Pittsburgh Compound-B (PIB) is a carbon-11-labelled benzothiazole derivative of the amyloid dye thioflavin T. First developed preclinically at the University of Pittsburgh; PIB has become a crucial tool in the study and early diagnosis of Alzheimer’s disease. This compound binds specifically to amyloid plaques, which are hallmark features of Alzheimer’s pathology, allowing for in vivo imaging using positron emission tomography (PET). The development of PIB has revolutionised Alzheimer’s research, enabling earlier diagnosis, better understanding of disease progression, and the potential for evaluating the efficacy of therapeutic interventions.
The Development of Pittsburgh Compound-B (PIB)
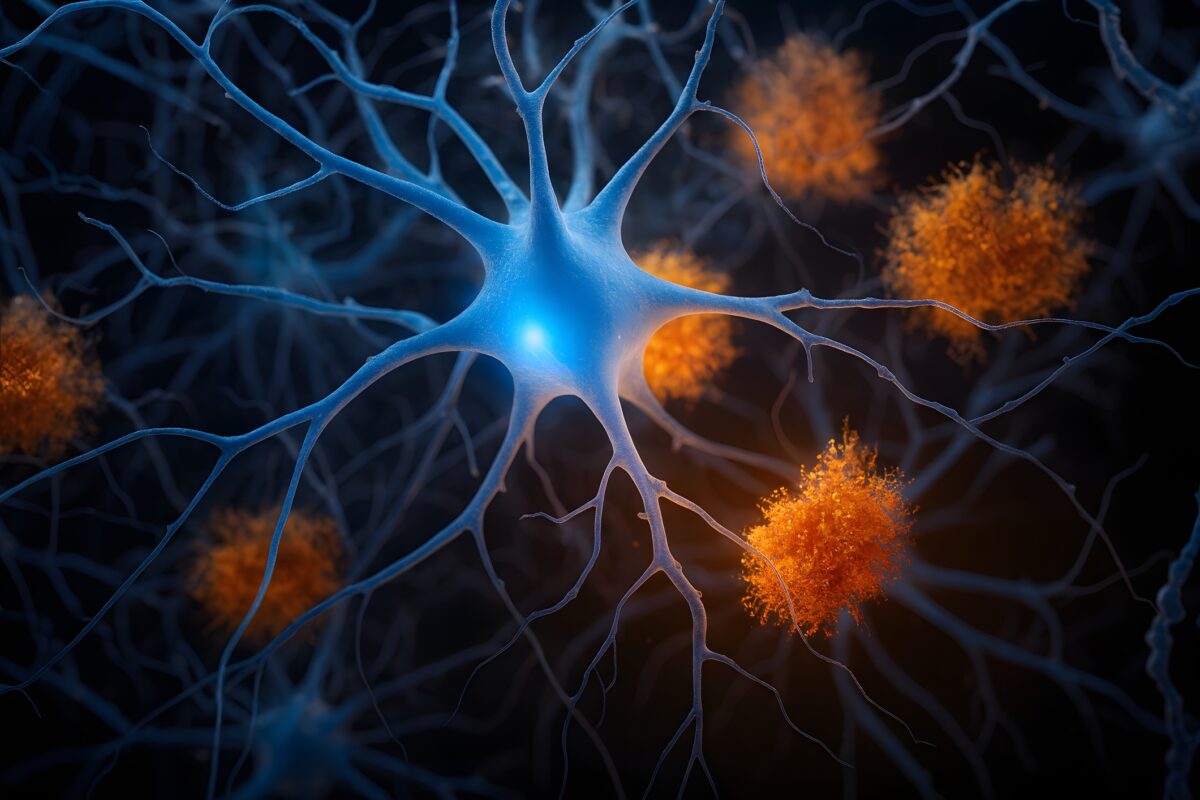
Alzheimer’s disease, a neurodegenerative disorder characterised by memory loss, cognitive decline, and behavioural changes, has posed significant challenges in both diagnosis and treatment. One of the primary pathological features of Alzheimer’s disease is the accumulation of amyloid-beta plaques in the brain. These plaques, composed mainly of aggregated amyloid-beta peptides, are believed to play a central role in the development and progression of the disease.
