Radiotheranostics is an innovative medical approach combining diagnostic imaging and therapeutic radiology to target and treat specific diseases, particularly cancers. This fusion of “radiotherapy” and “theranostics” allows for precise localisation, diagnosis, and treatment, often enhancing the efficacy and reducing side effects of traditional therapies. This essay explores the fundamentals of radiotheranostics, its components, applications in cancer treatment, advancements, challenges, and future prospects.
Introduction to Radiotheranostics
Radiotheranostics represents a paradigm shift in the medical field, offering a personalised approach to disease management. Integrating diagnostic imaging and targeted radiotherapy provides a comprehensive pathway from detection to treatment. It primarily focuses on using radioactive substances for both imaging and therapy, ensuring that treatment is effective and precisely targeted.
The Fundamentals of Radiotheranostics
Radiotheranostics merges two key components: diagnostic imaging and therapeutic radiology. Diagnostic imaging involves the use of radioactive tracers to visualise specific tissues or organs, aiding in the detection and characterisation of diseases. On the other hand, therapeutic radiology utilises these radioactive substances to deliver targeted radiation therapy to diseased cells, particularly cancer cells, thereby minimising damage to surrounding healthy tissues.
Mechanism of Action
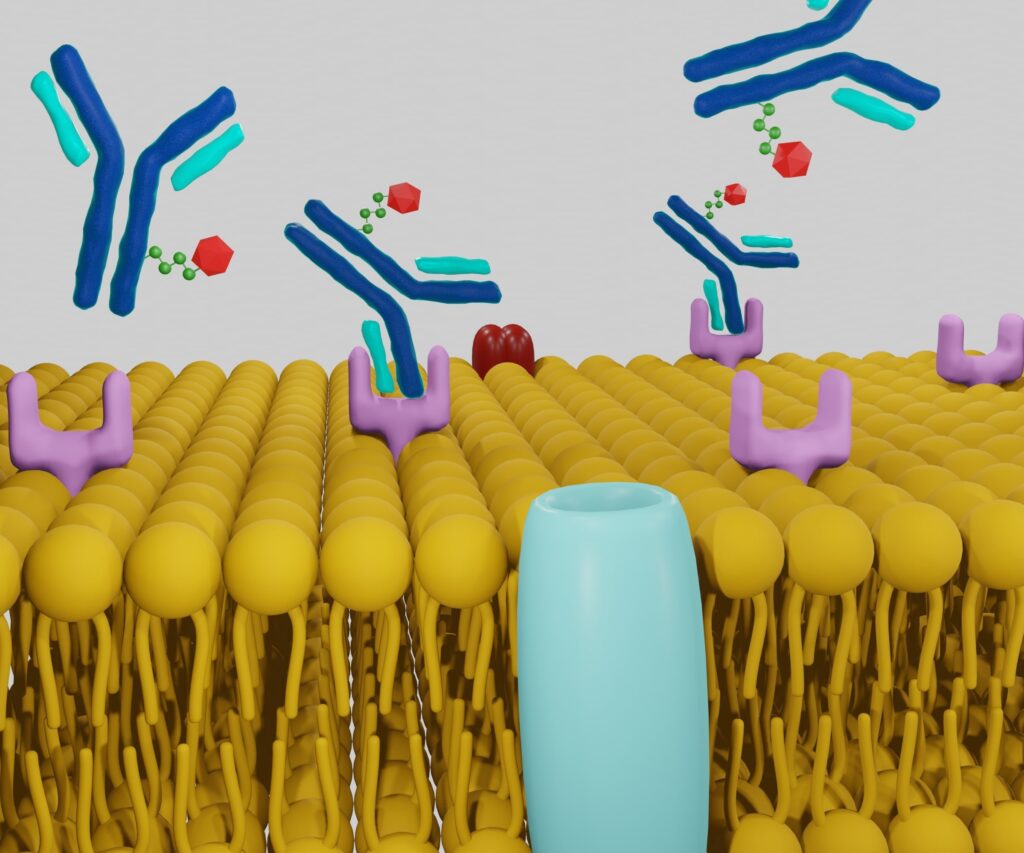
The mechanism of radiotheranostics involves the administration of radiopharmaceuticals, which are compounds that contain radioactive isotopes. These radiopharmaceuticals have an affinity for specific biological targets, such as cancer cells. Once administered, they accumulate in the target area, allowing for precise imaging and targeted radiotherapy. The dual role of these compounds ensures that the same agent used for diagnosis can also be utilised for treatment, streamlining the therapeutic process.
Applications in Cancer Treatment
Cancer treatment is one of the primary applications of radiotheranostics. Traditional cancer therapies, such as chemotherapy and external beam radiation, often affect both cancerous and healthy cells, leading to significant side effects. Radiotheranostics offers a more targeted approach, significantly reducing collateral damage. For instance, in prostate cancer, radiopharmaceuticals like PSMA (Prostate-Specific Membrane Antigen) ligands are used for both PET (Positron Emission Tomography) imaging and radionuclide therapy, allowing for precise localisation and effective treatment of cancerous tissues.
