelihood of successful outcomes, as treatment is no longer based solely on general patterns but on individual neurological data.
Moreover, radiological imaging can help monitor the effectiveness of medications within the brain, enabling clinicians to make more informed adjustments. This combination of imaging and clinical observation yields a more precise and responsive treatment plan.
Tracking Recovery and Reducing Relapse
Sustained recovery often requires ongoing assessment and support. Radiological imaging plays a crucial role in tracking brain changes over time, providing a non-invasive method for monitoring healing. Repeated scans can show improvements in brain function and structure, reinforcing both clinical understanding and patient motivation.
Therapists use these objective measures to assess the effectiveness of treatment and to identify any early signs of relapse. If deterioration is detected, changes to the treatment plan can be made before the behaviour worsens. This proactive approach makes relapse prevention more targeted and effective.
Visual Feedback as a Therapeutic Tool
One powerful benefit of using radiology in addiction treatment is its ability to make the condition visible. For many patients, seeing the physical changes in their brain caused by substance use can be a wake-up call. It externalises the problem and reinforces the idea that addiction is a medical issue, not a personal weakness.
Conversely, images showing recovery in the brain can provide encouragement, reinforcing the value of continued therapy and abstinence. This kind of visual evidence can be especially helpful for individuals who struggle to see their progress in day-to-day life.
Radiology in Modern Therapeutic Practice
The use of radiology is growing in modern addiction treatment centres, supported by interdisciplinary collaboration between therapists, radiologists, and neurologists. These teams collaborate to interpret imaging results and incorporate them into care plans. Therapists find that radiology enhances the quality of their interventions and improves communication with patients.
As more research confirms the benefits of imaging in understanding and treating addiction, it is likely that radiology will become a routine component of addiction therapy. This integrated approach represents a shift from traditional methods to science-based, patient-centred care.
Conclusion
Radiology is transforming the field of drug addiction treatment by providing insights into the neurological effects of substance use and offering new ways to support recovery. From early diagnosis to personalised care and progress monitoring, imaging is becoming a valuable asset for therapists. By making addiction visible and measurable, radiology not only guides treatment but also empowers patients with a clearer understanding of their condition and recovery journey. As technology continues to advance, radiology’s role in supporting effective, long-term addiction therapy is set to expand further.
Disclaimer
The information presented in The Role of Radiology in Drug Addiction Treatment: A New Perspective for Therapists by Open Medscience (2025-06-04) is intended for educational and informational purposes only. It does not constitute medical advice, diagnosis, or treatment, and should not be relied upon as a substitute for consultation with qualified healthcare professionals. While the article discusses emerging applications of radiology in addiction therapy, readers should be aware that not all methods described are standard clinical practice and may not be available or appropriate for all patients. Open Medscience makes no representations or warranties about the accuracy, completeness, or applicability of the content in clinical settings. Therapists and clinicians should always use their professional judgement and consider individual patient circumstances when applying any medical or therapeutic interventions.