Radiopharmaceuticals are used in nuclear medicine for the application of medical imaging and therapy.
An overview of radiopharmaceuticals in clinical use
Radiopharmaceuticals primarily consist of a radioisotope which is incorporated into a pharmaceutical with the ability to evaluate a disease state inside the human body. The pharmaceutical is used to transport the radioisotope to a certain organ, tissues or particular cells within the body. In some instances, radioisotopes can be used in their ionic or inert form without attachment to an organic molecule. In addition, biomolecules can be attached to radionuclides such as technetium-99m, rhenium-188, lutetium-177 and yttrium-90. When the radiopharmaceutical (imaging agent) is administered to a patient it is continually monitored by a specific imaging device such as a gamma camera for diagnosis and therapeutic purposes. These systems include SPECT and PET imaging.
Incidentally, radiopharmaceuticals possess the intrinsic property of radionuclides (radioisotopes) which is the natural process of decay. This provides routes to theranostic (therapy + diagnosis) applications. In effect, this fundamental property results from the excess energy produced due to nuclear instability since radioactive decay is the product of an unstable nucleus. In order, for the radionuclide to become more stable it must emit particles (e.g. alpha and beta) or rays such as gamma radiation from the nucleus.
Cancer theranostic treatments include 177lutetium PSMA therapy: this is a treatment for advanced prostate cancer and 177lutetium octreotate therapy for the treatment of neuroendocrine tumours (NETs) including head and neck cancers and gastrointestinal tumours.
Accordingly, radiopharmaceuticals are primarily used in the area of nuclear medicine for the application of medical imaging and/or therapy in the diagnosis and treatment of many disease states: for example, brachytherapy is used to treat prostate cancer. There are numerous radiopharmaceuticals that use technetium-99m and possess many useful properties as a gamma-emitting radionuclide in diagnostic imaging.
Nuclear medicine departments are responsible for the administration of radioisotopes and radiation in the diagnosis of the disease state and potential radiotherapy treatments. The objective of nuclear medicine is to provide information about the functioning of the human body and allow healthcare professionals to diagnosis the disease state of the patient. For example, the heart, liver, thyroid and skeleton can be imaged to detect disease.
Nuclear Medicine uses radiopharmaceuticals to gain insight into the intricate workings of the human body’s organs and biological processes. Currently, diagnostic procedures using radiotracers are routinely used in various healthcare organisations.
The advancement of radiotherapy systems incorporating proton therapy and image-guided applications are used to treat several medical oncological conditions. For example, using radiation to target cancer cells in any part of the human body.
Currently, over 40 million nuclear medicine procedures are performed every year with the demand for radioisotopes is increasing at an annual rate of 5%.
There are over 10,000 hospitals in the world use medical radioisotopes and approximately about 90% of all procedures are for diagnostic medical imaging. The most popularly used radioisotope in diagnosis is technetium-99m, with over 40 million procedures per year. This radioisotope accounts for approximately 80% of all nuclear medicine procedures.
In 2015, the global radioisotope market was worth $9.61 billion, with 80% of this figure accounting for medical radioisotopes. It is projected that the worldwide market for radioisotopes will be in the order of $17.28 billion by 2021. The North America market for diagnostic radioisotopes takes into account approximately 50% of the market share compared to Europe, which accounts for 20% of the market share.
Nuclear medicine departments began to appear in hospitals in the 1950s using iodine-131 to investigate and treat thyroid related diseases. Nuclear medicine continues to expand with the advancement of technologies, which include the hybrid scanner positron emission tomography/computed tomography (PET/CT). This was only achievable through the expansion of accelerators in radioisotope production. For example, the main radioisotope technetium-99m is better quality from nuclear reactors in comparison to the lower quality and higher cost obtained from accelerators.
The radiopharmaceuticals which are used for diagnostic purposes are short-lived radiotracers that emit gamma rays inside the body to produce a 2-D picture: alternatively by the application of tomography to generate a 3-D image. These radiotracers can be introduced into the body either by injection, inhalation or orally.
Consequently, radiation is emitted from various points within the body and gamma cameras are subsequently used for detection and to locate the disease state in order to construct a diagnostic image. The image is then further processed using a computer platform and evaluated by radiologists to locate any abnormalities.