The ability to detect amyloid plaques in living patients has long been a goal in Alzheimer’s research. Before the advent of imaging techniques, amyloid plaques could only be confirmed through post-mortem examination. However, the Pittsburgh Compound-B (PIB) development has transformed this landscape, offering a non-invasive method to visualise amyloid plaques in vivo.
Pittsburgh Compound-B (PIB) was first developed preclinically at the University of Pittsburgh by a team of researchers led by Drs. Chester Mathis and William Klunk. The compound is a derivative of thioflavin T, a dye that has long been used to stain amyloid plaques in histological studies. However, Thioflavin T is unsuitable for in vivo imaging due to its poor ability to cross the blood-brain barrier and its non-specific binding properties.
The research team at the University of Pittsburgh sought to create a compound that would retain the amyloid-binding properties of thioflavin T while overcoming its limitations for in vivo use. By introducing a carbon-11 radioisotope into the structure of a benzothiazole derivative, they developed PIB. Carbon-11, a positron-emitting isotope, allows PIB to be detected by positron emission tomography (PET) imaging.
The Mechanism of Action of PIB
PIB binds specifically to amyloid-beta plaques in the brain due to its structural similarity to thioflavin T. The benzothiazole moiety in PIB interacts with the beta-sheet structure of amyloid fibrils, a characteristic feature of amyloid plaques. This binding is highly specific, meaning that PIB predominantly accumulates in regions of the brain with high concentrations of amyloid plaques, such as the cortex.
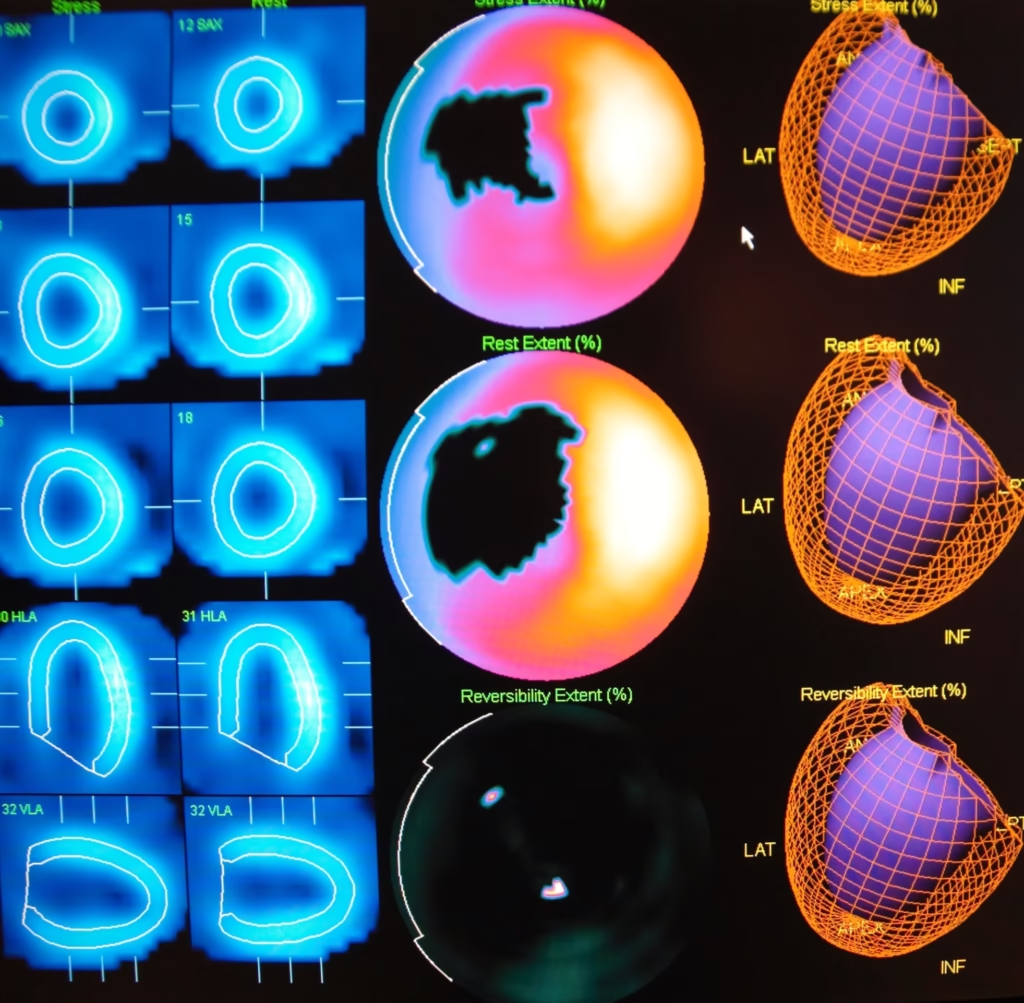
When injected into a patient, PIB crosses the blood-brain barrier and binds to amyloid plaques. The carbon-11 isotope within PIB decays, emitting positrons. These positrons interact with electrons in the surrounding tissue, producing gamma rays that are detected by the PET scanner. Researchers and clinicians can generate detailed images of amyloid plaque distribution within the brain by analysing the distribution of these gamma rays.
PIB in Alzheimer’s Disease Diagnosis
The introduction of PIB-PET imaging has been a significant advancement in the diagnosis of Alzheimer’s disease. Previously, the clinical diagnosis of Alzheimer’s relied heavily on cognitive assessments and the exclusion of other potential causes of dementia. However, PIB-PET imaging directly measures amyloid plaque burden in the brain, offering a more definitive diagnostic tool.
