Summary: Nuclear medicine is a vital branch of modern healthcare, merging chemistry, physics, biology, and medicine to diagnose and treat diseases. This field is built upon three primary elements: the clinical problem being addressed, the radiopharmaceutical used, and the instrumentation employed to detect and process radiation. As nuclear medicine involves exposing patients to ionising radiation, adherence to radiation protection principles is paramount. This article explores each element in detail and examines the essential safety measures required to protect patients and professionals.
Introduction to Nuclear Medicine
Nuclear medicine provides a unique approach to diagnosing and treating diseases by visualising physiological processes at a molecular level. It differs from traditional imaging modalities like X-rays and CT scans by using radioactive substances, known as radiopharmaceuticals, to track biological pathways and target specific conditions. However, the involvement of radiation necessitates strict adherence to safety protocols.
Role of Nuclear Medicine in Disease Management
The clinical problem is the cornerstone of any nuclear medicine procedure. The diagnostic or therapeutic objective defines the selection of radiopharmaceuticals and instrumentation. Nuclear medicine is particularly effective in diagnosing and treating conditions that require real-time imaging of metabolic or functional processes, such as:
- Cancer: Identifying malignant tissues and assessing treatment response.
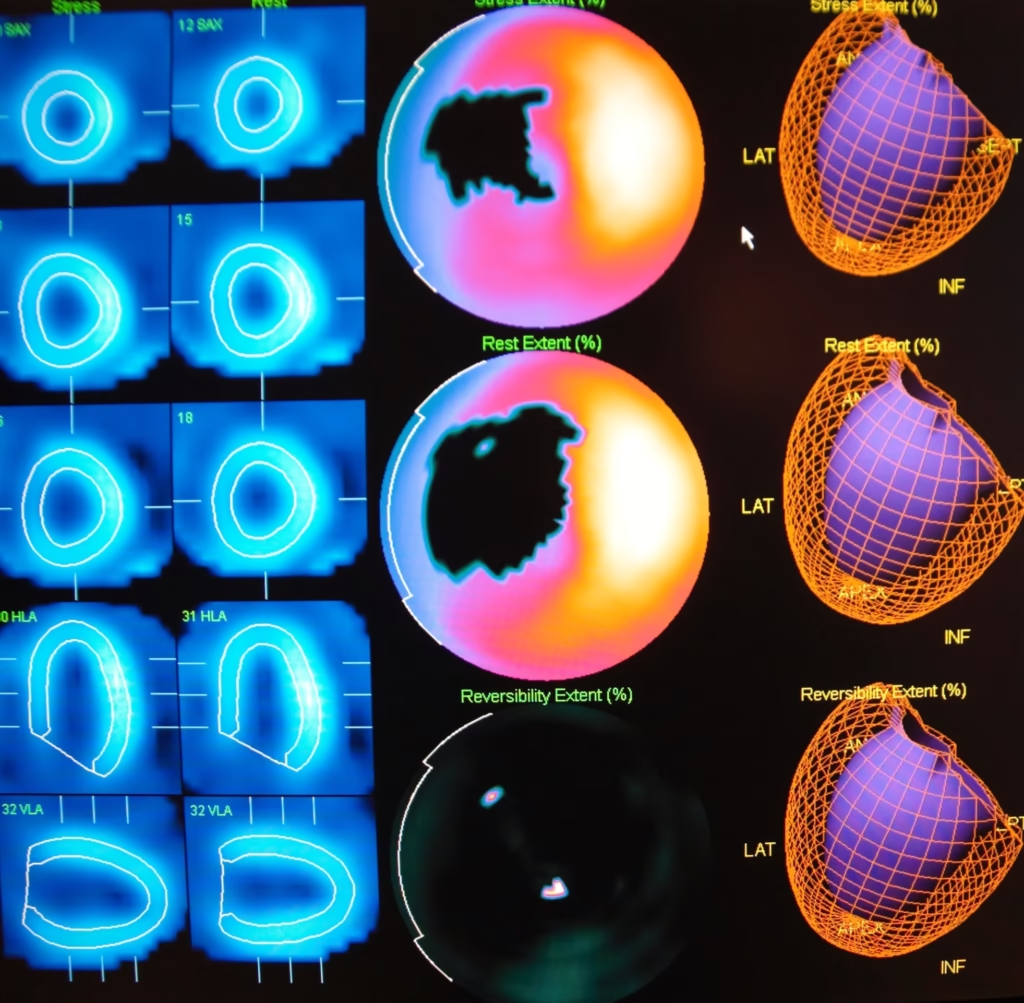
- Cardiovascular Diseases: Evaluating myocardial perfusion and viability.
- Neurological Disorders: Diagnosing conditions like Alzheimer’s disease and epilepsy.
- Endocrine Disorders: Imaging thyroid function and detecting parathyroid adenomas.
Defining the Clinical Question
A clear understanding of the clinical question ensures the proper use of nuclear medicine. For instance, if a clinician suspects coronary artery disease, myocardial perfusion imaging (MPI) may be recommended. Conversely, if assessing cancer metastasis, a PET-CT scan might be the preferred option.
What Are Radiopharmaceuticals?
Radiopharmaceuticals are compounds that combine a radioactive isotope with a biologically active molecule. The isotope emits radiation detectable by imaging equipment, while the molecule targets specific biological processes. For example:
- Technetium-99m: Widely used for bone scans and cardiac imaging.
- Fluorine-18 (in FDG): A radiotracer used in PET scans to detect cancer.