The scanning machine – single photon emission computed tomography (SPECT) is used to diagnose and monitor a broad range of medical conditions. Another scanner used in nuclear medicine imaging is called positron emission tomography (PET) and uses radioisotopes which are produced in a cyclotron.
The majority of positron-emitting radiopharmaceuticals are injected into the bloodstream of the patient which then accumulates in the target tissue. During the decaying process, a positron is emitted which interacts with the nearby electron resulting in the simultaneous emission of two gamma rays (511 keV) in opposite directions. These gamma rays are detectable by a PET camera in order to construct the relevant images.
The most important clinical role of PET imaging is in the area of oncology and this involves the radiotracer fluorine-18 (half-life 109.8 mins). These radiotracers have proven to be beneficial in the detection and evaluation of most cancers. PET imaging is also used for cardiac and brain imaging.
In addition, PET imaging can be combined with computed X-ray tomography (CT) scans to superimpose the two images (PET + CT) to provide information on a range of diseases from dementia to cancer. The advantage of these hybrid machines is that they enable a 30% increase in diagnosis compared to using standard gamma camera techniques.
The principle behind nuclear medicine is to have a radiation source emitting inside the human body so that it can be detected outside the body by using gamma cameras. This is in contrast to external imaging techniques such as the usage of planer X-ray machines. Also, the advantage of nuclear imaging over X-ray techniques is that both the bone and soft tissue can be imaged at the same time.
Gamma imaging can be used to determine the location and concentration of the radioisotope within the body. For example, if a particular organ is not functioning correctly, this would result in the accumulation of the radiotracer. During the uptake of the radiotracer, several images can be obtained to investigate the rate of radioisotope movement, which can be correlated to the function of the organ.
Diagnostic radiopharmaceuticals
The organs in the human body are able to absorb chemicals. For example, the thyroid takes up iodine and the brain consumes glucose. These observations are the basis to the development of a range of radiopharmaceuticals which include attaching radioisotopes to biomolecules. When a radiotracer enters the body, it is incorporated into its biological pathways, metabolised, and then excreted. These radiopharmaceuticals can be used to investigate the flow of blood in the brain, amongst other organs such as the liver, lungs, heart, kidneys and including investigations into bone growth.
However, the amount of radiopharmaceutical given to a patient can range from a small dose of 5 microcuries to 35 millicuries. To put this into context, the radiation received from these dosages is about the same amount of radiation received from an X-ray study of that particular organ.
Radiopharmaceuticals used in the diagnosis of the disease state
The diagnostic radioisotope must be able to emit gamma rays and contain enough energy to escape from the body. Ideally, the rate of decay of the radioisotope must be completed quite soon after the imaging.
