Summary: Positron emission tomography combined with computed tomography (PET/CT) has transformed the diagnostic evaluation and management of thyroid cancer. By merging functional and anatomical imaging, PET/CT enables precise tumour localisation, staging, and assessment of metabolic activity. The integration of 18F-fluorodeoxyglucose (FDG) PET with CT has proven particularly valuable in detecting recurrent and metastatic disease, evaluating indeterminate lesions, and guiding treatment decisions in patients with differentiated and undifferentiated thyroid carcinomas. This article examines the clinical role of PET/CT in thyroid cancer, including its diagnostic accuracy, prognostic implications, limitations, and its evolving contribution to personalised oncology.
Keywords: PET/CT, Thyroid Cancer, 18F-FDG, Imaging, Diagnosis, Oncology.
Introduction
Thyroid cancer represents the most common endocrine malignancy, with a steadily increasing global incidence over the past few decades. The disease encompasses a spectrum of histological types, including papillary, follicular, medullary, and anaplastic thyroid carcinoma, each with distinct biological behaviour and clinical outcomes. Conventional diagnostic methods, such as ultrasonography, computed tomography (CT), magnetic resonance imaging (MRI), and radioiodine scintigraphy, remain central to the evaluation of thyroid cancer. However, these modalities primarily offer anatomical information, which may not sufficiently characterise tumour metabolism or identify aggressive disease.
Positron emission tomography (PET), particularly when combined with computed tomography (PET/CT), has become a vital tool in oncological imaging. PET provides functional insights into glucose metabolism, while CT contributes detailed anatomical context. The use of 18F-fluorodeoxyglucose (18F-FDG) in PET imaging exploits the increased glucose uptake and glycolytic activity typical of malignant cells, thereby facilitating the detection of both primary and secondary tumour sites. In the context of thyroid cancer, PET/CT serves a pivotal role in identifying lesions that are not iodine-avid and in evaluating patients with elevated serum thyroglobulin but negative radioiodine scans.
Principles of PET/CT Imaging in Thyroid Cancer
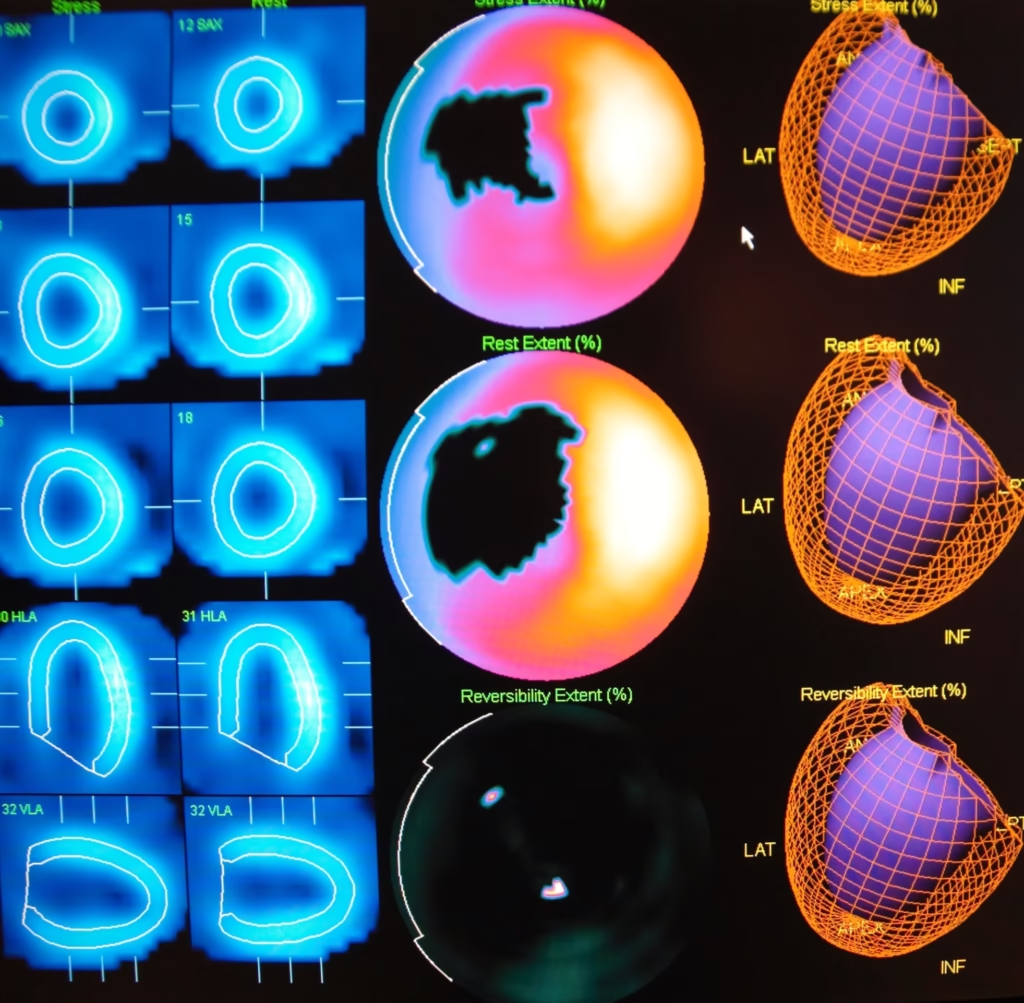
PET/CT integrates two complementary imaging modalities. The PET component measures the distribution of radiolabelled tracers, most commonly 18F-FDG, a glucose analogue that accumulates in metabolically active tissues. The CT component provides high-resolution anatomical images that aid in precise localisation and attenuation correction. The combined dataset allows clinicians to visualise both metabolic and structural changes within the same examination.
