Summary: Radiotheranostics represents a powerful and increasingly essential approach in personalised medicine, uniting diagnostic imaging and targeted radionuclide therapy into a single molecular platform. This article examines the current clinical applications of radiotheranostics, innovations in radiopharmaceutical development, advancements in imaging and dosimetry, emerging targets, regulatory and ethical considerations, and future directions in the field. From prostate cancer to neuroendocrine tumours, this combined diagnostic–therapeutic strategy is redefining cancer care by enabling more precise, patient-specific treatment pathways.
Keywords: Radiotheranostics, Prostate Cancer, Radiopharmaceuticals, Personalised Medicine, Molecular Imaging, Targeted Therapy.
Introduction to Radiotheranostics
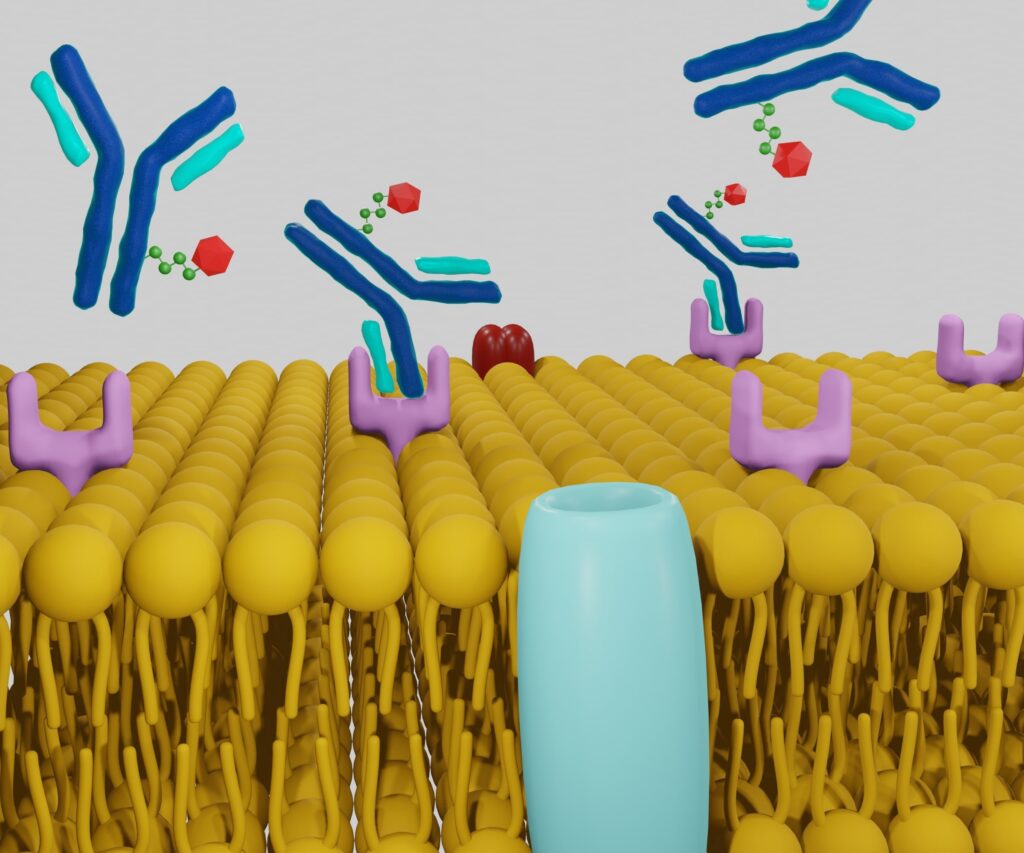
Radiotheranostics combines two essential functions — diagnosis and therapy — using a single molecular agent or pair of agents that target the same biological structure. Typically, the diagnostic agent is labelled with a positron or gamma emitter (such as ⁶⁸Ga or ⁹⁹ᵐTc) for imaging, while the therapeutic agent carries a cytotoxic radionuclide (e.g. ¹⁷⁷Lu or ²²⁵Ac). This dual functionality allows clinicians to visualise tumour burden, assess suitability for therapy, deliver targeted treatment, and monitor response — all based on the same molecular target.