Technetium-99m is the most extensively used radioisotope in medicine being involved in about 80% of all nuclear medicine procedures. Technetium-99m contains the following characteristics:
- The half-life of technetium-99m is 6 hours which facilitates the investigation of metabolic processes
- The half-life is short enough to minimise the radiation dose to the patient
- The decay process involves an ‘isomeric’ process by emitting both gamma rays and low energy electrons
- No high-energy beta emission is associated with technetium-99m which results in a low radiation dose to the patient
- The low-energy gamma rays emitted from inside the body are easily detectable by a gamma camera positioned outside the body
- The chemistry of technetium allows for the incorporation of this radiotracer in a range of biomolecules
- Technetium-99m is produced using the molybdenum-99 generator, which is portable
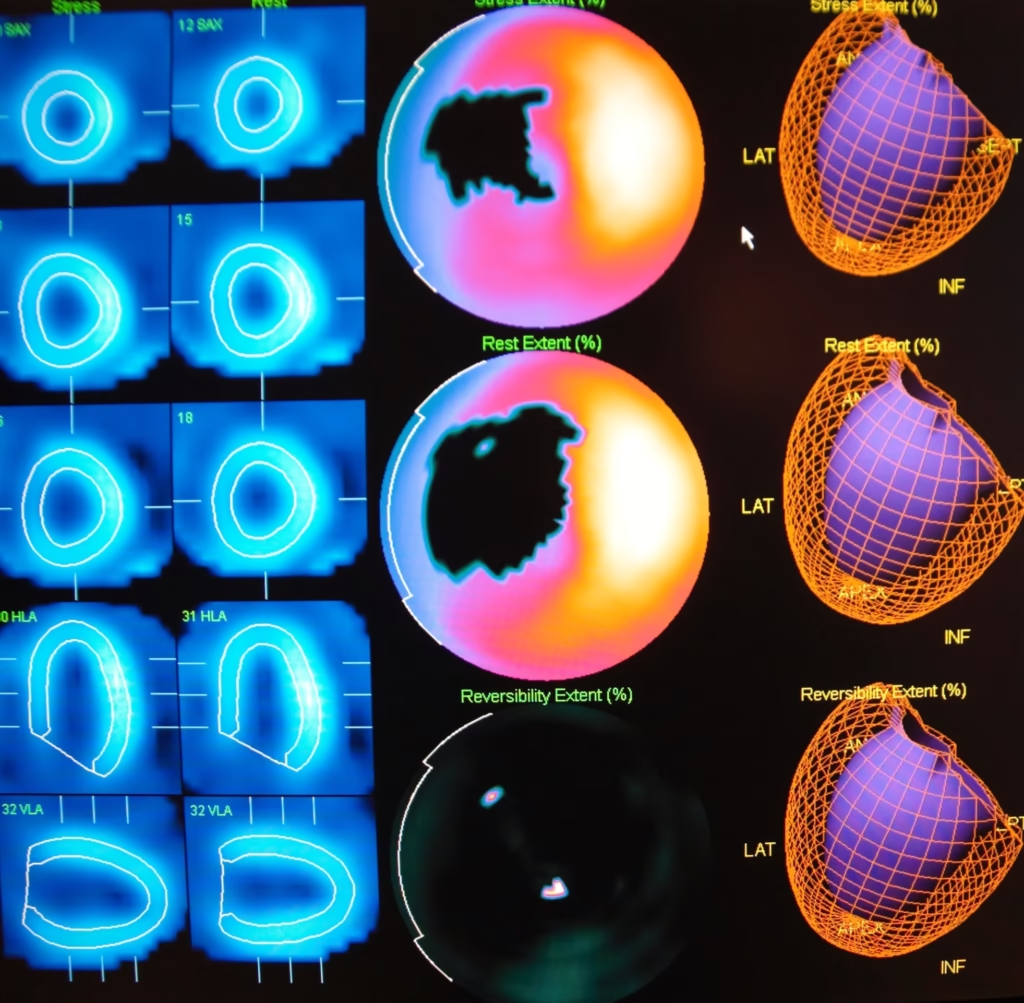
Radionuclide generators
The nuclear reactor which produces molybdenum-99 has a half-life of 66 hours and decays to technetium-99m. Drytec™ is a technetium-99m generator: each eluent of the generator should not exceed more than 0.0056 MBq of molybdenum-99 per 37 MBq of technetium-99m for a single administered dose. Also, the RadioGenix® System is a technetium-99m generator used to produce sodium pertechnetate 99mTc injection. The new TechneLite generator, which is the first technetium-99m generator in the United States containing molybdenum-99 (99Mo) which is produced from at least 95 per cent low-enriched uranium. This new type of generator aims to eliminate the use of highly enriched uranium, which is sourced from 99Mo. Technetium-99m; is used in SPECT imaging; for example, myocardial perfusion imaging to detect coronary artery disease.
In diagnostic medicine, there is a tendency towards using more cyclotron-produced isotopes such as fluorine-18 because PET and PET-CT have become more widely available. For PET imaging, the imaging agent 2-deoxy-2-[18F]fluoro-glucose with a half-life of approximately two hours is the primary radiotracer used in nuclear medicine procedures. FDG can be incorporated into the cell without being broken down and is, therefore, a good indicator of cell metabolism.
However, the procedure needs to be completed within two hours reach of a cyclotron, which limits its utility compared with 99Mo/99m generators. For PET imaging, strontium-82, which has a half-life of 25 days, can be used to generate rubidium-82, making it more accessible.
FDA approved radiopharmaceuticals
Radiopharmaceutical / Application
Carbon-11 choline
Carbon-11 choline is a PET imaging agent used to evaluate prostate cancer recurrence in patients based on elevated blood prostate-specific antigen (PSA) levels. This imaging agent is used in conjunction with bone scintigraphy, computerised tomography (CT) and/or magnetic resonance imaging to identify potential sites of prostate cancer recurrence.
Carbon-14 urea (Pytest)
This radiotracer is used to help in the diagnosis of Helicobacter pylori infection in the stomach by detecting levels of gastric urease.