In thyroid oncology, the metabolic activity visualised by PET/CT often correlates with tumour aggressiveness and dedifferentiation. Differentiated thyroid cancers, such as papillary and follicular subtypes, typically demonstrate low FDG uptake when iodine-avid, as they retain the ability to trap and organify iodine. Conversely, dedifferentiated or radioiodine-refractory lesions frequently exhibit high FDG uptake due to enhanced glycolytic metabolism and loss of iodine-handling capacity. This inverse relationship between iodine avidity and FDG uptake, sometimes referred to as the “flip-flop phenomenon”, forms the basis for using FDG-PET/CT in the evaluation of refractory thyroid cancers.
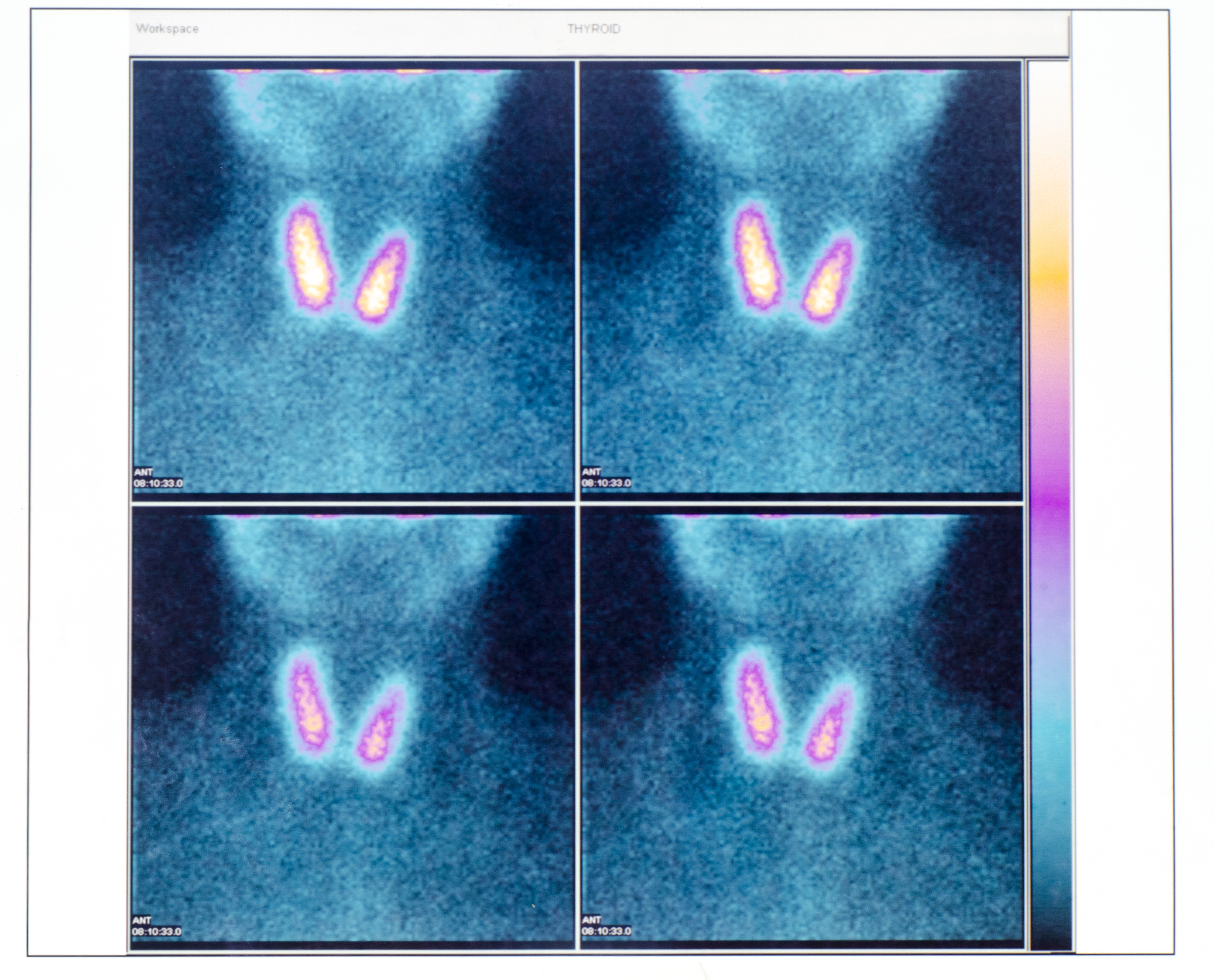
PET/CT in the Detection and Characterisation of Primary Thyroid Lesions
While PET/CT is not routinely used as an initial diagnostic tool for primary thyroid nodules, it often reveals incidental focal uptake in the thyroid gland during imaging performed for other malignancies. Such incidental findings, known as “thyroid incidentalomas”, are observed in approximately 1–4% of PET/CT scans. Studies indicate that a substantial proportion of these lesions—up to 35%—represent malignancy, particularly papillary thyroid carcinoma. Therefore, focal thyroid FDG uptake warrants further evaluation through ultrasonography and fine-needle aspiration cytology.
In cases where conventional imaging or cytology yields indeterminate results, PET/CT may assist in differentiating benign from malignant nodules. Malignant nodules typically display higher standardised uptake values (SUVs), reflecting increased metabolic activity. However, caution is necessary since inflammatory and benign hyperplastic processes can also result in elevated FDG uptake. Thus, PET/CT findings must be interpreted in conjunction with clinical and biochemical data.
Role of PET/CT in Staging and Restaging of Thyroid Cancer
Accurate staging is essential for determining prognosis and guiding treatment in thyroid cancer. PET/CT provides valuable information in both the preoperative and postoperative settings, particularly for identifying regional and distant metastases that may not be visualised using conventional modalities.
In differentiated thyroid cancer, 18F-FDG PET/CT is particularly useful in patients with elevated serum thyroglobulin levels and negative radioiodine whole-body scans. These patients often harbour recurrent or metastatic disease that has lost the ability to concentrate iodine. PET/CT can localise such lesions in the neck, mediastinum, lungs, or bones, thereby influencing subsequent therapeutic planning.