Personalised Treatment Plans
Radiotheranostics enables the development of personalised treatment plans. By using diagnostic imaging, physicians can assess a tumour’s extent and specific characteristics, facilitating tailored therapeutic strategies. This personalised approach enhances treatment efficacy and reduces unnecessary exposure to radiation, thereby improving patient outcomes.
Advancements in Radiotheranostics
Recent advancements in radiotheranostics have led to the development of novel radiopharmaceuticals. These new compounds offer improved targeting capabilities and reduced toxicity. For example, the introduction of 68Ga-DOTATATE for neuroendocrine tumours and 177Lu-PSMA for prostate cancer has revolutionised treatment protocols, providing more effective and safer options for patients.
Technological Innovations
Technological innovations in imaging and radiotherapy have also contributed to the progress of radiotheranostics. Enhanced imaging techniques, such as hybrid PET/CT and PET/MRI scanners, provide more detailed and accurate visualisation of tumours. Additionally, advancements in radiotherapy delivery systems, including intensity-modulated radiation therapy (IMRT) and stereotactic body radiotherapy (SBRT), allow for precise radiopharmaceuticals targeting further improving treatment outcomes.
Challenges in Radiotheranostics
One of the significant challenges in the field of radiotheranostics is navigating regulatory hurdles. The approval process for new radiopharmaceuticals is rigorous, involving extensive clinical trials to ensure safety and efficacy. This process can be time-consuming and costly, potentially delaying the availability of innovative treatments to patients.
Limited Availability and Accessibility
Another challenge is the limited availability and accessibility of radiotheranostics. The production of radiopharmaceuticals requires specialised facilities and expertise, which are not widely available. This limitation can restrict access to these advanced treatments, particularly in regions with underdeveloped healthcare infrastructure.
Cost Considerations
The cost of radiotheranostic treatments can also be a barrier. The development, production, and administration of radiopharmaceuticals involve significant expenses, which can result in high treatment costs for patients. Ensuring that these treatments are affordable and accessible is a critical challenge that needs to be addressed to maximise their impact.
Future Prospects of Radiotheranostics
The future of radiotheranostics holds promise for expanding its applications beyond cancer treatment. Research is ongoing to explore its potential in managing other diseases, such as cardiovascular conditions, neurological disorders, and infectious diseases. The ability to precisely target and treat specific disease sites makes radiotheranostics a versatile tool in modern medicine.
Integration with Other Modalities
Integrating radiotheranostics with other therapeutic modalities, such as immunotherapy and gene therapy, is another exciting prospect. Combining these approaches can enhance treatment efficacy and provide synergistic effects, offering new hope for patients with challenging conditions. For instance, radiotheranostics can be used to deliver radiation directly to tumour sites, enhancing the effectiveness of immunotherapy by increasing tumour cell kill and stimulating the immune response.
Advances in Radiopharmaceutical Development
Continued advances in radiopharmaceutical development are expected to drive the future of radiotheranostics. Researchers are focusing on creating new compounds with improved targeting abilities, reduced side effects, and longer half-lives, which can improve treatments’ overall efficacy and safety. Innovations in molecular biology and chemistry are likely to yield more sophisticated radiopharmaceuticals capable of addressing a wider range of diseases.
Precision Medicine and Personalisation
The trend towards precision medicine and personalised healthcare is expected to boost the adoption of radiotheranostics further. As the understanding of genetic and molecular profiles of diseases improves, radio theranostics can be tailored to individual patient’s needs, ensuring that treatments are optimised for maximum effectiveness with minimal side effects.
Conclusion
Radiotheranostics represents a transformative approach in the medical field, merging radiopharmaceuticals’ diagnostic and therapeutic potential to offer targeted, effective, and personalised treatments. Its primary application in cancer treatment has already shown significant promise, with ongoing advancements poised to expand its utility across various medical conditions. However, challenges such as regulatory hurdles, accessibility issues, and cost considerations must be addressed to realise its potential fully. With continuous research and technological innovation, radiotheranostics is set to play a pivotal role in the future of personalised medicine, offering new hope and improved outcomes for patients worldwide.
Disclaimer
The content of this article is provided for informational and educational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Radiotheranostics is an evolving field, and the information presented may not reflect the most current research or clinical guidelines. Readers should always seek the advice of their physician or qualified healthcare provider with any questions they may have regarding a medical condition or treatment options. Open Medscience does not endorse or recommend any specific tests, treatments, procedures, or opinions mentioned in this article. Reliance on any information provided by Open Medscience is solely at the reader’s own risk.