Fluorine-18 florbetaben (Neuraceq™)
The PET imaging agent fluorine-18 florbetaben is used to evaluate β-amyloid neuritic plaque density in the brain to aid in the diagnosis of Alzheimer’s disease.
Fluorine-18 florbetapir (Amyvid™)
Fluorine-18 flucicovine (Axumin™)
This diagnostic PET imaging agent is used to evaluate suspected prostate cancer recurrence based on elevated blood prostate-specific antigen (PSA) levels following treatment.
Fluorine-18 sodium fluoride
Used in PET bone imaging to determine osteogenesis imperfecta (OI) known as brittle bone disease.
2-deoxy-2-[18F]fluoro-glucose (FDG)
The PET imaging agent 2-deoxy-2-[18F]fluoro-glucose is used to evaluate abnormal glucose metabolism in oncology and myocardial hibernation. Also, used to indicate abnormal glucose metabolism regions in the body, for example, epileptic seizures.
Fluorine-18 flutemetamol (Vizamyl™)
Fluorine-18 flutemetamol is a PET imaging agent used to estimate the level of β amyloid neuritic plaque density in the brain, especially for Alzheimer’s disease (AD).
Gallium-67 citrate
The half-life of Gallium-67 is 78 hours. This radioisotope is administered intravenously to patients as Ga-citrate. It is used to evaluate Hodgkin’s disease, Lymphoma and Bronchogenic carcinoma.
Gallium-68 dotatate (NETSPOT™)
Gallium-68 dotatate is a PET imaging agent used to identify somatostatin receptor-positive neuroendocrine tumours (NETs) in patients.
Indium-111 chloride
Indium-111 chloride is contained in the imaging agents OncoScint (satumomab pendetide) and ProstaScint (capromab pendetide) for in vivo diagnostic imaging. Also, used in the radiolabelling of Zevalin (ibritumomab tiuxetan).
Indium-111 pentetate
Used in cisternography imaging.
Indium-111 oxyquinoline
Used for radiolabelling autologous leukocytes to detect inflammatory processes associated with abscesses or other infections.
Indium-111 pentetreotide (Octreoscan™)
Octreoscan is used to detect primary and metastatic neuroendocrine tumours with associated somatostatin receptors.
Iodine I-123 iobenguane (AdreView™)
Iodine I-123 iobenguane is used as a diagnostic test for primary or metastatic pheochromocytoma or neuroblastoma.
Iodine-123 ioflupane (DaTscan™)
This SPECT imaging agent is used to visualise patients with suspected Parkinson's disease. It can also be used to differentiate essential tremor due to Parkinson's disease.
Iodine-123 sodium iodide capsules
These capsules are used to evaluate thyroid function.
Iodine-125 human serum albumin (Jeanatope)
Radiolabelled albumin is used to evaluate blood and plasma volume.
Iodine-125 iothalamate (Glofil-125)
Used to investigate glomerular filtration.
Iodine-131 human serum albumin (Megatope)
Megatope is used to evaluate the blood and plasma volumes, including cardiac and pulmonary blood volumes and circulation times. Also used to study protein turnover and the heart, including vessel delineation.
Iodine-131 iobenguane (AZEDRA®)
Iodine-131 obenguane is used to image locally advanced or metastatic pheochromocytoma or paraganglioma that require anticancer therapy.
Iodine-131 sodium iodide (HICON™)
Diagnostic agent iodine-131 sodium iodide is used to evaluate thyroid function such as hyperthyroidism and treatment of cancer of the thyroid.
Lutetium Lu-177 dotatate (LUTATHERA®)
Used in the treatment of somatostatin receptor-positive gastroenteropancreatic neuroendocrine tumours (GEP-NETs).
Molybdenum Mo-99 generator (UltraTechneKow V4, DRYTEC™, Technelite®, RadioGenix™ System
The molybdenum-99 generator is used to produce 99mTc-sodium pertechnetate for preparation of the radiopharmaceutical. These 99mTc-SPECT imaging agents can be used to image salivary glands and the Lacrimal Drainage System including the thyroid.
Nitrogen-13 ammonia
Nitrogen-13 ammonia is used in PET imaging to investigate the myocardium under rest of pharmacologic stress conditions. Also, to study myocardial perfusion and coronary artery disease.