For medullary thyroid carcinoma (MTC), which arises from parafollicular C cells and does not concentrate iodine, FDG-PET/CT has shown promise in detecting residual or metastatic disease in patients with elevated calcitonin levels. Furthermore, alternative tracers such as 18F-dihydroxyphenylalanine (18F-DOPA) and 68Ga-DOTATATE have demonstrated enhanced sensitivity in MTC imaging.
In anaplastic thyroid carcinoma (ATC), an aggressive and undifferentiated form of the disease, PET/CT plays a key role in initial staging due to the high metabolic activity and rapid spread characteristic of this tumour type. The modality facilitates the assessment of local invasion and distant metastases, supporting treatment decisions that often involve palliative or combined modality approaches.
PET/CT in the Detection of Recurrent and Metastatic Disease
Recurrence is a significant clinical challenge in the management of thyroid cancer. PET/CT is highly valuable in evaluating patients with biochemical evidence of recurrence but inconclusive anatomical imaging results. Elevated thyroglobulin levels following thyroidectomy and radioiodine ablation, coupled with a negative radioiodine scan, are classic indications for 18F-FDG PET/CT.
The sensitivity of PET/CT in detecting recurrent disease in such patients ranges between 70% and 90%. The technique can identify small metastases in lymph nodes, lungs, bones, and soft tissues that may evade detection by CT or MRI alone. The functional data obtained can also help distinguish between viable tumour tissue and post-therapeutic fibrosis or necrosis.
Moreover, PET/CT assists in monitoring therapeutic response and in determining the suitability of patients for targeted or systemic therapies. In cases of radioiodine-refractory disease, serial PET/CT scans can provide an objective measure of disease progression or stability under tyrosine kinase inhibitor treatment.
Prognostic Value of PET/CT in Thyroid Cancer
Beyond its diagnostic function, PET/CT holds significant prognostic value. The intensity of FDG uptake, quantified by the SUVmax, has been correlated with tumour aggressiveness, dedifferentiation, and poorer clinical outcomes. High FDG uptake in thyroid lesions is associated with increased risk of recurrence and decreased disease-free survival.