PIB-PET imaging has been particularly valuable in distinguishing Alzheimer’s disease from other forms of dementia. For example, patients with frontotemporal dementia, a condition that shares some clinical features with Alzheimer’s, typically do not exhibit significant amyloid plaque accumulation. PIB-PET imaging can, therefore, aid in the differential diagnosis of these conditions.
Additionally, PIB-PET imaging has enabled the identification of amyloid-positive individuals who are asymptomatic. These individuals, often referred to as “preclinical” Alzheimer’s patients, show significant amyloid plaque deposition despite the absence of cognitive symptoms. The ability to detect amyloid plaques at this early stage has important implications for developing preventative strategies and understanding disease progression.
Research Applications of PIB
Beyond its clinical utility, PIB has become an invaluable tool in Alzheimer’s research. One of the key areas where PIB has had a significant impact is in the study of the natural history of Alzheimer’s disease. Longitudinal studies using PIB-PET imaging have provided insights into the temporal relationship between amyloid plaque deposition and cognitive decline.
These studies have shown that amyloid plaque deposition begins many years, possibly even decades, before the onset of clinical symptoms. This finding has led to the hypothesis that Alzheimer’s disease has a long preclinical phase during which amyloid pathology accumulates silently in the brain. Understanding this phase is critical for developing interventions that can slow or prevent the progression to symptomatic Alzheimer’s disease.
PIB-PET imaging has also been used to evaluate the efficacy of potential Alzheimer’s treatments. Clinical trials often use PIB-PET imaging as a biomarker to assess whether a therapeutic agent can reduce the amyloid plaque burden in the brain. By providing a direct measure of amyloid pathology, PIB allows researchers to determine the impact of treatments on the underlying disease process rather than relying solely on clinical outcomes.
Limitations and Challenges
While PIB has been a breakthrough in Alzheimer’s research, it is not without its limitations. One of the primary challenges with PIB is its reliance on the short-lived carbon-11 isotope, which has a half-life of about 20 minutes. This necessitates the availability of an on-site cyclotron for the production of carbon-11, limiting the widespread use of PIB to specialised research centres with this capability.