Radium-223 dichloride (Xofigo®)
Radium-223 dichloride is used for the treatment of castration-resistant prostate cancer and bone metastases.
Rubidium-82 chloride (Cardiogen-82®, Ruby-Fill®)
Rubidium-82 chloride is a PET myocardial perfusion agent used to investigate myocardial infarction.
Samarium-153 lexidronam (Quadramet®)
Samarium-153 lexidronam is used for pain relief in patients suffering from osteoblastic metastatic bone lesions.
Strontium-89 chloride (Metastron™)
Used to relieve bone pain in patients suffering from skeletal metastases.
Technetium-99m bicisate (Neurolite®)
The SPECT imaging agent technetium-99m bicisate is used after a stroke diagnosis.
Technetium-99m disofenin (Hepatolite®)
Technetium-99m disofenin is used to diagnose acute cholecystitis.
Technetium-99m exametazine (Ceretec™)
Technetium-99m exametazine is used to detect changes in the regional cerebral perfusion of a stroke patient. Also, used to investigate internal abdominal infection and inflammatory bowel disease.
Technetium-99m macroaggregated albumin
Used in the evaluation of pulmonary perfusion.
Technetium-99m mebrofenin (Choletec®)
This SPECT imaging agent is used to image the liver and gallbladder.
Technetium-99m medronate (MDP-25, MDP Multidose)
A bone imaging agent to investigate osteogenesis.
Technetium-99m mertiatide (Technescan MAG3™)
This renal SPECT imaging agent is used for the diagnose of renal failure, congenital abnormalities and urinary tract obstruction.
Technetium-99m oxidronate (Technescan™, HDP)
A bone imaging agent to evaluate osteogenesis.
Technetium-99m pentetate
Technetium-99m pentetate is used in brain and kidney imaging.
Technetium-99m pyrophosphate (Technescan™, PYP™)
This SPECT imaging agent is used to investigate areas of altered osteogenesis in the bone. Also, used as a cardiac imaging agent to diagnose myocardial infarction.
Technetium-99m red blood cells (UltraTag™)
Technetium-99m can be used to radiolabel red blood cells to study blood pool imaging including cardiac and gastrointestinal bleeding.
Technetium-99m sestamibi (Cardiolite®)
Technetium-99m sestamibi is a SPECT imaging agent to investigate myocardial perfusion, especially in the detection of coronary artery disease.
Technetium-99m sodium pertechnetate
Technetium-99m sodium pertechnetate is used in SPECT imaging of the brain including thyroid and salivary gland imaging. Also, used in angiography and urinary bladder imaging.
Technetium-99m succimer
Used to evaluate renal parenchymal disorders.
Technetium-99m sulfur colloid
Technetium-99m sulfur colloid is used in SPECT imaging of the reticuloendothelial cells in the liver, spleen and bone marrow. It can also be used in oesophageal and gastroesophageal reflux scintigraphy. In addition to the detection of pulmonary aspiration of gastric contents and in the assessment of breast cancer or malignant melanoma.
Technetium-99m tetrofosmin (Myoview™)
Myoview is used in SPECT imaging of myocardial perfusion for detecting coronary artery disease by localising myocardial ischemia and infarction. Also, used in the assessment of left ventricular function.
Technetium-99m tilmanocept (Lymphoseek®)
Technetium-99m tilmanoceptis used to map the lymphatic system for tumour sites.
Thallium-201 chloride
Thallium-201 chloride is a myocardial perfusion SPECT imaging agent used for the diagnosis and localization of myocardial infarction.
Xenon-133 gas
Xenon-133 gas is used to investigate the pulmonary function and for imaging the lungs including the assessment of cerebral flow.
Yttrium-90 chloride
Zevalin is used for radioimmunotherapy procedures.
Yttrium-90 ibritumomab tiuxetan (Zevalin®)
Yttrium-90 ibritumomab tiuxetan is used for the treatment of relapsed or refractory, low-grade or follicular B-cell non-Hodgkin’s lymphoma (NHL).
Future of radiopharmaceuticals
Technetium-99m and 2-deoxy-2-[18F]fluoro-glucose (FDG) remain the workhorse radiopharmaceuticals for SPECT and PET imaging accounting for 80 per cent of all nuclear medicine procedures. However, several new radiopharmaceuticals are driving molecular imaging in the clinical setting, and these include the PET imaging agents flutemetamol and florbetapir which are used in the early diagnosis of neurodegenerative diseases such as Alzheimer’s. The technetium-99m radiopharmaceutical ubiquicidin is used to detect bacterial infections on the sites of orthopaedic implants extending to 68Ga-NOTA-ubiquicidin for PET imaging of infection.