The principle has gained wide acceptance in oncology, particularly for neuroendocrine tumours (NETs) and prostate cancer, with increasing research extending the applications to other cancers and even inflammatory or infectious diseases.
Clinical Applications: Where Theranostics Meets Oncology
Prostate Cancer: PSMA-Targeted Imaging and Therapy
One of the most significant milestones in radiotheranostics is the development of PSMA-targeted imaging and treatment for prostate cancer. ⁶⁸Ga-PSMA PET/CT has become an essential tool in detecting recurrent or metastatic disease with high specificity and sensitivity. Therapeutically, ¹⁷⁷Lu-PSMA delivers focused radiation to PSMA-expressing cells, offering improved survival outcomes in metastatic castration-resistant prostate cancer. Trials such as VISION have confirmed its efficacy and tolerability.
Neuroendocrine Tumours (NETs)
NETs are classically managed using somatostatin receptor (SSTR)-based theranostics. Diagnostic imaging with ⁶⁸Ga-DOTATATE PET/CT allows precise tumour visualisation, while ¹⁷⁷Lu-DOTATATE is used for peptide receptor radionuclide therapy (PRRT). This approach has shown durable responses, improved progression-free survival, and symptom control in metastatic or inoperable NETs.
Thyroid Cancer Beyond Radioiodine
Radioiodine therapy (¹³¹I) has long been the cornerstone of differentiated thyroid cancer treatment. However, for radioiodine-refractory disease, newer theranostic strategies using tracers that target alternative pathways (e.g., integrins or MET receptors) are being investigated to address therapeutic resistance.
Bone Metastases: A Focus on Radium-223
Radium-223 dichloride, an alpha emitter mimicking calcium, selectively targets bone metastases in prostate cancer. It provides symptomatic relief and survival benefit by delivering high-energy alpha particles to osseous lesions, minimising marrow toxicity. Its role continues to evolve within broader theranostic frameworks.
Emerging Paediatric Applications
Paediatric applications of radiotheranostics remain limited, partly due to regulatory concerns and concerns about radiation sensitivity. However, progress in neuroblastoma and paediatric gliomas using agents such as ¹³¹I-MIBG and ¹²⁴I-labelled antibodies is opening potential pathways for future integration.
Innovation in Radiopharmaceutical Development
Ligand Design and Radionuclide Selection
Successful radiotheranostics relies on selecting the right molecular ligand to target tumour-specific antigens. Peptides, antibodies, and small molecules are tailored to deliver diagnostic or therapeutic isotopes with minimal off-target effects. Chelators such as DOTA or NOTA play a critical role in securing radionuclides while maintaining bioactivity.
Alpha vs Beta Emitters
Beta emitters (such as ¹⁷⁷Lu) deliver lower energy over longer distances, making them suitable for bulky tumours. Alpha emitters (e.g. ²²⁵Ac, ²¹³Bi) release high-energy radiation over short paths, allowing more potent and localised tumour killing with less surrounding tissue damage — albeit with more complex handling requirements.
Nanotechnology and Theranostics
Nanoparticles are gaining interest for theranostic applications due to their multifunctionality and controlled pharmacokinetics. Functionalised with targeting moieties and loaded with both diagnostic and therapeutic payloads, these systems promise more intelligent delivery platforms, although few have reached clinical practice.
Advances in Imaging and Dosimetry
Personalised Dosimetry
Theranostic imaging enables a shift from empirical dosing to image-guided, personalised dosimetry. Quantitative imaging using SPECT/CT or PET/CT allows the accurate measurement of radiation absorbed by both tumours and normal tissues, thereby optimising efficacy while limiting toxicity.
Hybrid Imaging Modalities
The use of hybrid scanners, such as PET/MRI and SPECT/CT, enhances localisation and quantification of radiopharmaceuticals. MRI provides soft-tissue contrast, enhancing anatomical detail and facilitating functional correlation, particularly in the brain, liver, and pelvic organs.
Kinetic Modelling and Data Analysis
Advanced kinetic modelling helps refine radiopharmaceutical development by quantifying binding, internalisation, and clearance properties. Software platforms and artificial intelligence are now being used to predict therapeutic outcomes based on patient uptake patterns.