Another limitation of PIB is its specificity for amyloid plaques, which means that it does not provide information about other pathological features of Alzheimer’s disease, such as neurofibrillary tangles composed of tau protein. Consequently, PIB-PET imaging alone cannot provide a complete picture of Alzheimer’s pathology.
Moreover, while PIB-PET imaging can detect amyloid plaques, the presence of amyloid pathology does not always correlate with clinical symptoms. Some individuals with significant amyloid plaque deposition remain cognitively normal, suggesting that amyloid plaques are necessary but not sufficient for the development of Alzheimer’s disease. This complexity underscores the need for additional biomarkers and imaging techniques to fully understand the disease process.
Advancements Beyond PIB
Since the development of PIB, there have been efforts to create new amyloid imaging agents that overcome some of its limitations. For example, fluorine-18-labelled compounds, such as florbetapir, florbetaben, and flutemetamol, have been developed for amyloid imaging. Fluorine-18 has a longer half-life (approximately 110 minutes) than carbon-11, allowing for wider distribution and use in clinical settings without needing an on-site cyclotron.
These newer amyloid imaging agents have expanded the availability of amyloid PET imaging, making it accessible to a broader range of clinical and research facilities. Moreover, some of these agents have received regulatory approval for clinical use, allowing for amyloid imaging to be incorporated into routine clinical practice for diagnosing and managing Alzheimer’s disease.
The Future of Alzheimer’s Imaging and Biomarkers
The development of PIB marked the beginning of a new era in Alzheimer’s research, where in vivo imaging of amyloid plaques became possible. However, the future of Alzheimer’s imaging and biomarkers is likely to involve a combination of modalities that provide a more comprehensive view of the disease.
For instance, tau PET imaging, which detects neurofibrillary tangles, is increasingly being used alongside amyloid PET imaging to assess both major pathological features of Alzheimer’s disease. In addition, advances in cerebrospinal fluid (CSF) and blood biomarkers are providing complementary information that can aid in the early diagnosis and monitoring of disease progression.
The integration of multiple biomarkers is expected to enhance the accuracy of Alzheimer’s diagnosis and enable a more personalised approach to treatment. For example, identifying individuals with high amyloid and tau burden who are at greatest risk of cognitive decline could inform the selection of patients for clinical trials and therapeutic interventions.
Conclusion
Pittsburgh Compound-B (PIB) has been a transformative tool in Alzheimer’s disease research and diagnosis. Developed at the University of Pittsburgh, PIB has enabled the in vivo imaging of amyloid plaques, providing critical insights into the pathology of Alzheimer’s disease. Its impact on clinical practice and research has been profound, offering a window into the previously unavailable brain.
Although PIB has its limitations, it paved the way for the development of other amyloid imaging agents and advanced our understanding of Alzheimer’s disease. As research continues, the combination of amyloid imaging with other biomarkers and modalities will likely provide even greater clarity into the complex processes underlying Alzheimer’s disease, ultimately leading to improved diagnosis, treatment, and potentially prevention of this devastating condition.
Disclaimer
The content presented in The Discovery and Development of Pittsburgh Compound-B (PIB): A Breakthrough in Alzheimer’s Disease Research by Open Medscience is intended for informational and educational purposes only. While every effort has been made to ensure the accuracy and reliability of the information, it should not be considered medical advice, diagnostic guidance, or a substitute for consultation with qualified healthcare professionals.
Open Medscience does not endorse or recommend any specific medical treatments, diagnostic tools, or interventions mentioned in this article. The research findings and opinions expressed are those of the original authors and sources cited, and do not necessarily reflect the views of Open Medscience.
Readers should consult medical professionals or specialists before making any decisions related to the diagnosis, treatment, or management of Alzheimer’s disease or any other health condition. Open Medscience disclaims any liability for the use or misuse of the information contained herein.
home » blog » nuclear medicine imaging »