Incidentally, there are some new cardiovascular PET imaging applications towards myocardial perfusion imaging such as ammonia-13 and flurpiridaz. Also, the recent approval of RUBY-FILL (generator containing strontium-82) and the elution system to produce CardioGen-82: these systems lead to the formation of rubidium-82. This radionuclide is used in the clinical setting in the form of 82RbCl to mimic the potassium ions (K+) for the imaging of myocardial perfusion. However, due to its short half-life of 1.3 min rubidium-82 poses several challenges for routine applications. However, the benefit of using rubidium-82 is that it provides a higher resolution PET scan in comparison to the SPECT tracer 99mTc-MIBI.
A novel class of PET radiopharmaceuticals using 68Ga-FAPI was able to identify at least 30 types of malignant tumours. This radiotracer targets cancer-associated fibroblasts, which can contribute up to 90 per cent of a tumour’s mass.
Advancements of radiopharmaceuticals in oncology have included axumin (18F-fluciclovine) used for the detection of recurrent prostate cancer. The FDA has given approval for the PET imaging agent 68Ga-dotatate known as NETSPOT™ to locate somostatin receptor positive neuroendocrine tumours in both adult and paediatric patients.
Subsequently, the PET radiotracer, 18F-TZ3504 has been used to image neuroinflammation due to multiple sclerosis by quantitative assessment of S1P1 expression in the body.
The generation of technetium-99m introduces problems to the SPECT-CT market and therefore requires an alternative approach. The non-reactor manufacture of technetium-99m in the future will allow SPECT radiopharmaceuticals to effectively compete with cardiac PET.
Theranostics is a hot topic in the radiopharmaceutical market, especially due to the latest FDA approval of lutetium-177 dotatate (lutathera) to image and treat gastroenteropancreatic neuroendocrine tumours. This theranostic agent is a combination of a diagnostic agent and a therapeutic agent, such as 68Ga- and 177Lu-dotatate.
Another promising prostate cancer theranostic pairing are the bombesin analogues, 68Ga and 177Lu-RM2. Also, 86Y (β+) forms a theranostic isotopic pair with the pure β− emitter 90Y. Currently, the PET radiometal 44Sc which can be obtained from a 44Ti/44Sc generator possesses similar decay characteristics to 68Ga but a longer half-life of 3.97 hours. It has been demonstrated that 44Sc-DOTATOC is compatible with standard radiolabelling techniques and produces a comparable imaging quality to that of the 68Ga-DOTATOC.
In addition, the calcium mimic, Xofigo (radium-223) was approved by the FDA in 2013 for the treatment of bone metastases in prostate cancer. However, a future radiopharmaceutical [225Ac]-FPI-1434 is in development to target solid tumours, which include non-small cell lung, prostate and breast cancers.
Interestingly, pentixafor can be labelled with 99mTc for SPECT imaging and 68Ga for PET imaging. This imaging agent binds to CXC chemokine type 4 receptors which are up-regulated in several cancers, for example, multiple myeloma.
In January 2019, the diagnostic radiopharmaceutical, 64Cu-dotatate, received fast track designation from the FDA. 64Cu-dotatate is a PET diagnostic agent developed to detect neuroendocrine tumours. Also, the radiotherapy drug Azedra (iobenguane iodine-131) is used to treat rare tumours of the adrenal gland called pheochromocytomas.
On the SPECT horizon, the radiotracer AdreView (iobenguane iodine-123) is the first imaging agent to establish a link between nerve function in the heart and the patient’s mortality risk. Also, AdreView has been given FDA approval for the scintigraphic assessment of myocardial sympathetic innervation, known as cardiac nerve activity.
Currently, a new generation of hybrid scanners is entering the clinical setting which combines PET and MRI imaging. This will allow for the development of a new class of imaging agents that incorporate the radionuclide into superparamagnetic iron oxide nanoparticles (SPION) to allow hybrids of PET/MRI and SPECT/MRI.