Regulatory, Commercial and Logistical Considerations
Licensing and Clinical Trial Design
Bringing a theranostic agent to clinical use requires careful alignment of regulatory pathways for both diagnostic and therapeutic agents, which are often treated as separate drug entities. Coordinated clinical trials with robust imaging endpoints are essential but challenging to design and fund.
Reimbursement and Health Economics
Although theranostics may reduce unnecessary treatments and improve outcomes, the initial cost of radiopharmaceuticals and infrastructure remains high. Cost-effectiveness studies are increasingly influencing reimbursement decisions, particularly in public healthcare systems like the NHS.
Supply Chain and Radiopharmacy
Manufacturing, transporting, and delivering short-lived isotopes require coordinated logistics, especially for isotopes like ⁶⁸Ga, which has a 68-minute half-life. In-house generators, cyclotron production, and regional radiopharmacy networks are critical components of a reliable supply chain.
Emerging Targets and Novel Indications
Beyond Oncology: Inflammation and Infection
Radiotheranostics is now being explored in non-oncological conditions, including sarcoidosis, tuberculosis, and rheumatoid arthritis, using tracers targeting activated immune cells or microbial markers. These may enable early detection and tailored anti-inflammatory therapy.
New Molecular Targets: FAP, CXCR4, GRPR
Fibroblast activation protein (FAP), C-X-C chemokine receptor 4 (CXCR4), and gastrin-releasing peptide receptors (GRPR) represent newer targets under active investigation. FAP inhibitors, for instance, are showing promise in various carcinomas, enabling imaging and therapy of previously “non-theranostic” cancers.
Artificial Intelligence in Theranostics
AI tools are being developed to interpret complex imaging data, model radiation dosimetry, and stratify patients based on radiomic features. Integration of machine learning could enhance theranostic workflows and assist in predictive modelling of treatment response.
Safety, Ethics, and Patient Perspectives
Radiation Safety and Facility Requirements
Handling both imaging and therapeutic isotopes requires rigorous safety protocols. Shielded treatment rooms, designated waste systems, and trained personnel are essential for protecting patients and staff.
Informed Consent and Communication
Patients undergoing theranostic procedures must understand the diagnostic and therapeutic intent, potential side effects, and limitations associated with these procedures. Clear communication — particularly in terms of therapy expectations and outcomes — enhances shared decision-making.
Ethical Issues in Palliative Settings
Many patients receiving theranostic therapy are in advanced stages of cancer. Ethical concerns include balancing hope with realism, managing radiation exposure among caregivers, and ensuring equitable access across demographics and regions.
Future Outlook
Radiotheranostics is gaining rapid momentum as a precision oncology tool. The integration of novel targets, more potent radionuclides, nanotechnology, and artificial intelligence will likely push the boundaries further. As evidence grows and logistical hurdles are addressed, radiotheranostics is poised to become a standard component of cancer management.
The key to its continued success lies in multidisciplinary collaboration: nuclear medicine, medical oncology, radiopharmacy, physics, regulatory agencies, and patient advocacy must work together to ensure this promising strategy reaches its full clinical potential.
Conclusion
Radiotheranostics offers a paradigm shift in how we approach cancer diagnosis and therapy, with the power to visualise, personalise, and treat disease in a single clinical workflow. From early detection to precision therapy, this strategy exemplifies the direction of modern medicine: targeted, data-driven, and patient-centred. As the field evolves, it not only brings new tools but also a fundamentally different approach to treating complex diseases with confidence and clarity.
Disclaimer
The content provided in this article is intended for informational and educational purposes only. It does not constitute medical advice, diagnosis, or treatment recommendations and should not be relied upon as a substitute for consultation with qualified healthcare professionals. While every effort has been made to ensure the accuracy and currency of the information presented, Open Medscience makes no guarantees or warranties, express or implied, regarding the completeness, reliability, or applicability of the content.
References to specific radiopharmaceuticals, clinical trials, or medical procedures are for illustrative purposes and do not imply endorsement or suitability for any individual patient. Readers are encouraged to consult appropriate clinical and regulatory guidance before considering or implementing any medical intervention discussed herein.
Open Medscience accepts no responsibility for any actions taken based on the information contained in this article. The views expressed are those of the authors and contributors and do not necessarily reflect the official policy or position of any affiliated institutions or organisations.
home » blog » radiotheranostics »