- Iodine-131: A therapeutic radiopharmaceutical for thyroid conditions.
- Gallium-68: Used for imaging neuroendocrine tumours.
Production and Decay
Radiopharmaceuticals are typically produced in cyclotrons or nuclear reactors and have a limited shelf life due to radioactive decay. This short half-life minimises patient exposure but necessitates efficient logistics for their production, transport, and use.
Applications in Therapy and Diagnosis
Nuclear medicine encompasses both diagnostic and therapeutic applications:
- Diagnostics: Imaging procedures using tracers like FDG to visualise metabolic activity.
- Therapeutics: Targeted radiation to treat conditions such as hyperthyroidism or cancer. An example is the use of Lutetium-177 for prostate cancer therapy.
Instrumentation
Instrumentation is the third critical pillar of nuclear medicine, designed to detect and process the radiation emitted by radiopharmaceuticals. Key devices include:
- Gamma Cameras: Used for single-photon emission computed tomography (SPECT). They detect gamma rays emitted by radiotracers.
- Positron Emission Tomography (PET) Scanners: Detect positrons emitted during radiotracer decay and create highly detailed images.
- Hybrid Systems (PET-CT, SPECT-CT): Combine functional imaging with anatomical data for improved diagnosis.
- Radiation Detectors: Devices like Geiger-Müller counters monitor radiation levels in the environment or on patients.
Advances in Instrumentation
Modern systems offer greater sensitivity and resolution, enhancing diagnostic accuracy. For example:
- Digital PET Scanners: Provide sharper images and reduce the required dose of radiopharmaceuticals.
- AI Integration: Artificial intelligence is increasingly used to process imaging data, improving speed and precision.
Principles of Radiation Protection
The use of radioactive substances inherently involves risks. Exposure to ionising radiation can damage tissues and increase the risk of cancer over time. Consequently, radiation protection principles are integral to nuclear medicine.
The ALARA Principle
Radiation protection follows the ALARA (As Low As Reasonably Achievable) principle, which involves:
- Time: Minimising the duration of exposure.
- Distance: Increasing the distance between the radiation source and individuals.
- Shielding: Using barriers like lead aprons and walls to block radiation.
Patient Safety
For patients, safety measures include:
- Administering the smallest effective dose.
- Tailoring protocols to the individual’s health status.
- Monitoring radiation exposure during and after procedures.
Professional Safety
For healthcare workers, safety protocols are crucial to minimise occupational exposure. These include:
- Regular dosimetry monitoring to track cumulative radiation doses.
- Use of personal protective equipment (PPE) such as lead-lined gloves.
- Limiting time spent in proximity to radioactive materials.
Environmental Considerations
The safe disposal of radioactive waste is a critical aspect of radiation protection. Hospitals and laboratories follow strict regulations to prevent environmental contamination.
Integration of the Three Elements
A Holistic Approach
The effectiveness of nuclear medicine lies in the seamless integration of the clinical problem, radiopharmaceutical, and instrumentation. Each element complements the others, creating a comprehensive system for diagnosing and treating diseases.
For example, in a case of suspected lung cancer:
- Clinical Problem: Determining the presence and extent of the tumour.
- Radiopharmaceutical: Administering Fluorine-18 FDG to highlight cancerous cells.
- Instrumentation: Using a PET-CT scanner to obtain precise images.
Challenges in Integration
- Availability of Radiopharmaceuticals: Limited access to isotopes can delay diagnosis and treatment.
- Cost: Nuclear medicine equipment and radiopharmaceuticals are expensive, posing challenges for resource-limited settings.
- Training: Skilled personnel are required to interpret results and operate advanced equipment.
Future Directions
Personalised Medicine
Advances in nuclear medicine are paving the way for personalised healthcare. Radiopharmaceuticals can be tailored to target specific biomarkers, improving therapeutic outcomes.
New Isotopes and Tracers
Research is ongoing to develop novel isotopes and tracers with improved specificity and reduced side effects. For instance, Copper-64 and Zirconium-89 are being explored for cancer imaging.
Non-Invasive Techniques
Efforts are underway to enhance non-invasive imaging technologies, reducing the need for biopsies and other invasive procedures.
Conclusion
Nuclear medicine is a transformative field that bridges molecular biology and imaging to diagnose and treat diseases. By focusing on the clinical problem, employing appropriate radiopharmaceuticals, and using advanced instrumentation, this field offers unparalleled insights into human health. However, the inherent risks associated with radiation necessitate strict adherence to radiation protection principles. As the field continues to evolve, innovations promise even greater precision, safety, and accessibility, ensuring that nuclear medicine remains a cornerstone of modern healthcare.
Disclaimer
The information presented in this article is intended for general educational and informational purposes only. It does not constitute professional medical, scientific, or technical advice and should not be relied upon as such. Open Medscience makes every effort to ensure that the content is accurate and up to date at the time of publication; however, developments in medical science and practice may occur that render some information obsolete or incomplete.
Readers should not use the information contained herein as a substitute for professional medical consultation, diagnosis, or treatment. Decisions relating to patient care must be made by qualified healthcare professionals, taking into account individual circumstances and local guidelines.
Furthermore, while the article discusses aspects of nuclear medicine involving ionising radiation, all procedures should only be conducted in compliance with relevant safety regulations, under the supervision of trained professionals, and in accredited medical facilities.
Open Medscience and its contributors accept no responsibility for any loss, injury, or damage arising from the use of or reliance upon the material contained in this publication.
You are here: home » diagnostic medical imaging blog »