An alternative approach is to use paramagnetic manganese instead of the MRI contrast agents based on gadolinium. It can be envisaged that the use of paramagnetic manganese and the PET radiometal 52gMn can be used to produce hybrid PET/MRI images. These scanners will enable radiopharmaceuticals to be developed to evaluate traumatic brain injury and post-traumatic stress disorder amongst other disease states.
Disclaimer
Medical and Scientific Information
The content presented in this article, Radiopharmaceuticals Used in Nuclear Medicine by Open Medscience, is intended for informational and educational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of a qualified healthcare professional or nuclear medicine specialist with any questions you may have regarding a medical condition or treatment involving radiopharmaceuticals or radiation-based diagnostics.
No Clinical or Therapeutic Endorsement
Open Medscience does not endorse, recommend, or guarantee the safety, efficacy, or suitability of any specific radiopharmaceutical, imaging technique, or therapeutic protocol mentioned in this article. The inclusion of proprietary names, commercial systems, or specific radiotracers is solely for descriptive and illustrative purposes. Clinical decisions must be made by qualified practitioners based on individual patient assessments, institutional guidelines, and the most current evidence-based standards.
Use of Radioactive Materials
The preparation, handling, administration, and disposal of radiopharmaceuticals involve inherent risks and must be performed in accordance with national and local regulations, radiation protection standards, and under the supervision of authorised personnel within a licensed nuclear medicine facility. This article does not provide instruction or guidance on compliance with such regulations.
Regulatory and Safety Considerations
Many radiopharmaceuticals described herein may be subject to approval and regulation by relevant national or international authorities, including the Medicines and Healthcare products Regulatory Agency (MHRA), the U.S. Food and Drug Administration (FDA), or the European Medicines Agency (EMA). Users of this information are responsible for ensuring compliance with applicable laws, guidance documents, and institutional protocols.
Liability Limitation
Open Medscience and its contributors disclaim all liability for any loss, injury, or damage suffered as a result of the use, misuse, or interpretation of the information contained in this publication. This includes but is not limited to any reliance placed on such information by healthcare professionals, researchers, or members of the public.
Future Developments and Accuracy
The field of radiopharmaceuticals is rapidly evolving. While Open Medscience aims to provide accurate and up-to-date information, no guarantee is made that the content reflects the latest clinical developments, research, or changes in regulatory status. Readers are encouraged to consult current literature and professional sources for the most recent updates.
Disclaimer
Medical and Scientific Information
The content provided in Radiopharmaceuticals Used in Nuclear Medicine by Open Medscience is intended solely for informational and educational purposes. It is not designed to replace professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider or nuclear medicine specialist for advice concerning any medical condition or decisions involving radiopharmaceuticals or radiation-based diagnostics.
Clinical Use and Endorsement
Open Medscience does not endorse, recommend, or warrant the efficacy, safety, or appropriateness of any specific radiopharmaceutical, imaging technique, or treatment method referenced in this article. Mentions of commercial names, branded systems, or particular tracers are for illustrative purposes only. All clinical applications must be assessed and determined by qualified professionals based on individual patient needs, current clinical guidelines, and established standards of care.
Radiation Safety and Handling
The preparation, use, and disposal of radiopharmaceuticals must comply with relevant national and local legislation, including radiation safety protocols. Such activities should only be undertaken by authorised personnel operating within licensed facilities. This publication does not serve as a guide to regulatory compliance or safety procedures.
Regulatory Oversight
Some of the substances and technologies mentioned may be regulated by authorities such as the Medicines and Healthcare products Regulatory Agency (MHRA), the U.S. Food and Drug Administration (FDA), or the European Medicines Agency (EMA). It is the responsibility of practitioners and institutions to ensure all use is in accordance with applicable legal and regulatory frameworks.
Liability and Responsibility
Open Medscience and its contributors accept no liability for any outcome arising from the use or interpretation of the information contained in this article. This includes, but is not limited to, medical, legal, or operational consequences resulting from reliance on the material by clinicians, researchers, or members of the public.
Scientific Updates and Limitations
The field of nuclear medicine is continually advancing. While efforts are made to ensure the accuracy and relevance of the information provided, Open Medscience cannot guarantee that all content reflects the latest research, technologies, or regulatory changes. Readers are encouraged to consult up-to-date, peer-reviewed sources and professional bodies for the latest guidance.
home » blog » nuclear medicine imaging »