In differentiated thyroid carcinoma, patients with FDG-avid metastases typically exhibit worse prognosis than those with non-avid disease, particularly when the lesions are refractory to radioiodine therapy. Therefore, FDG-PET/CT findings can inform risk stratification and guide clinical decision-making regarding the intensity of follow-up or the initiation of systemic therapies.
In medullary and anaplastic thyroid carcinomas, where prognosis is intrinsically poor, the extent and intensity of FDG uptake may serve as an indicator of tumour burden and biological aggressiveness. PET/CT can thus aid in tailoring treatment strategies and in evaluating eligibility for clinical trials exploring novel therapeutic agents.
Limitations and Challenges
Although PET/CT provides substantial clinical benefits, it also has limitations that must be acknowledged. The physiological uptake of FDG in the thyroid gland can vary, leading to potential false positives or negatives. Benign conditions such as thyroiditis, nodular goitre, or inflammatory reactions can cause increased FDG uptake, which may mimic malignancy. Conversely, small lesions below the resolution threshold of PET/CT or lesions with low metabolic activity may be missed.
Another limitation is the variability of SUV measurements, which can be influenced by factors such as patient preparation, blood glucose levels, imaging protocols, and scanner calibration. The interpretation of PET/CT should therefore be standardised and correlated with histopathological findings whenever possible.
Additionally, the cost and limited availability of PET/CT may restrict its routine use in certain healthcare settings. The radiation exposure from combined PET and CT imaging also warrants consideration, particularly in younger patients or those requiring repeated follow-up studies.
Future Directions and Emerging Tracers
The evolving field of molecular imaging continues to refine the role of PET/CT in thyroid oncology. Research into novel radiotracers holds promise for enhanced specificity and sensitivity. Tracers such as 18F-tetrafluoroborate (18F-TFB), which targets the sodium–iodide symporter, may enable imaging of iodine-avid thyroid tissue without the need for radioiodine. Other agents, including 68Ga-labelled somatostatin analogues and 18F-DOPA, have shown promise in medullary and poorly differentiated thyroid cancers.
Artificial intelligence and quantitative imaging analysis are also expected to enhance PET/CT interpretation, enabling more precise tumour characterisation and predictive modelling. Integrating PET/CT data with genomic and molecular profiling could further advance personalised medicine in thyroid cancer management, optimising treatment selection and surveillance strategies.
Clinical Impact and Management Implications
The incorporation of PET/CT into clinical algorithms has redefined the diagnostic pathway for many patients with thyroid cancer. For individuals with elevated thyroglobulin and negative iodine scans, PET/CT has become an essential tool for locating disease recurrence and guiding targeted intervention. The ability to detect metabolically active but anatomically subtle lesions enables earlier therapeutic decisions, potentially improving outcomes.
In surgical planning, PET/CT aids in delineating the extent of disease, particularly in cases of recurrent or metastatic disease, where anatomical distortion complicates conventional imaging. Furthermore, in the setting of systemic therapy for advanced thyroid cancer, PET/CT provides a reliable means of assessing metabolic response, which often precedes structural changes detectable by CT or MRI.
Conclusion
Positron emission tomography with computed tomography represents a cornerstone of modern thyroid cancer imaging, offering a unique combination of metabolic and anatomical information. It has proven indispensable in the evaluation of recurrent and metastatic disease, particularly when conventional imaging fails to provide definitive results. By guiding diagnosis, staging, treatment planning, and prognostic assessment, PET/CT has enhanced the precision and effectiveness of thyroid cancer management.
As new tracers and quantitative imaging techniques emerge, the role of PET/CT will continue to expand, integrating functional imaging more deeply into the framework of personalised oncology. Its contribution to the early detection of aggressive disease and the optimisation of therapeutic strategies underscores its enduring value in the fight against thyroid cancer.
Disclaimer
The article “Unmasking Thyroid Cancer: The Power of PET/CT Imaging” by Open MedScience is intended for educational and informational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Readers should not rely on the content as a basis for managing any health condition without consulting a qualified healthcare professional.
While every effort has been made to ensure the accuracy and reliability of the information presented, Open MedScience makes no representations or warranties, express or implied, regarding its completeness, timeliness, or suitability for any particular purpose. Clinical decisions should always be based on the individual circumstances of each patient and guided by established medical practice and professional judgement.
Open MedScience, its authors, and affiliates accept no liability for any loss, injury, or damage arising from the use of this material. References to specific products, technologies, or imaging techniques are provided for context only and do not constitute endorsement or recommendation.
All medical images, data, and terminology discussed in this article are for illustrative purposes. Readers are encouraged to seek independent medical or scientific advice where necessary.
home » blog » nuclear medicine imaging »